- Submissions

Full Text
Research in Pediatrics & Neonatology
Laparoscopic Nissen Fundoplication and Gastrostomy in Children - Our Experience
Anis Akhtarkhavari1, Lakshmi Sundararajan1*, Srinivas Shankaranarayanan2 and Viswanathan V3
1Department of Pediatric Surgery, Childs Trust Medical Research Foundation, Kanchi Kamakoti Childs Trust Hospital, India
2Department of Pediatric Gastroenterologist, Childs Trust Medical Research Foundation, Kanchi Kamakoti Childs Trust Hospital, India
3Paediatric Neurologist, VJ Clinic, India
*Corresponding author: Lakshmi Sundararajan, Department of Pediatric Surgery, Childs Trust Medical Research Foundation, Kanchi Kamakoti Childs trust hospital, Chennai, India
Submission: May 03, 2021; Published: May 21, 2021

ISSN: 2577-9200 Volume5 Issue5
Abstract
Aim: Laparoscopic approach to fundoplication for gastroesophageal reflux disease has become an established procedure in infants and children. This study aims to evaluate our experience with laparoscopic Nissen fundoplication and gastrostomy in a developing country.
Methods: We reviewed the records of 13 consecutive laparoscopic Nissen fundoplication with or without gastrostomy performed by a single surgeon at our institution. All patients had documented gastroesophageal reflux disease with ages ranging from 8 months to 15.2 years. All were followed clinically for the presence of early or late postoperative complications including recurrent reflux.
Results: In 10 of the 13 children, Nissen fundoplication was completed laparoscopically, 3 needed conversion to open technique. An average operative time of 182 minutes was noted with a decreasing trend over time. No postoperative complications like need for postoperative ventilation, bowel disturbances and pulmonary complications were seen. Long term follow up showed all patients thriving, without need for antacid medication. Encouragingly, high parental satisfaction was seen both for the procedure as well as for results of surgery.
Conclusion: Laparoscopic Nissen fundoplication is an effective treatment option for children in our hands. There is high parental satisfaction with the procedure.
Keywords: Gastroesophageal reflux disease; Laparoscopy; Fundoplication; Gastrostomy
Introduction
Fundoplication for GERD is indicated in case of failure of medical management, recurrent aspirations and life threatening episodes, complications like reflux stricture and failure to thrive1-3. Laparoscopic approach to this surgery has contributed to an increase in the acceptance of anti-reflux surgery. Though such procedures are very common in the western world, it is still an underserviced area in developing countries with constrained resources. There remains great anxiety in the minds of parents in subjecting neurologically impaired children to painful surgery. This report describes our early experience with laparoscopic Nissen fundoplication with/without gastrostomy in children.
Methods
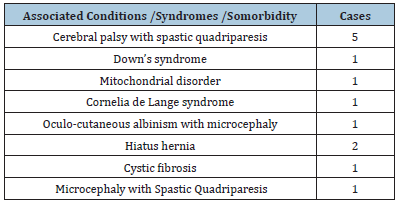
A retrospective study of 13 patients who underwent laparoscopic Nissen fundoplication with or without laparoscopic gastrostomy at our institution under a single surgeon was done. Recorded data of their preoperative diagnosis, indications for surgery, operative procedures were collected. There were 8 males and 5 females. Age ranging from 8 months to 15.2 years. Indication for surgery was severe gastro esophageal reflux and recurrent aspiration pneumonia with failed medical therapy and failure to thrive. Underlying cause of GERD and comorbidities are described in Table 1. Standard laparoscopic floppy 3600 Nissen fundoplication procedure was performed using a 5 trocar technique and with 5mm or 3mm instruments depending on the size and age of the patients. For children older than 3 years all ports were of 5mm size, and for children less than 3 years 5mm ports were only used for the main umbilical port and the left hypochondrial port, for the rest 3mm ports were used. When required a concurrent laparoscopic tube gastrostomy was also performed with the left hypochondrial port as the gastrostomy site. The postoperative recovery, duration of hospital stay and occurrence of early and late complications were noted using outpatient follow up notes and telephonic assessment.
Table 1: Diagnoses of patients with GERD in study.
Results
10 of the 13 laparoscopic procedures were completed successfully and 3 cases were converted to open. Reasons for conversions were, difficulty in wrapping the fundus (a thickened oedematous oesophagus secondary to recalcitrant reflux esophagitis) in two of the cases and intraoperative finding of an associated malrotation of gut in one. Operative time improved from 235 minutes to 150 minutes with an average of 182 minutes. Laparoscopic gastrostomy was performed in 8 out of 13 patients; 3 of the children had previous open gastrostomy done and 2 (hiatus hernia) did not need it. In all cases blood loss was minimal and no other intraoperative complications were encountered. Postoperatively feeds were started on day two and patients were discharged on average of 6.1 days. Pulmonary complications, need for postoperative ventilation, bowel disturbances were not seen in any of the patients. Gastrostomy site infection/cellulitis occurred in 3, and responded to systemic and topical antibiotics. Gas bloat was seen in two patients, in the early postoperative period. Long term follow-up ranged from 8 to 32 months. 3 out of the 13 patients died due to other associated comorbidities between 14 to 24 months after the surgery. 2 children with hiatus hernia had Sandifer syndrome, which resolved postoperatively. All patients demonstrated good weight gain and no had no further aspiration episodes. Retching was noted in 2 patients. One patient had occasional vomiting which was found only to be associated with episodes of UTI, but remained asymptomatic at other times. None of the patients needed any acid suppression medication. All patients with gastrostomy tolerated bolus pureed home cooked feeds through gastrostomy. Six patients are able to take oral feeds, 4 of whom are also given supplemental gastrostomy feeds. Children also showed catch up growth. In children with neurological impairment, parents also reported better participation in therapy after the increased calorie intake possible following surgery with improvement in milestones and enhanced neurological development. The satisfaction with the operation both during admission, postoperative recovery and the results of the surgery were uniformly good.
Discussion
Gastroesophageal Reflux (GER) is a common symptomatic clinical disorder affecting the gastrointestinal tract of infants and children. Particularly in those patients with neurologic disorders, there appears to be a high prevalence of autonomic neuropathy in which esophago-gastric transit and gastric emptying are frequently delayed, producing a somewhat complex foregut motility disorder [1]. Medical treatment for Gastroesophageal Reflux Disease (GERD) though has improved vastly over the years, failure of medical treatment remains vexing among those who are neurologically impaired [1,2]. Surgery is indicated when these measures fail, or when complications develop. Children with associated anatomic problems, such as large hiatal hernia are more likely to require surgical fundoplication, to reduce their likelihood of esophagitis with bleeding, aspiration pneumonia, or both [2]. The transabdominal Nissen’s fundoplication is the most widely used antireflux procedure worldwide in children. A loose wrap is essential in view of the common association of esophageal motility disorders and to permit the child to burp after the operation. A transient tube gastrostomy may be used for venting the stomach in infants and young children if there is concern of gas bloat [1].
Laparoscopic Nissen’s fundoplication has been shown to offer results similar to open surgery, though with lesser morbidity. Postoperative respiratory complications and ventilator dependence were reduced, and children were able to return to baseline function and diet much sooner. Although the learning curve is steep because of the advanced laparoscopic techniques required to perform a fundoplication, the procedure can be performed quickly and effectively once these skills are mastered [3]. Moreover, it has been found to be feasible, safe, and effective, even in very small babies [4,5]. Lower postoperative complications following laparoscopy have been reported in several studies. In a study of 1050 patients, intraoperative and postoperative complications were 0.26% and 4.0% [6]. Capito C et al [7] in their study with the neurologically impaired children showed more than 85% of the children were symptom free after 5 years [7]. The technical advantages offered by a laparoscopic approach like the exposure of the hiatus and gastric anatomy can allow formation of an anatomically correct wrap, which is not under tension and does not twist or torque the stomach, which can contribute to lower incidence of dysphagia, gas bloat, and other symptoms often associated with a fundoplication [8]. Mathei J et al [9] reported a conversion rate of 2.8%, and major postoperative complications occurred in 12 of 106 patients, mostly those with neurologically impairment. However, later dysphagia was seen in 23 patients of which 4 required dilatations and 2 a redo Nissen’s. Gas bloating occurred in 15 children, with spontaneous regression in all [9]. In our series, we have had higher conversion rate, probably due to learning curve, but our complications have been low. Rothenberg, in the impressive experience of 2000 children, reported very low intraoperative and postoperative complication rates of 0.13% of 4.0% respectively [10].
In our health care setup, many parents with children having chronic neurological conditions are not able to avail the same level of care as in western countries both due to financial/time constraints for the carers, and apprehension of causing pain to the child. One of the concerns for the parents was the post-operative period, because if there was a long break in physiotherapy, they could start developing deformities/ increased spasticity etc. All these cause significant delay in seeking care, and psychological barriers in accepting surgical options. In our experience with laparoscopic fundoplication and gastrostomy, there has been a universally positive feedback from parents regarding both the procedure, postoperative recovery as well as the results of the procedure. Early, safe and smooth resumption of therapy was also possible after laparoscopic surgery. One of the greatest satisfaction both for the neurologist and surgeon was when parents of these children started recommending this to other parents at the special schools as they felt it would help the other children as well.
Conclusion
Our experience shows that laparoscopic Nissen’s fundoplication can be an attractive option for infants and children suffering from GERD with underlying neurological deficits. The recovery is quick, with low complication rates and with good long-term results. Moreover, we found good parental acceptance as its lower pain score and early recovery helps to offer surgery as an option to parents who are concerned of subjecting their children to painful surgical interventions.
References
- Fonkalsrud EW, Ament ME (1996) Gastroesophageal reflux in childhood. Curr Probl Surg 33:1-70
- Hillemeier AC (1996) Gastroesophageal reflux. Diagnostic and therapeutic approaches. Pediatr Clin North Am 43(1): 197-212.
- Meehan JJ, Georgeson KE (1997) The learning curve associated with laparoscopic anti-reflux surgery in infants and children. J Pediatr Surg 32(3): 426-429.
- Zamir O, Udassin R, Seror D, Vromen A, Freund HR (1997) Laparoscopic Nissen fundoplication in children under 2 years of age. Surg Endosc 11(12): 1202-1205.
- Meehan JJ, Georgeson KE (1996) Laparoscopic fundoplication in infants and children. Surg Endosc 10(12): 1154-1157.
- Rothenberg SS (2005) The first decade's experience with laparoscopic Nissen fundoplication in infants and children. J Pediatr Surg 40(1): 142-146.
- Capito C, Leclair MD, Piloquet H, Plattner V, Heloury Y, et al. (2008) Long-term outcome of laparoscopic Nissen-Rossetti fundoplication for neurologically impaired and normal children. Surg Endosc 22(4): 875-880.
- Hopkins MA, Stringel G (1999) Laparoscopic Nissen fundoplication in children: A single surgeon's experience. JSLS 3(4): 261-266.
- Mathei J, Coosemans W, Nafteux P, Decker G, De Leyn P, et al. (2008) Laparoscopic Nissen fundoplication in infants and children: analysis of 106 consecutive patients with special emphasis in neurologically impaired vs. neurologically normal patients. Surg Endosc 22(4):1054-1059.
- Rothenberg SS (2013) Two decades of experience with laparoscopic Nissen fundoplication in infants and children: A critical evaluation of indications, technique, and results. J Laparoendosc Adv Surg Tech A 23(9): 791-794.
© 2021 Lakshmi Sundararajan. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






