- Submissions

Full Text
Research in Pediatrics & Neonatology
Posterior Urethral Valve
Al hojaili N*, Al Zahrani A, kutbi I, Al Malik H, Ali S and Yosef M
Maternity children hospital, Saudi Arabia
*Corresponding author:Najia al hojaili, Makkah, Maternity children hospital, Saudi Arabia
Submission: November 15, 2019; Published: November 25, 2019

ISSN: 2577-9200 Volume4 Issue1
Abstract
Posterior urethral valve (PUV) disorder is an obstructive developmental anomaly in the urethra and genitourinary system of male newborns [1]. A posterior urethral valve is an obstructing membrane in the posterior male urethra as a result of abnormal in utero development. It is the most common cause of bladder outlet obstruction in male newborns. PUV may cause the kidneys to swell-this is called antenatal hydronephrosis and is a common problem for babies in the womb. Occasionally, this causes more serious problems. Boys with PUV may be more likely to get urinary tract infections (UTIs) when germs get into the urine and cause infection and illness. These are treated with medicines. In some cases, boys with PUV get a serious infection in their kidneys or in their blood. PUV may cause vesicoureteral reflux (VUR)- when urine refluxes (goes back up) the wrong way towards or into the kidneys.20-30 of patient had renal failure even if treated
Epidemiology
In the United States, PUV is the most common cause of lower urinary tract obstruction in male neonates; the reported incidence ranges from 1 per 8000 to 1 per 25,000 live births.
Case Presentation
F.T 2.9 kg, 11 days old, shifted from another hospital as a case of PUV and bilateral hydronephrosis.
Product of a mother 45 years G8 P6+1, hepatitis B carrier, negative consanguinity (baby received hepatitis vaccine and immunoglobulin.in his hospital.
Investigation
CBC: was normal
Chemistry sent
Echocardiogram was done PFO, mild PS
Seen by urology and booked for operation
Antenatal diagnosis
The widespread use of antenatal ultrasonography (US) has enabled diagnosis of posterior urethral valves (PUVs) in many more individuals. Patients who have PUVs that are not diagnosed on antenatal US and who do not present with overt urinary pathology are at risk for delayed presentation of PUVs.
Differential diagnosis
A. Neonatal hydronephrosis
B. Urnary tract infection
C. Viasicoureteric Reflex
D. Renal failure
Management
Treating before birth
In most cases, there is no treatment before birth. In a small number of cases, and only when the level of amniotic fluid (or liquor) around the baby has dropped, a surgical procedure called a vesico-amniotic shunt is recommended during pregnancy. This operation is always done by trained healthcare professionals in a specialist center. A tube (the shunt) is inserted through the mother’s abdomen and into the baby’s bladder. This aims to drain urine out of the baby’s bladder and into the amniotic fluid. This reduces the effects of pressure and helps the baby’s lungs to develop normally. Your healthcare team will talk to you about the risks of the procedure and the risks of not doing the procedure, so you can make an informed decision. Our case admitted in NICU operated in 2nd day of admission there was UVC+ circumcision+ vasectomy, Urethra was edematous with blood spot and debris. Many attempts done and scope was not clear. Pt. developed desaturation b/o diffusion of saline from urinary bladder to periton and try to empty the bladder, Route was blocked by edema, so vasectomy done, and Foley’s catheter inserted, fulguration was failed [2,3].
Baby return from OR on mechanical ventilation. Sepsis work up was done, Baby on Meropenam and Ditropan. Creatinine starts to rise, and baby developed generalized edema and anuria, thrombocytopenia
Hypertension, IV fluid adjusted according to IWL + Urine output
ID consultation was done continue Meropenem and Bactrim
For LP when it is possible. To do CT brain with contrast r/o CNS infection
Nephrology consultation done: their impression was obstructive Uropathy
Plan to do HD only if:
1. Refractory acidosis
2. Refractory hyperkalemia
3. Sign of fluid overload (pulmonary edema).
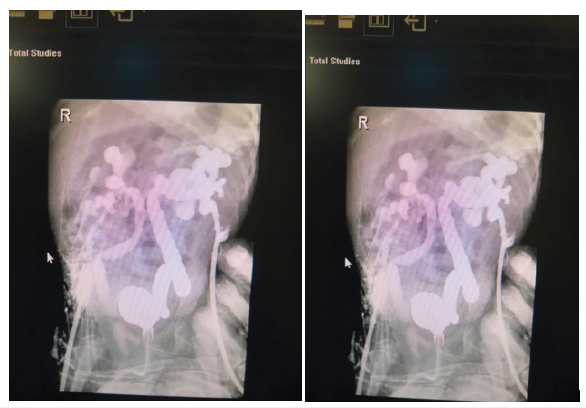
Serial renal US was done which showed increase in parenchymal echogenicity with grade II nephropathy and enlarged both kidneys with marked dilated calycle system and both ureters. BL/c came Burkholderia cepacian Bactrim was added and dose adjusted. Baby went for 2nd OR, 2nd exploratory laparotomy and cystoscopy they found UB perforation. And then bed side contrast was done there was bladder extra vacation of contrast, no intrapretonial fluid. Urgent bilateral nephrostomy was done guided by US.in Al-Noor hospital. Dye was injected there were bilateral hydronephrosis and no connection with urinary bladder After nephrostomy baby improved dramatically creatinine go down, urine output calculated from nephrostomy, IVF adjusted, baby ex-tubated to room air, vitally stable. Planned by urology team to do nephrostogram which was done and showed; RT nephrostogram shows dilated tortuous Rt. ureter and pelvicalceal system, the contrast reached the distal RT ureter but did not pass into the bladder. LT nephrostogram shows severely dilated tortuous LT ureter and pelvicalceal system and contrast passed into bladder. Planned by urologist to clamp the Lt. nephrostomy to allow passage of urine to UB but if LT ureter increase in size or creatinine increase open the clamp (It was successful attempt the baby pass urine from bladder). For removal of Lt nephrostomy. Their plan to do RT nephrostogram and if passed urine to UB to remove Rt. nephrostomy and to do fulguration for PUV Figure 1-2.
Figure 1:
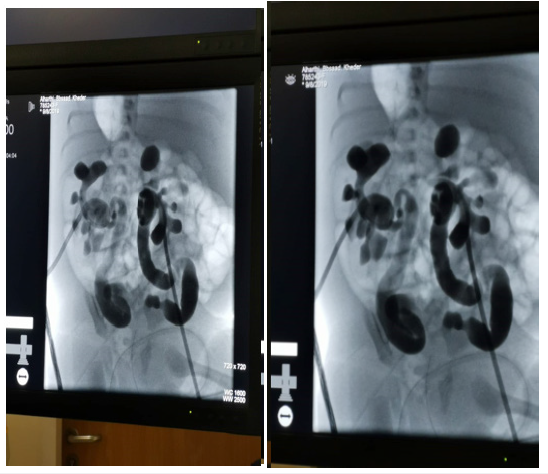
Figure 2:
Complication
A. Lung hypoplasia duo to This happens when PUV cause there to be less amniotic fluid (or liquor), the fluid that babies float in when growing in the womb, than usual. In extreme and rare cases, the lungs do not develop enough for the support to help, and the baby dies before, or shortly after birth. The baby swallows and “breathes in” the amniotic fluid. When the kidneys develop, they start making urine. The baby passes the urine out, adding to the amount of amniotic fluid. If the baby cannot pass urine, there is not enough amniotic fluid-this is called oligohydramnios. In serious cases, this can stop the lungs fully developing-this is called pulmonary hypoplasia.
B. Limb deformity duo to oligohydramnios.
C. Renal failure if PUV is severe.
D. Vesico ureteric Reflex.
Prognosis
Over the past 30 years, the prognosis of children with PUV has steadily improved. In the past, most children were found to have PUV only after presenting with urosepsis or progressive renal insufficiency. Older series demonstrated mortality figures approaching 50% by late adolescence. Today, most individuals with PUV are discovered when antenatal US reveals hydronephrosis. Prompt resolution of bladder obstruction, aggressive treatment of bladder dysfunction, and improved surgical techniques have lowered the neonatal mortality to less than 3%. PUVs are the cause of renal insufficiency in approximately 10-15% of children undergoing renal transplant, and approximately one third of patients born with PUV progress to ESRD in their lifetimes. Early initial presentation, pneumothorax, bilateral vesicoureteral reflux (VUR), and recurrent UTIs after valve ablation are all associated with risk for progression to ESRD
Follow-Up
A check cystoscopy may be done after some time, to make sure the PUV have been completely removed. If they have not, they will need to resect away again. Sometimes they will need an alternative treatment. Kidney function tests check how well your child’s kidneys are working. They include blood tests urine tests. ultrasound scans or other imaging tests, such as DMSA and MAG3 scans-to look at their kidney.
References
- Manzoni C, Valentini AL (2002) Posterior urethral valves. Rays 27(2): 131-134.
- Heikkilä J, Holmberg C, Kyllönen L, Rintala R, Taskinen S (2011) Long-term risk of end stage renal disease in patients with posterior urethral valves. J Urol 186(6): 2392-2396.
- https://www.infokid.org.uk/
© 2019 Najia al hojaili. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






