- Submissions

Full Text
Research in Pediatrics & Neonatology
Assessing Emotion Recognition in Adolescents After Traumatic Brain Injury: A Neuropsychological Cohort Study
Kathy T. T. Vu1, You Jung Seo1 and Brenda Hussey-Gardner2*
1University of Maryland, Baltimore County
2University of Maryland School of Medicine
*Corresponding author:Brenda Hussey- Gardner, Department of Pediatrics, University of Maryland School of Medicine, 110 South Paca Street-8th Floor, Baltimore, MD, USA 21201
Submission: October 11, 2019; Published: November 07, 2019

ISSN: 2576-9200 Volume3 Issue5
Abstract
Mental health difficulties of traumatic brain injury (TBI) interfere with rehabilitative interventions and following their discharge from inpatient rehabilitation settings. Little is known in Saudi Arabia about how emotion recognition abilities become affected after TBI. The aim of this study was to determine whether emotion recognition deficits may be additional mental health impairment for adolescents with TBI. A cohort study of five adolescents with TBI at the outpatient rehabilitation psychology clinic at the Rehabilitation Hospital of King Fahad Medical City (KFMC) was conducted. Deficits in recognizing emotion was reported among the sample. The finding highlights the importance of providing valid neuropsychological assessments in order to target emotion recognition limitations in the rehabilitation interventions programs.
Keywords: Emotion recognition; Neuropsychology; Traumatic brain injury; Rehabilitation; Cognation.
Introduction
A recent Saudi study [1] showed that TBI is the most common pediatric trauma and could be linked with harmful consequences. Deficits in the ability to evaluate emotional information are implicated in TBI. Researchers indicate that lasting emotion recognition deficits are common among adolescents who have suffered TBI [2]. Although adolescents who have TBI are generally discharged following rehabilitation hospitalization, some adolescents need additional rehabilitation interventions in the post-injury period, including outpatient services [3]. Studies showed that more than half of TBI adolescents are at risk of presenting with emotion recognition difficulties.
Preschoolers and elementary school students were mostly affected by TBI consequences in Saudi Arabia [1]. Survivors of adolescents TBI commonly result in emotional, behavioral and cognitive deficits [2]. However, emotion recognition deficits following TBI become obvious at age of adolescent hood and above [4]. Parents rate behavior disturbance and emotion changes as the most difficult and persistent problem following TBI. Emotion recognition requires the quick processing of motivations and emotional reactions of others. Essential emotional stimuli are conveyed by facial and eye expression [5]. Assessing adolescent’s abilities to understand emotion from facial expressions indicates that such skills are subject to developmental improvement mainly among adolescents with TBI.
In light of the growing recognition that TBI among adolescents may contribute to the development of emotion recognition difficulties, it is critical to assess the emotion recognition deficits after pediatric brain injury. No previous study in Saudi Arabia has taken this investigation approach to evaluate this issue. The main aim of the current study was to investigate how adolescents may suffer from emotion recognition deficits following TBI. To date, the ability of adolescents diagnosed with TBI to correctly identify facial emotion expressions has not been assessed in Saudi Arabia yet. Identification of such deficits may aid the health care professionals in identifying patients who may be in need of additional rehabilitation interventions.
Case Report
Five adolescents with TBI (two males and three females) were selected from a sample of TBI adolescents who experienced moderate to severe closed head injuries and had been referred to the outpatient rehabilitation psychology clinic at the Rehabilitation Hospital of King Fahad Medical City RH-KFMC in Al Riyadh. The recommended clinical Psychology Ethics guideline was applied [6]. Full information on the procedures of the psychometric assessments was given to the parents. Informed consent was obtained from both the parents and their adolescents. All of the adolescents had a recorded Glasgow Coma Scale (GCS) score which had been reported in the hospital records. Individual details for each adolescent are provided in Table 1. In order to select the adolescents from the outpatient rehabilitation psychology clinic, the Arabic version of the fifth edition of the Stanford-Binet Intelligence Test (SBITA) [7] and the Vineland Adaptive Behavior Scales, Arabic version (VABSA) [8] were given to all the adolescents and their parents. Only those patients with within borderline IQ or above according to the SBITA were included.
SBITA aims to measure four intellectual areas: Verbal, Abstract and Visual, Quantitative, and Short-term Memory. The SBITA has been found to be effective in detecting clinical intellectual disability. Total IQ score was categorized according to the Arabic version into: intellectual disability (≤67), borderline intelligence (68-78), below average (79-88), average (89-110); above average, excellent and genius were 111-120, 121-131, and ≥132 respectively. SBITA was standardized for Arabic community with good reliability and validity, producing standardized scores with a mean of 100 and standard deviation of 16 points 8. In the current result, the SBITA confirmed that intellectually, all of the TBI adolescents are within borderline or above. IQs range from 78 to 83. Frequently, socialemotional profile is measured by VABSA. Several disabilities such as developmental delays, functional impairment, and learning disability are evaluated by the VABSA. It includes four subscales: Socialization, Daily Living Skills, Communication and Motor Skills. The mean total score of the Arabic VABSA was classified as: low adaptive behavior (≤69), below average (70-84), average (85-115); above average and high adaptive behavior were 116-130 and ≥131 respectively. In the current study, the VABSA scale indicated an adequate adaptive level of social-emotional skills with a total score range of from 81 to 88.
The presence of an emotion recognition deficit was determined first using the Toronto Alexithymia Scale (TAS-20). This is a selfassessment scale of 20 items, on a 5-point Likert scale. High points indicate a high degree of alexithymia (dissociation in social and emotional awareness and disrupted interpersonal interactions). TAS-20 has good psychometric properties in adolescents and adolescent samples and the measure provides a total score and three subscales scores. A total score of 61 is categorized as a recommended cut-off for the clinical alexithymia; while scores 52- 60 are moderate alexithymia; and non-alexithymic scores are below 52. The three subscales include: Difficulty Identifying Feelings (DIF), Difficulty Describing Feelings (DDF), and Externally Oriented Thinking (EOT).
Figure 1:Photograph samples of the basic facial expressions of emotion (Stimuli), using M-FEEST tests.
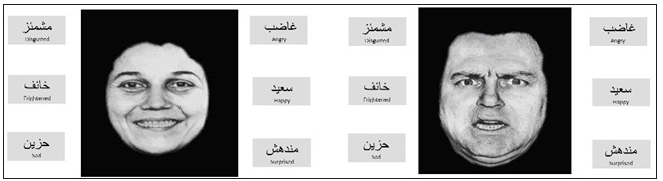
The basic emotions (fearful, surprised, disgusted, angry, sad and happy) were assessed using the Facial Expressions of Emotion Stimuli Tests (FEEST). The FEEST stimuli are well investigated for evaluating facial expression recognition. Each photograph was 11.5cm×10.5cm in size and was displayed on a computer monitor screen. Each emotion appeared 10 times in 10 different photographs. No photograph appeared more than once. Stimuli were displayed for 5 seconds, followed by a 5-second interval in which the screen was blank, and during that interval, patients had to select which emotional label best defined the emotion shown. Facial expressions of emotion stimuli were adapted in a previous Saudi study [5]. All photographs were Modified (M-FEEST) and were edited to focus on facial features, and to make the photos accepted culturally (Figure1). The emotional labels were showed in Arabic black bold font, with each photograph. Total scoring was based on the correct answers in targeted emotions. The score ranged from 0 to 60.
The approach here was to select a small number of TBI patients in order to assess them as an individual case and then attempt to generalize across the individual cases. On the first outpatient visit, regularly, each patient is tested on SBITA and VABSA. Parents who agree to their adolescent’s participation were followed at the second outpatient visit by additional assessments, mainly the TAS-20 and FEEST. Each enrolled adolescent was evaluated individually in a quiet clinic that was designed to observe and assess TBI patients’ neuropsychologicaly.
Results
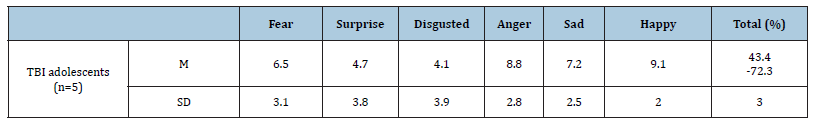
The current findings observed that the adolescents with TBI showed clinical alexithymia or a moderate level of alexithymia according to TAS-20. All of the five cases here reported high mean scores for all three subscales of the TAS-20: DIF, DDF, and EOT as well as for the total score. This finding shows the frequency of emotion recognition deficits after TBI according to the alexithymia scale (Table 2). The other part of this investigation highlighted an obvious limitation of emotion recognition. The performance of all five patients in the M-FEEST test was below the expected level. Patients decoded the emotional facial expression of happy, anger then sad better than the other emotional facial expressions. The lowest performances for decoding emotion expression tasks were for disgusted, surprise then fear (Table 3).
Table 1:Details of the five TBI adolescents included in the study.
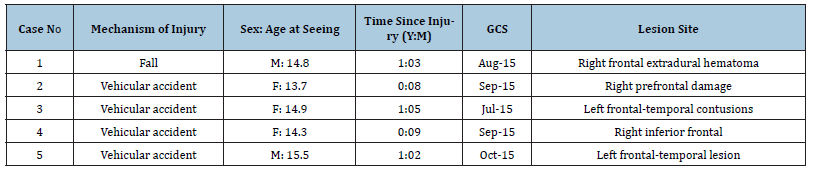
Table 2:The emotion recognition deficits as determined by the Toronto Alexithymia Scale (TAS-20).
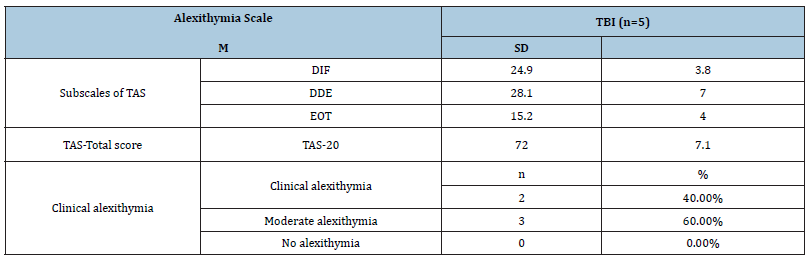
Table 3:Correct performance in recognizing emotions according to the M-FEEST (Max. score for the subscale=10 and for the total scale=60.
Discussion
This study provides its finding from TBI adolescents from 8 months up to 15 months from the time of injury. Investigating recent TBI patients allowed for an observation of emotion perception impairments before a fully functional recovery [5]. However, the current finding provides overall support for the hypothesis that TBI adolescents exhibit limitations on visual tasks of facial expression recognition. Despite such relationship between brain injury in adolescent hood and lasting emotional disturbance, there was little attention paid to this and few scientific investigations within this area when compared to the availability of data for adult brain injury.
The sample of this study includes only the moderate and severe TBI according to the GCS. However, even mild TBI may damage an adolescent’s emotion recognition abilities, causing deficits that could continue undiagnosed for several years. Therefore, clinical psychologists at the rehabilitation sittings should guarantee sufficient follow-up with assessments of neuropsychology domains to detect adolescents at risk of developing socialemotional disruption and help them receive suitable psychological rehabilitation interventions.
The recent studies that focused on why TBI adolescents experience post-injury emotional problems have developed two separate theoretical explanations. The first acknowledges the centrality of cognition in our processing of affect. Accordingly, TBI adolescents experience post-injury emotional difficulties due to an impairment in their executive function. Such an impairment could be manifested as impaired visual or verbal processing speed, limitation of attention and concentration, and impaired memory [9]. The second theoretical explanation highlights the existence of specific skills in reading emotional information and highlights the role of emotional-cognitive processing, which depends on the skill of correctly recognizing emotional expression as conveyed by others. For example, some studies such as Dennis and her colleagues [10] show that TBI can result in general emotion recognition difficulties affecting both emotive communication and facial expression.
Conclusion
As a conclusion, deficits in recognizing emotion will possibly continue undiagnosed when general psychological assessments such as IQ are used alone. It is, therefore, important to provide valid and sophisticated neuropsychological assessments to evaluate emotion recognition abilities in order to target these cognitive abilities in the rehabilitation intervention program. Within the rehabilitation sitting, early detection of an adolescent with neuropsychological limitations and subsequent treatment involving a team of professionals could make reasonable improvements [7]. It is worth mentioning here that some important variables such as injury severity and time since injury were not controlled. Future investigations with large sample size, therefore, are needed to overcome the current study limitations. Continued research is necessary to understand the impact of pediatric brain injury on emotional behavioral outcomes in Saudi communities.
References
- Alhabdan S, Zamakhshary M, AlNaimi M, Mandora H, Alhamdan M, et al. (2013) Epidemiology of traumatic head injury in children and adolescents in a major trauma center in Saudi Arabia: implications for injury prevention. Ann Saudi Med 33(1): 52-56.
- Yeates KO (2013) Social outcomes in pediatric traumatic brain injury: Perspectives from social neuroscience and developmental psychology. J Int Neuropsychol Soc 19(5): 493-496.
- Yeates KO (2010) Mild traumatic brain injury and postconcussive symptoms in children and adolescents. J Int Neuropsychol Soc 16(6): 953-960.
- Hanten G, Cook L, Orsten K, Chapman SB, Li X, et al. (2011) Effects of traumatic brain injury on a virtual reality social problem-solving task and relations to cortical thickness in adolescence. Neuropsychologia 49(3): 486-97.
- Alqahtani M (2015) An investigation of emotional deficit and facial emotion recognition in traumatic brain injury: A neuropsychological study. Postępy Psychiatrii i Neurologii 24(4): 217-224.
- Alqahtani M, Altamimi N (2016) Code of ethics and professionalism in light of cultural competency: a guideline for saudi psychologists, supervisors, and trainees. Psychol Stud 61(2): 103-112.
- Alqahtani M, Wahaas S, Mahmoud A (2010) Cognitive and behavioral development profile of a Saudi girl with Fragile X syndrome. Neurosciences (Riyadh) 15(2): 113-116.
- Alqahtani M (2016) Neurobehavioral outcomes of school-age children born preterm: a preliminary study in the Arabic community. J Pediatr Neonat Individual Med 5(2): 1-9.
- Anderson V, Beauchamp MH, Yeates KO, Crossley L, Hearps SJ, et al. (2013) Social competence at 6 months following childhood traumatic brain injury. J Int Neuropsychol Soc 19(5): 539-550.
- Dennis M, Agostino A, Taylor HG, Bigler ED, Rubin K, et al. (2013) Emotional expression and socially modulated emotive communication in children with traumatic braininjury. J Int Neuropsychol Soc 19(1): 34-43.
© 2019 Mohammed M J Alqahtani. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






