- Submissions

Full Text
Research in Pediatrics & Neonatology
Inflammatory Myofibroblastic Tumor: Encounter with A Rare Tumour in Pediatric Age Group
Adhikari SB1* and Saiful Islam M2
1Department of Pediatric Surgery, Bangladesh
2Department of Pediatric Surgery, Bangladesh
*Corresponding author:Suman Bikram Adhikari, Department of Pediatric Surgery, Bangladesh
Submission: March 12, 2019; Published: January 17, 2020

ISSN: 2577-9200 Volume4 Issue2
Abstract
Inflammatory myofibroblastic tumor, a rare benign tumor, occurs at any site in the body, is more common in pediatric age group than adult. Among them, inflammatory myofibroblastic tumors arising from stomach and mesentery are rare entity.
We report two cases
A. 9 years old boy who suffered from dysphagia, vomiting and weight loss. Barium swallow examination revealed narrowed distal esophagus up to lower gastro-esophageal junction with bird-beak appearance. UGI Endoscopy revealed narrowed lower esophagus. During operation, the mass was found to be in fundus of stomach obstructing gastro-esophageal junction and total radical gastrectomy was done and histopathology report traced inflammatory myofibroblastic tumor.
B. 7 years old boy presented with recurrent (two times operated) ill-defined, periumbilical abdominal mass. Previous tissue biopsy was non-conclusive. Abdominal Contrast CT Scan revealed heterogenous mass in epigastric and umbilical region encasing Superior Mesenteric Artery (SMA), which could not be separated from small bowel loops. During operation, the tumor was found to be arising from root of mesentery, encasing SMA & Head of Pancreas and adhere with almost middle ½ of small intestine. Debulking of mass along with resection anastomosis of small intestine was realized and histopathology report traced inflammatory myofibroblastic tumour.
Keywords: Inflammatory myofibroblastic tumour
Introduction
Inflammatory Myofibroblastic Tumor (IMT) is a rare benign but locally aggressive tumour [1]. It occurs primarily in children and young adults, but it can occur at any age and can arise from various anatomic locations [2]. These tumors have been found in numerous sites but rarely in stomach and root of mesentery [3]. Management regarding IMT is still obscure and challenging as no particular treatment protocol has been established yet. However, Tumor recurrence is unusual following complete surgical resection or organ-preserving modality therapy [1].
Case Reports
Case report A
We report a case of 9 years old boy with difficulty in swallowing mainly solid food, vomiting and loss of weight since the age of 5 years. On examination, no abdominal palpable lump was found. Upper GI Endoscopy showed marked narrowing at 26cm from incisor teeth with no apparent mucosal lesion noted. But, scope could not be passed through narrow part distally. Due to poor financial condition of patient, CT scan of the abdomen was not done. Barium swallow of esophagus showed narrow distal esophagus with temporary holdup of barium at distal esophagus with proximal dilatation, narrowing was up to the gastro-esophageal junction and giving a bird-beak appearance Figure 1. The resort to surgery was diagnostic (the tumor presented at fundus of stomach and obstructing lower gastro-esophagus junction) and therapeutic purposes and consisted in a total radical gastrectomy. On gross examination Figure 2, two nodular like tumor arise from the anterior wall of fundus of stomach, measuring 5*5 and 3*3cm² respectively; firm; chalky-white on cut section. Microscopic examination revealed lining epithelium shows mild dysplastic changes and infiltration of chronic inflammatory cells, subepithelial region shows infiltration of moderate number of chronic inflammatory cells, based on this data, Gastric IMT was diagnosed. There are very few indications of total radical gastrectomy in pediatric age group. The patient after radical gastrectomy developed nutritional deprivation and kwashiorkor. His life was very challenging particularly due to his rural settings, illiteracy of his parents, poverty, and uncertainty of follow up Figure 3-7. Unfortunately, by the age of 11 years, he died due to consequence of poor nutrition.
Figure 1:Barium swallow showing bird beak appearance.
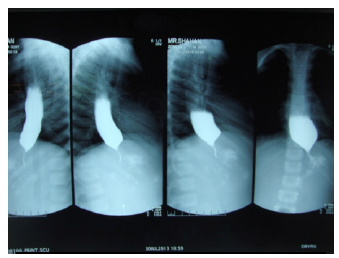
Figure 2:Specimen of the tumour. Arrow indicates the tumour lesion.
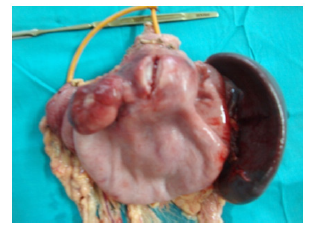
Figure 3:Preoperative appearance.

Figure 4:kwashiorkor developed postoperatively

Figure 5:Scrotal oedema due to malnutrition.

Figure 6:Bilateral pitting oedema due to malnutrition (Arrow indicate pitting on pressure).

Figure 7:

Case report B
We report another case of a 7 years old boy with recurrent ill-defined periumbilical abdominal mass for 6 months for which he underwent in early childhood two times incisional biopsy. Both previous biopsies were not confirmatory. Contrast CT Scan of the whole abdomen revealed large lobulated heterogeneously enhancing soft tissue mass in epigastric and umbilical regions encasing SMA and the mass could not be separated from small bowel loops. With this presentation, exploratory laparotomy was performed where a firm mass arising from the root of mesentery encasing SMA & Head of pancreas which adhered with almost middle ½ of small intestine was found.
There was no ascitic fluid, enlarged lymph node and other viscera’s were normal. Debulking of tumour mass with resection anastomosis of jejuni-ileal was performed with at least 5cm clear margin macroscopically. Gross examination revealed 7*5cm² firm, greyish mass which on cut section appeared grey brown and solid. Histopathological Biopsy revealed spindle cell proliferation in a myxoid and inflammatory background and mesenteric IMT diagnosis was made. No Immunohistochemistry was done due to low socioeconomic condition of patient. He developed Enterocutaneous fistula from the drain site on 8th POD along with SAIO, for which exploratory laparotomy with release of adhesion followed by end terminal ileostomy was done. Child was then kept in a regular follow up and nutritional status was improved. After 6 months, restoration of gut was done with side-to-side ileoascending colon anastomosis. At the same setting, evaluation of primary lesion/tumour was done and there was not any evidence of growth of tumour.
Discussion
Gastric IMT is an extremely uncommon entity. To our knowledge, 16 pediatric cases of gastric IMT have been reported in the literature [3,4]. The mesentery and omentum are the most common sites of extra-pulmonary inflammatory myofibroblastic tumor. In a study by Coffin [5] and associates, 43% of these tumors (36 of 84) arose in these sites. Extra-pulmonary inflammatory myofibroblastic tumors show a predilection for children, with a mean age of 10 years at presentation. Females are affected slightly more than males [5]. These are the first cases reported in Bangladesh among pediatric surgical patients. IMT is a rare benign soft tissue tumour which may arise from any anatomical sites. Other names described these tumors: atypical fibro myxoid tumor, plasma cell granuloma, pseudo-sarcomatous fibro myxoid tumor, inflammatory pseudotumor, postoperative spindle cell nodules, pseudo sarcomatous myofibrotic proliferations [1,2,6]. Apart from stomach& mesentery, the other sites reported are lung (commonest), urinary bladder, liver, spleen, lymph nodes, esophagus, salivary glands, breast, epididymis, central nervous system, and soft tissues [6-8].
The IMT affects both sexes, at any ages, with a slight predominance in children and young adults [7,8]. The pathogenesis of IMT is unknown. Several hypotheses have been proposed such as an auto-immune mechanism or infectious origin. Infectious microorganisms include Mycoplasma, Nocardia, Actinomycetes, Epstein-Barr and Human herpes virus [9,10]. Other studies, however, suggest that it might be a true neoplasm due to the presence, at the myofibroblastic component, of a fusion gene involving the ALK gene, a tyrosine kinase oncogene located on chromosome 2p23, initially found to be arranged in anaplastic large cell lymphomas. This fusion leads to constitutive over-expression of the ALK, causing cell proliferation [2,7,10,11].
On presentation, IMT can constitute a challenge, from diagnosis through to treatment. In this report, we present cases of a patient with gastric and mesenteric IMT that challenged radiologists, pathologists, and inevitably, surgeons. Most of these tumors are discovered incidentally. The current histopathological definition of an IMT is a distinctive neoplasm composed of myofibroblastic mesenchymal spindle cells accompanied by an inflammatory infiltrate of plasma cells [12,13]. Currently, surgery is the mainstay of treatment for IMTs. Complete removal of the tumour generally provides resolution of all symptoms and laboratory abnormalities.
However, tumors in intra-or retroperitoneal locations tend to invade adjacent structures, preventing curative resections and breeding local recurrences [14]. These patients require further management. Unfortunately, chemotherapy and radiotherapy are not successful in most patients. Recently, researchers have published promising results with anti-inflammatory agents and anti-tumour necrosis factor-α binding antibodies [15].
Despite of being a benign tumor, it is considered by some authors as a low-grade tumor because of malignant features such as local invasiveness, recurrence (4% in cases of incomplete resection) or malignant transformation (exceptional). The evolution depends on the tumor size (less than or equal to 3cm) and the quality of surgical resection. The 5-year survival is 91.3% [6-10].
Conclusion
Inflammatory myofibroblastic tumors are rare benign soft tissue tumors. Their presentation depends upon the site from where they origin and confirmation are done only by histopathology and immunochemistry. Despite being a benign lesion, its potential for recurrence and local invasion requires complete surgical resection.
References
- Kovach SJ, Fischer AC, Katzman PJ, Salloum RM, Ettinghausen SE, et al. (2006) Inflammatory myofibroblastic tumors. J Surg Oncol 94(5): 385-391.
- Coffin CM, Hornick JL, Fletcher CD (2007) Inflammatory myofibroblastic tumor: Comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive cases. Am J Surg Pathol 31(4): 509-520.
- Lazure T, Ferlicot S, Gauthier F, Doz F, Couturier J, et al. (2002) Gastric inflammatory myofibroblastic tumors in children: An unpredictable course. J Pediatr Gastroenterol Nutr 34(3): 319-332.
- Riedel BD, Wong RC, Elizabeth HE (1994) Gastric inflammatory myofibroblastic tumor in infancy: Case report and review of the literature. J Pediatr Gastroenterol Nutr 19(4): 437-443.
- Coffin CM, Watterson J, Priest JR, Dehner LP (1995) Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). A clinicopathologic and immunohistochemical study of 84 cases. Am J Surg Pathol 19(8): 859-872.
- Pinillaa I, Herreroa Y, Torresa MI, Nistalb M, Pardoa M (2007) Myofibroblastic pulmonary inflammatory tumor myofibroblastic inflammatory tumor of the lung. Radiology 49(1): 53-55.
- Zhang Y, Dong ZJ, Zhi XY, Liu L, HU M (2009) Inflammatory myofibroblastic tumor in lung with osteopulmonary arthropathy. Chin Med J 122(24): 3094-3096.
- Racil H, Saad S, Ben AJ, Cheikh RS, Chaouch N, et al. (2011) Invasive inflammatory pseudotumor invasive inflammatory pseudotumor of the lung. The Journal of Internal Medicine 32(4): e55-e58.
- Ochs K, Hoksch B, Frey U, Schmid RA (2010) Inflammatory myofibroblastic tumour of the lung in a five-year-old girl. Interact Cardiovasc Thorac Surg 10(5): 805-806.
- Chien KC, Chia IJ, Jian ST, Hsu CH, Pin RC, et al. (2010) Inflammatory myofibroblastic tumor of the lung- a case report. J Cardiothorac Surg 5(55): 1-4.
- Bousnina S, Racil H, Marniche K, Hassine E, Fekih L, et al. (2004) Inflammatory pseudo-tumors of the lung: An anatomo-clinical study of an inflammatory pseudo-tumor of the lung observation. A pathology clinical study of one case. Journal of Clinical Pulmonology 60(1): 55-57.
- Sirvent N, Coindre JM, Pedeutour F (2002) Inflammatory myofibroblastic tumors. Ann Pathol 22(6): 453-460.
- Ozgur F, Safak O, Taner A, Ahmet C (2009) Inflammatory myofibroblastic tumor. Can J surg 52(3): E60-E61.
- Pungpapong S, Geiger XJ, Raimondo M (2004) Inflammatory myofibroblastic tumor presenting as a pancreatic mass: A case report and review of the literature. JOP 5(5): 360-367.
- Germanidis G, Xanthakis I, Tsitouridis I, Zaramboukas T, Kiskinis D, et al. (2005) Regression of inflammatory myofibroblastic tumor of the gastrointestinal tract under infliximab treatment. Dig Dis Sci 50(20): 262-265.
© 2020 Suman Bikram Adhikari. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






