- Submissions

Full Text
Research in Pediatrics & Neonatology
Juvenile Psoriatic Arthritis with Incidental Finding of Factor VII Deficiency: A Case Report
Fouzia Alsobhi1, Abdullah Alharbi2, Khayria Alsufyani3, Usman Saeed4, Salma iltaf5 and Khaled Ismail AbdElShakoor6*
1Pediatric hematology Consultant, Maternity Children Hospital, Makkah, Saudia Arabia
2Pediatric Saudi Board Resident, Maternity Children Hospital, Makkah, Saudia Arabia
3Pediatric Rheumatology Consultant, Maternity Children Hospital, Makkah, Saudia Arabia
4Pediatric Registrar, Maternity Children Hospital, Makkah, Saudia Arabia
5FCPS Trainee Histopathology, Shifa International Hospital, Saudia Arabia
6Pediatric Senior Registerar, Maternity Children Hospital, Makkah, Saudia Arabia
*Corresponding author: Khaled Ismail AbdElShakoor, Pediatric Senior Registrar, Maternity and Children Hospital (MCH), Ministry of Health, Makkah, Saudi Arabia
Submission: May 03, 2021; Published: May 17, 2021

ISSN: 2577-9200 Volume5 Issue4
Abstract
Juvenile Psoriatic Arthritis (JPsA) is a distinct type of arthritis that develops in children with psoriasis. According to the National Psoriasis Foundation, Psoriatic Arthritis is found in 10-30% of cases diagnosed with psoriasis. Here, we report a rare case of juvenile psoriatic arthritis in a 12-year-old child with an incidental finding of factor VII deficiency irrespective of causing any coagulation disorder.
Keywords:Juvenile Psoriatic arthritis; Factor VII deficiency; Factor VII; Incidental
Introduction
Psoriatic Arthritis (PsA) is a heterogeneous group of diseases with variable presentations. It involves pain and inflammation in joints and progressive joint involvement and damage. The condition is associated with skin disease Psoriasis, but not all people with Psoriasis will develop Psoriatic Arthritis. Factor VII deficiency is a rare congenital clotting disorder that develops in 1 out of 500,000 individuals. It causes excessive or prolonged bleeding following a trauma or surgery. The most common clinical presentations include epistaxis, menorrhagia or post tooth extraction bleeding. However, hemarthrosis may occur rarely. There is lack of correlation between the blood plasma levels and severity of symptoms. Cases with marked Factor VII deficiency may lack related symptoms. Such cases are diagnosed with another disease with incidental finding of Factor VII deficiency.
Case Report
Figure 1: Muscle wasting is prominent.

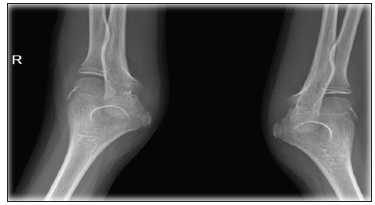
A 12-year-old Saudi boy born to consanguineous parents and presented to Pediatric hematology clinic with intermittent joint swelling for 2 years. He was previously diagnosed as Factor VII deficiency at another hospital and received recombinant Factor VII replacement for unknown period with no significant improvement. Local examination showed painful swelling of bilateral elbow joints and right ankle joint with restricted range of movements and overlying skin redness. Mild muscle wasting was also noticed (Figure 1). Furthermore, patient was circumcised at the age of 1 month, and multiple tooth extractions were done before 10 years of age without any significant bleeding [1]. Laboratory findings showed low hemoglobin (10.7g/dl) with deranged bleeding profile and factor VII deficiency. Radiological examination showed marked effusion of bilateral elbow joints and right ankle joint with left elbow extraarticular synovial cyst (Figure 2).
Figure 2: X-Ray of both elbows showed marked swelling of both joint with erosion.
Initially, Patient was treated as case of hemarthrosis and given Factor VII replacement, but it showed no improvement. Later, a trial of short course of steroid (2mg/kg/day) was given for 2 weeks. There was marked improvement clinically with disappearance of joint swelling. On gradual tapering of steroids, the joint swelling was reappeared. Joint aspiration was done on further consultation and showed features of synovitis (Figure 3). Follow up examination of patient in rheumatology clinic revealed skin rashes typical of Psoriasis. Family history showed two family members have been diagnosed with Psoriasis. Based on all these findings, Patient was finally diagnosed as case of Juvenile Psoriatic Arthritis with incidental finding of Factor VII deficiency [2]. On follow up, Patient showed marked improvement following the methotrexate and steroid therapy (Table 1).
Figure 3: Joint aspiration under guidance of Ultrasound.

Table 1:
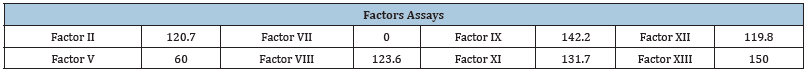
Laboratory Tests: *Hgb: 10.7 (g/dL), *PTT & PT by Mixing study, PTT was 26.8, PTT after was corrected with 25.7seconds, PT: 21.7 after was corrected with 12.2, INR:2.1 after was corrected with INR:1.1 * Peripheral blood Smear: Unremarkable * ESR: 7 *CRP: <0.2 .
Discussion
We report a case of Juvenile Psoriatic Arthritis with an Incidental finding of Factor VII deficiency. This report is intended to show the overlapping clinical features of Psoriatic Arthritis with Factor VII deficiency. Patient was initially presented with hemarthrosis and treated for factor VII deficiency, but there was no improvement. The case was further reviewed based upon laboratory, radiological and cytological findings and finally diagnosed as Psoriatic Arthritis with incidental finding of Factor VII deficiency. Factor VII deficiency is the commonest autosomal recessive coagulation disorder. The clinical features are variable that range from severe massive bleeding (i.e. intracranial or gastrointestinal) to mild symptoms (i.e. epistaxis) and even remains asymptomatic [3]. In our case, patient was circumcised at age of 1 month and had multiple tooth extractions before age of 10 years without causing the significant bleeding.
Furthermore, in our case, Patient was initially presented with overlapping clinical feature of hemarthrosis. He was treated in the line of Factor VII deficiency, but it showed no improvement. The case was further investigated. Radiological examination showed the multiple joint effusions and excluding the hemarthrosis. Effusion cytology further supported the finding by showing the feature of synovitis. The case was finally diagnosed as Juvenile Arthritis with incidental finding of Factor VII deficiency. Patient was treated with steroid therapy, methotrexate and showed significant improvement.
References
- Peyvandi F, Palla R, Menegatti M, Siboni SM, Halimeh S, et al. (2012) Coagulation factor activity and clinical bleeding severity in rare bleeding disorders: Results from the European network of rare bleeding disorders. J Thromb Haemost 10(4): 615-621.
- Mariani G, Dolce A, Marchetti G, Bernardi F (2004) Clinical picture and management of congenital factor VII deficiency. Haemophilia 10(Suppl 4): 180-183.
- Ferraresi P, Balestra D, Guittard C, Buthiau D, Pan-Petesh B, et al. (2019) Next-generation sequencing and recombinant expression characterized aberrant splicing mechanisms and provided correction strategies in factor VII deficiency. Haematologica 105(3): 829-837.
© 2021 Khaled Ismail AbdElShakoor. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






