- Submissions

Full Text
Research in Pediatrics & Neonatology
Pediatric Outpatient Parenteral Antimicrobial Therapy (OPAT) Patient Experiences, Length of Stay and Cost- Effectiveness, One-Year Experience in a Tertiary Hospital, Riyadh, Saudi Arabia
Rana Hassan Almaghrabi1, Lubna Abdulrahman Elshaib2*, Nourah Hussain Alhussain and Ibrahim Bin Hussain
1Department of paediatrics, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
2Pediatric antimicrobial Stewardship and OPAT Unit, Department of paediatrics, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
*Corresponding author: Lubna Abdulrahman Elshaib, Pediatric antimicrobial Stewardship and OPAT Unit Department of paediatrics, Prince Sultan Military Medical City, Riyadh, Saudi Arabia
Submission: June 01, 2021; Published: June 28, 2021

ISSN: 2577-9200 Volume5 Issue5
Abstract
Background: The outpatient parenteral antibiotic therapy (OPAT) service is becoming increasingly popular worldwide due to its efficacy, safety and cost effectiveness. It is considered as an alternative to hospital treatment. However, these services have not yet become an integral part of the health care system in Saudi Arabia. The present study is intended to assess healthcare employee experience, safety, cost effectiveness, patient satisfaction in OPAT service in pediatric patients at tertiary care hospital, Riyadh.
Methods: In this retrospective study, 19 patients aged between ≥3 months to <14 years, stable and ready for discharge but kept only for completion of IV antibiotics were recruited between the period of Nov. 2018 to Oct. 2019. Data on demographic characteristics, antibiotics used, improvement rate, patient satisfaction and cost effectiveness were collected.
Results: Clinical outcomes and patient’s experience in pediatric OPAT service reported 95% health improvement rate with 100% patients and parents’ satisfaction. Ceftriaxone is the most commonly (70%) prescribed antibiotic followed by Tazocin. The psychological status, family convenient and medical care were reported better in OPAT as compared to in hospital stay. We have saved 61% bed days through the establishment of OPAT service. In addition, OPAT service-related complication, readmission, and failure rate were minimal in our study. The cost of all the patients participating in OPAT care is 46,125 SAR as compared to the in hospital estimated cost of SAR 707,400. Thus, we saved 93.48% of the overall estimated inpatient stay cost.
Conclusions: Our study demonstrates that OPAT is reliable and cost-effective service. It can reduce the direct costs of non-life-threatening infections compared to completing the course as an in-patient case. We have saved 93.48% of the overall estimated hospital expense through establishing OPAT service.
Keywords: OPAT; Pediatrics; IV antibiotic; Cost-effective; Non-life threatening; Patient Satisfaction; Psychological status
Introduction
Outpatient parenteral antibiotic therapy (OPAT) programs are applied for non-lifethreatening infections in stable and well patients. It is used as a hospital alternative to inpatient care for prolonged stays where facilities permit. Hospitalization has a great impact on the healthcare expenditure of any country particularly if the stay is prolonged because of Intravenous Antibiotics (IVABs). It leads to a significant increase in nosocomial infection and a high rate of medication error. Pediatric OPAT has many advantages in comparison to inpatient treatment, including less interruptions in family and school life, improved psychological comfort, decreased risk of nosocomial comfort [1-5]. It can be used in patients with a range of infections, but most often for complicated infections of the soft tissue, infections of the bones (osteomyelitis), heart infections (endocarditis), joints and bacteremia [6]. The acceptability of OPAT increased tremendously and became global treatment modality because of the cost effectiveness, alternative to in-hospital therapy with the better quality through reduced patient stay.
The British Society of Antimicrobial Chemotherapy (BSAC) guidelines for pediatrics OPAT service recommended the management of children with complex infections requiring prolonged courses of IVABs [7]. It is accepted as a standard practice worldwide including the USA, Australia [8]. In the USA alone, an estimated quarter of a million patients receive IV antibiotics on an outpatient basis each year. The OPAT service tended to deliver through one or more of three models which includes ‘infusion center’ model, where patients attend an OPAT facility daily, a nurse visiting the patients at home and the model of self-administration, where the patient or a caregiver is trained to administer therapy with regular OPAT service supervision [9-11]. It is therefore important to understand patient experiences of different OPAT services to inform commissioning decisions. The advancement of OPAT programs represents significant developments in clinical, pharmaceutical, and technological research, leading to the development of new drugs and IV infusion devices that promote outpatient care delivery and improve patient satisfaction. To allow the complete safe and effective treatment to the patients in the outpatient sittings and to avoid the potential inconvenience, complications, expenses of hospitalization, and to maintain a normal of lifestyle, we need to address some common problem such as prolonged length of stay which can increase hospital cost, miss-utilization of hospital beds, significant increase in nosocomial infection, high rate of medication errors, disruption of family environment. Hence, present study was designed to evaluate the safety, cost effectiveness, patient’s satisfaction etc. under OPAT service at pediatrics department of PSMMC, Riyadh, KSA.
Methods
The present OPAT service was launched as an infusion room with a single bed in the medical unit serving pediatric patients for a period of Nov. 2018 to Oct. 2019 at Prince Sultan Military Medical City (PSMMC), Riyadh, K.S.A. The ethical clearance was obtained from Institutional Review board, PSMMC, Riyadh prior to conducting this study. The patients were recruited after following the strict inclusion and exclusion criteria. The age of subject lying between > 3 months and <14 years were included. Only those patients who were found negative for culture test, clinically stable and ready for discharge but kept only for completion of IV antibiotics course were included. Pediatric patients who have no further predictable need for hospital-based care apart from the administration of antimicrobial therapy and their caregiver capable to come to hospital every day to receive the medications. In the current analysis, patients < 3 months and > 14 years of age and medically unstable were excluded. Also, cooperative families with convenient transport and agreed to the OPAT service were preferred. The working telephone number were exchanged for the hassle-free communication. The patients who are eligible and met the criteria of recruitment was referred to OPAT team which includes house staff doctors, nurses and pharmacist. The written consent was taken from parent/legal guardian prior to the inclusion of subjects in the study. The study population was characterized in terms of age, length of hospital stays, antimicrobial agents used, and clinical indication for OPAT.
The frequency of antibiotics for the OPAT service was not more than 3 times a day, preferably once or twice per day. In courses shorter than 14 days, IV cannula was used while PICC (peripherally inserted central catheter) line was used for longer courses or for extremely challenging patients. Patients were given clear instructions by the doctors about the care of the IV cannula or PICC line. At the end of the course, the IV cannula or PICC line must be removed in the infusion room. The interventional data were collected using a retrospective chart review on monthly basis by selecting the entire patient. The data were then submitted to CQI&PS. In the present study, two economic studies, for short and long-term IVA treatments, were carried out. The impact of treatment on the health-related quality of life of the patients, bed days saved by OPAT, cost effectiveness and the length of stay were assessed.
Statistical analysis
Qualitative and quantitative methods were used to analyze data generated in the present study. The data were analyzed using Excel tool. Further, the data were sorted based on the similarity and groups. The grouped data were analyzed by using bar diagram/ histogram, pia chart, 2D line diagram etc. Data were also presented in table format using word pad 2010 version.
Results
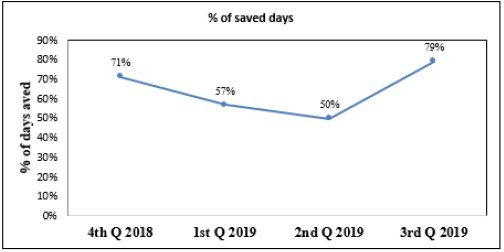
In this present OPAT service, 19 patients were included for the shortest duration of 3 days and longest duration of 150 days. The most common diagnosis performed in our OPAT service is neurological followed osteoarticular, respiratory, sepsis accompanied by UTI. Furthermore, clinical findings and patient experience in pediatric OPAT have demonstrated a 95% improvement in patients. The satisfaction data analysis revealed 100% patient’s satisfaction with the services provided under OPAT (Table 1). The well psychological status, family convenient and medical care were reported in 100% of the patients under OPAT service while 60% in patients care. However, time saving and medical related parameters were also better in 90% of the patients under OPAT service as compared to in hospital service (Figure 1). Ceftrixone was given in 70% of patients, followed by Tazocin (Figure 2). The data for bed days saved through OPAT service were stratified under different kind’s infection groups. We found the highest number of patients are fallen under neurological disorder followed by osteoarticular and respiratory diseases (Figure 3). The cost of all the patients involved in OPAT service is SAR 461,25 compared with SAR 707,400 an estimated cost for in-hospital treatment. Hence, OPAT cost is just only 6.52 % of the inpatient stay cost. This intervention saved the hospital’s 93.48% of the stay cost (Figure 4). The data for cost saving per patient in Saudi Riyal is shown in Figure 5. When the data were analyzed for percentage of days saved in the different quarter of study period through OPAT service, 79% of the days saved in third quarter followed by fourth quarter (Figure 6). In total, we have saved a total number of 393 (61%) bed days by the establishment of OPAT service.
Table 1: Clinical outcomes and patients experience in pediatric OPAT service (N=19).
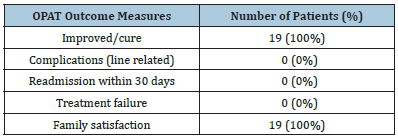
Figure 1: Shows wellbeing of psychological status, family convenient, time saving, medication related issue and medical care under OPAT as compared to inpatients services. Y axis: Percentage value
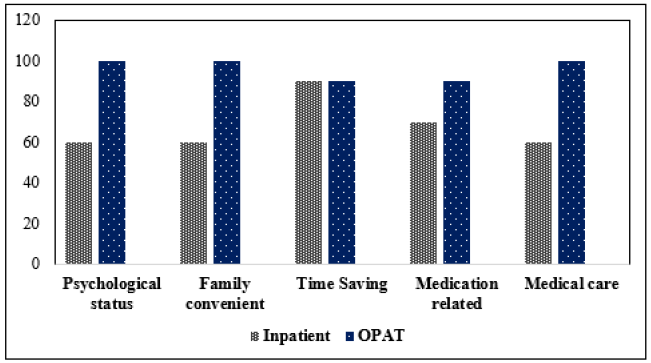
Figure 2:Shows different kind of antibiotic used for pediatric teartment under OPAT service. Y axis: Number of patients
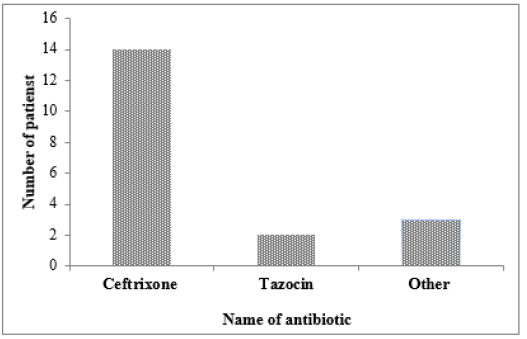
Figure 3:Shows number of bed days saved according to infection groups under OPAT service. Y axis: Number of bed days saved
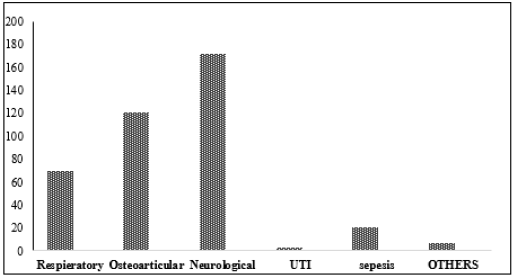
Figure 4: Shows overall cost saving (SR) under OPAT service as compared to in patients.
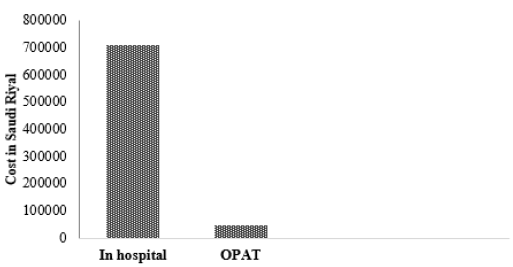
Figure 5:Shows direct cost saving per patient (SAR) under OPAT service. Y axis: Saudi Arab Riyal (SAR) X axis: patients
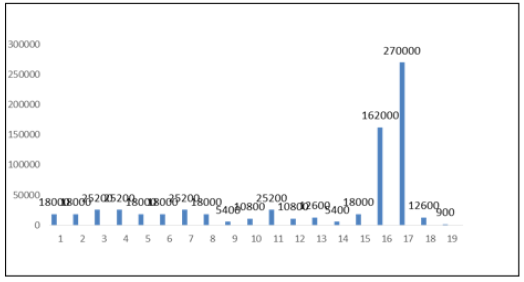
Figure 6:Shows percentage of days saved in the different quarter of study period under OPAT service. X axis: Time period (quartile)
Discussion
The roots of OPAT service, originally for children with cystic fibrosis, can be traced back to the 1970s, however, recent advances in OPAT have focused on adult practice [12]. To date, only a few studies have been carried out to investigate the safety and effectiveness of OPAT in children, with the majority focusing on outcomes linked to OPAT services in adults [2]. Previous studies have shown adverse events such as health care associated infections (HCAIs), adverse effect of drug, and surgical complications etc in hospitalized patients. The US Center for Disease Control and Prevention (CDC) states that approximately 1.7 million occurrences of HCAIs annually while being treated for other health conditions, resulting in more than 98,000 patient’s mortalities annually [13]. In contrary to this, managing children at home has clear advantages in terms of reductions in HCAIs, minimal operational costs, high satisfaction of parents and patients, psychological well-being, return to school/employment etc. The serious financial constraints faced by hospitals urgently need OPAT service, an appealing choice to minimize operating costs by reducing patient stays inside the hospital. The recent BSAC recommendations for pediatric OPAT service, along with previous research on child stress management because of the extended courses of IV antibiotics in complex infections cases drew the attention towards OPAT service, globally [7,13,14].
In our governmental hospital, increased admission load, bed shortage, safe discharge of patients suggests us to adopt OPAT service for the safe and efficacious in carefully selected patients. Previous studies also suggesting this type of care is being increasingly utilized for antimicrobial administration in the home [15-17]. Our findings revealed 100% patient’s satisfaction without any complications, treatment failure and readmission within 30 days after receiving OPAT service (Table 1). The wellbeing of psychological status, family convenient and medical care in OPAT were reported in 100% of the patients as compared to 60% of inhospital cases. In contrast to this, medication related issue of the patients was comparatively higher in OPAT. Also, we did not observe any difference in time saving between OPAT and in-hospital service (Figure 1). The high success rate of OPAT in our study may suggest its use for children with a wide spectrum of clinical diagnoses. For infants, OPAT is especially beneficial to minimize the negative psychological effect of hospitalization and also to uninterrupted family life [18-20]. Given the option, most parents choose to be at home rather than have their child in the hospital [21]. Children can also attend school or nursery based on clinical response, avoiding educational interruptions, and parents can still attend work.
In our study, Ceftriaxone (70%), is the first choice of antibiotics for pediatric treatment in OPAT followed by Tazocin (Figure 2). The highest number of bed days were saved for neurological disorder followed by osteoarticular. It is also considered as an option in the treatment of patients with MSSA bacteremia compared to oxacillin or cefazolin under OPAT [22]. Madigan et al. [23] reported positive culture or serology result in 86 (68%) OPAT courses and they have given ceftriaxone in 17% patients while, cefazolin in 16% and cefepime in 13%. Our findings are corroborated with Hodgson et al. [8] who prescribed ceftriaxone in 28% of the patients followed by gentamicin in 19% of pediatrics OPAT service in Australian population.
In our study, the calculated in-patient cost was SAR 707,400 which included bed cost, nursing cost, physicians visit cost, administration of antibiotics, and disposables however, in OPAT the cost of all the patients was only 46,125 SAR which also included the cost of nurse visits, physician visits, disposables, and antibiotics (Figure 4). Almost, 93.48% of the overall projected hospital expense was saved by implanting the OPAT service. In addition, we have also analyzed data for cost saving per patient (Figure 5) as well as quarterly saving (Figure 6). Jali et al. [24] have reported the cost of all patients participating in OPAT care was $6706 as compared to $68,090 an estimated cost for in-hospital treatment. They reported an average OPAT cost is only 9.84% of the inpatient stay cost for the antibiotics. This intervention saved the hospital 90.16% of the cost. Similar to us, a home intravenous antibiotic in a tertiary care hospital in Saudi Arabia have also saved about 47% of the inpatients cost (1). Hodgson et al. [8] also reported OPAT is a safe and effective way of providing antibiotics to children. They also tried to measure their workload and determine the appropriateness of their prescribing IVAB over a 12-month span. They handled 251 infectious episodes with IVABs staying for a median of 7 days. In their study, OPAT had replaced inpatient treatment for 3084 days, combined with a remarkable cost saving of $A1.82 million in a single year.
A Central Line-Associated Bloodstream Infection (CLABSI) contributes to extended hospital stays and increases the cost of health care and mortality. An estimated 250,000 bloodstream infections occur every year [25]. It is important to ensure that children receive the same quality of care at home as they will receive at the hospital, and only 11% of adverse effect complication rates are recorded and only 4% of patients seek unplanned readmission. It includes essential training to facilitate drug administration in a safe and effective manner with minimal complications [16]. Report showed that preventing even 10% of readmissions might save $1 billion for Medicare [26]. We have also analyzed our data for the percentage of days saved in the different quarters of study period and found 79% of the days saved in third quarter followed by fourth quarter (Figure 6). In total, we have saved 61% bed days by the establishment of OPAT service in our hospital. Our finding is corroborated with previous study conducted in Saudi hospital and they have saved 47.67% days in the period of 1 year through establishing OPAT [24]. This service does not only benefit the hospital, but it also provides patients with assistance, as they can return to work and continue their antibiotic therapy. Numerous clinical studies have demonstrated that the administration of IV (intravenous) antibiotics on an outpatient basis to selected patients is safe, cost effective, practical, and can reduce overall health care expenditure [17, 27-30]. Our findings are in line with above results reflecting the success of OPAT in Saudi Arabia. There is a growing interest in OPAT from the last century; OPAT has become a global treatment modality [31] in different areas of the world [32]. OPAT allows patients to have a more normal life, saves money, appears to be safe [33] and leads to an increase in the available bed days in the hospitals [34]. The model for self-administration is significantly lower in cost than the other models because of savings in healthcare personnel and overhead expenses. Beside this, there are certain disadvantages include poor medical knowledge of patients, poor medical supervision and availability of medical equipment, diagnosis of only medically stable cases, inpatient care, treatment of only limited infection such as skin and soft tissue infection, osteomyelitis, septic arthritis, wound infection etc. [35].
Limitations
In our study, the risk of nosocomial infection and the chances of contracting an antimicrobial resistant organism, if any, were not evaluated. Hence, multicentric studies with a larger sample size, risk management of nosocomial infection and the likelihood of acquiring an antimicrobial resistant organism are required to reinforce the results of our study.
Conclusion
Our study demonstrates that OPAT is reliable and cost-effective service. It can reduce the direct costs of non-life-threatening infections compared to completing the same course as an in-patient case. We reported 93.48% of the overall hospital expense saving by OPAT service. We suggest OPAT program as an alternative to inhospital management and could be used more often as part of Saudi Arabia’s health care system.
References
- Baharoon S, Almodaimeg H, Watban HA, Jahdali HA, Alenazi T, et al. (2011) Home intravenous antibiotics in a tertiary care hospital in Saudi Arabia. Ann Saudi Med 31(5): 457-461.
- Tice AD, Rehm SJ, Dalovisio JR, Bradley JS, Martinelli LP, et al. (2004) Practice guidelines for outpatient parenteral antimicrobial therapy. Clin Infect Dis 38(12): 1651-1671.
- Seaton RA, Nathwani D (2000) Outpatient and home parenteral antibiotic therapy (OHPAT) in the UK: Survey of infection specialists' experience and views. Clin Microbiol Infect 6(7): 387-390.
- Kayley J, Berendt A, Snelling M, Moore H, Hamilton HC, et al. (1996) Safe intravenous antibiotic therapy at home: Experience of a UK based programme. J Antimicrob Chemother 37(5): 1023-1029.
- Sriskandarajah S, Ritchie B, Sluggett JK, Hobbs JG, Reynolds KJ (2020) Safety of nurse and self-administered paediatric outpatient parenteral antimicrobial therapy. Antibiotics (Basel) 9(11): 761.
- Brugha RE, Abrahamson E (2012) Ambulatory intravenous antibiotic therapy for children with preseptal cellulitis. Pediatr Emerg Care 28(3): 226-228.
- Patel S, Abrahamson E, Goldring S, Green H, Wickens H, et al. (2015) Good practice recommendations for paediatric outpatient parenteral antibiotic therapy (p-OPAT) in the UK: A consensus statement. J Antimicrob Chemother 70(2): 360-373.
- Hodgson KA, Huynh J, Ibrahim LF, Sacks B, Golshevsky D, et al. (2016) The use, appropriateness and outcomes of outpatient parenteral antimicrobial therapy. Arch Dis Child 101(10): 886-893.
- Gauthier M, Chevalier I, Sterescu A, Bergeron S, Brunet S, et al. (2004) Treatment of urinary tract infections among febrile young children with daily intravenous antibiotic therapy at a day treatment center. Pediatrics 114(4): e469-e76.
- Reid S, Bonadio W (2006) Feasibility of short-term outpatient intravenous antibiotic therapy for the management of infectious conditions in pediatric patients. Am J Emerg Med 24(7): 839-842.
- Chapman ALN, Patel S, Horner C, Green H, Guleri A, et al. (2019) Updated good practice recommendations for outpatient parenteral antimicrobial therapy (OPAT) in adults and children in the UK. JAC-Antimicrobial Resistance 1(2): 1-18.
- Rucker RW, Harrison GM (1974) Outpatient intravenous medications in the management of cystic fibrosis. Pediatrics 54(3): 358-360.
- Haque M, Sartelli M, McKimm J, Bakar MA (2018) Health care-associated infections-an overview. Infect Drug Resist 11: 2321-2333.
- Al-Tawfiq JA, Amalraj A, Memish ZA (2013) Reduction and surveillance of device-associated infections in adult intensive care units at a Saudi Arabian hospital, 2004-2011. Int J Infect Dis 17(12): e1207-e1211.
- Matthews PC, Conlon CP, Berendt AR, Kayley J, Jefferies L, et al. (2007) Outpatient parenteral antimicrobial therapy (OPAT): Is it safe for selected patients to self-administer at home? a retrospective analysis of a large cohort over 13 years. J Antimicrob Chemother 60(2): 356-362.
- Subedi S, Looke DF, McDougall DA, Sehu MM, Playford EG (2015) Supervised self-administration of outpatient parenteral antibiotic therapy: A report from a large tertiary hospital in Australia. Int J Infect Dis 30: 161-165.
- Barr DA, Semple L, Seaton RA (2012) Outpatient parenteral antimicrobial therapy (OPAT) in a teaching hospital-based practice: A retrospective cohort study describing experience and evolution over 10 years. Int J Antimicrob Agents 39(5): 407-413.
- Maraqa NF, Rathore MH (2010) Pediatric outpatient parenteral antimicrobial therapy: An update. Adv Pediatr 57(1): 219-245.
- Moore D, Bortolussi R (2011) Home intravenous therapy: Accessibility for Canadian children and youth. Paediatr Child Health 16(2): 105-114.
- Sartain SA, Maxwell MJ, Todd PJ (2001) Users’ views on hospital and home care for acute illness in childhood. Health Soc Care Community 9(2): 108-117.
- Manji A, Beyene J, Dupuis LL, Phillips R, Lehrnbecher T, et al. (2012) Outpatient and oral antibiotic management of low-risk febrile neutropenia are effective in children-a systematic review of prospective trials. Support Care Cancer 20(6): 1135-1145.
- Hamad Y, Connor L, Bailey TC, George IA (2020) Outcomes of outpatient parenteral antimicrobial therapy with ceftriaxone for methicillin-susceptible staphylococcus aureus bloodstream infections-a single-center observational study. Open Forum Infect Dis 7(9): ofaa341.
- Madigan T, Banerjee R (2013) Characteristics and outcomes of outpatient parenteral antimicrobial therapy at an academic children's hospital. Pediatr Infect Dis J 32(4): 346-349.
- Jali I, Bajnaid N (2016) Cost effectiveness of outpatient parenteral antibiotic therapy. Global Advanced Research Journal of Medicine and Medical Sciences 5(7): 203-207.
- Haddadin Y, Annamaraju P, Regunath H (2020) Central line associated blood stream infections, StatPearls publishing, USA.
- Medicare Payment Advisory Commission (2014) Report to the Congress: Promoting greater efficiency in Medicare, Medicare Payment Advisory Commission, USA.
- Poretz DM (1998) Evolution of outpatient parenteral antibiotic therapy. Infect Dis Clin North Am 12(4): 827-834.
- Chapman AL, Dixon S, Andrews D, Lillie PJ, Bazaz R, et al. (2009) Clinical efficacy and cost-effectiveness of outpatient parenteral antibiotic therapy (OPAT): A UK perspective. J Antimicrob Chemother 64(6): 1316-1324.
- Wai AO, Frighetto L, Marra CA, Chan E, Jewesson PJ (2000) Cost analysis of an adult outpatient parenteral antibiotic therapy (OPAT) programme. A Canadian teaching hospital and ministry of health perspective. Pharmacoeconomics 18(5): 451-457.
- Chary A, Tice AD, Martinelli LP, Liedtke LA, Plantenga MS, et al. (2006) Experience of infectious diseases consultants with outpatient parenteral antimicrobial therapy: Results of an emerging infections network survey. Clin Infect Dis 43(10): 1290-1295.
- MacKenzie M, Rae N, Nathwani D (2014) Outcomes from global adult outpatient parenteral antimicrobial therapy programmes: A review of the last decade. Int J Antimicrob Agents 43(1): 7-16.
- Esposito S, Noviello S, Leone S, Tice A, Seibold G (2004) Outpatient parenteral antibiotic therapy (OPAT) in different countries: A comparison. Int J Antimicrob Agents 24(5): 473-478.
- Antoniskis A, Anderson BC, Van Volkinburg EJ, Jackson JM, Gilbert DN (1978) Feasibility of outpatient self-administration of parenteral antibiotics. West J Med 128(3): 203-206.
- Swenson JP (1981) Training patients to administer intravenous antibiotics at home. Am J Hosp Pharm 38(10): 1480-1483.
- Tice AD (1995) Experience with a physician-directed, clinic-based program for outpatient parenteral antibiotic therapy in the USA. Eur J Clin Microbiol Infect Dis 14(7): 655-661.
© 2021 Lubna Abdulrahman Elshaib. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






