- Submissions

Full Text
Research in Pediatrics & Neonatology
Clinico - Haematological Profile and Composite Platelet Index in Paediatric Dengue Illness. A Retrospective Study
Srinivasa Murthy Doreswamy1*, Vani Krishnamurthy2 and Rakesh Skater2
1 Department of Pediatrics, JSS Medical College, JSS University, India
2 Department of Pathology, JSS Medical College, JSS University, India
*Corresponding author: Dr. Srinivasa Murthy Doreswamy, Department of Pediatrics, JSS Medical College, JSS University, #70, Prakruthi, BEML 2nd Stage, Rajarajeshwari Nagara, Mysuru, Karnataka, India-570022
Submission: July 30, 2018; Published: October 15, 2018

ISSN: 2576-9200 Volume3 Issue2
Abstract
Background: Dengue illness is a common devastating epidemic in pediatric population. Fever, Thrombocytopenia, hypovolemic shock and bleeding are the common manifestations. Platelet indices are now increasingly being reported by the haematology labs which has shown promise as predictor of bleeding. We have derived a composite index which has a potential to be a better predictor of bleeding in dengue illness.
Objective: Primary objective was to describe the clinic haematological profile in serologically proved dengue infection in children. Composite platelet index (CPLI) was calculated by multiplying platelet count (decimals) with Mean platelet volume.
Material and methods: This was a retrospective study with data of children admitted for dengue illness collected between January 2015 and October 2015. We have studied a total of 117 children.
Results: Median (IQR) age was 9 (6-13) years. 34.1% of the patients had hypotension, 20% had bleeding manifestation and 2.4% developed haemorrhagic shock. Case fatality rate was 0.8%. 74.5% had thrombocytopenia. Both platelet and white cell counts were low in 30.9% of our patients. Median (IQR) CPLI in our patients was 13.5 (6.6-23.1) and in those with mucosal bleed or haemorrhagic shock was 6 (3-9.3).
Conclusion: About one quarter of pediatric dengue patients will not have thrombocytopenia at admission. Composite platelet index will be low in patients with mucosal bleeding or haemorrhagic shock.
Keywords: Pediatric dengue; Hematological profile; Composite platelet index
Introduction
Dengue infection is a devastating annual epidemic illness in India. It is seen across all the ages and has high mortality in paediatric population [1]. The typical clinical feature in paediatric dengue illness is biphasic fever and thrombocytopenia with variable involvement of other systems. Infection initiates prompt immunological response which at times lead to activation of cytokine mediated hemodynamic instability. Two recognised pathogenic mechanisms of death in severe dengue illness are capillary leak induced hypovolemic shock and bleeding leading to haemorrhagic shock [2-4].
Haematological system is early and commonly affected in Dengue infection. Most commonly affected cell line is that of platelets which is either consumed or its production depressed, leading to thrombocytopenia [5]. Petechiae is common in paediatric dengue illness. It is neither specific nor pathognomonic of Dengue infection. However, like many other viral haemorrhagic fevers with petechiae, some of the children with dengue illness can progress to mucosal or internal bleeding leading to death. Variable amount of bone marrow suppression has been described in dengue infection [6]. We found very few studies with detailed description of both clinical and haematological profile in paediatric dengue illness.
There are several studies looking at the predictors of bleeding in dengue illness. Recently there has been increased interest in platelet indices as predictor of bleeding [7]. This is further fuelled by more and more labs utilizing high fidelity automated haematology analysers which are capable of reporting platelet indices. With several studies shedding light on the platelet indices and evidence of bone marrow suppression in dengue infection, we revisited the relation between them and their possible role in bleeding.
Increased mean platelet volume (MPV) suggests active bone marrow and young platelets in the circulation [8,9]. This could be a possible protective factor against bleeding due to thrombocytopenia. To factor in this possible advantage, we propose a composite platelet index (CPLI) which is the product of platelet count and MPV. We believe that low CPLI could be a more sensitive predictor of bleeding than low platelet counts alone.
Objectives
Primary objective: To describe the clinico -haematological profile in serologically proved dengue infection in children.
Secondary objectives: To compute composite platelet index (CPLI) in all children with dengue infection and compare it between children with and without bleeding in dengue infection.
Methods
Study design: This is a retrospective study undertaken in the department of Pathology and Pediatrics in a tertiary care hospital. Study period was between January 2015 and October 2015.
Subjects: All children aged less than 15 years and admitted to paediatric ward with a diagnosis of dengue infection. Dengue infection was diagnosed by clinical history of fever and one of the dengue serology like NS1, IgM or IgG being positive.
Data collection: Clinical data -the list of children with diagnosis of dengue infection as per WHO classification of 2009, during the study period was obtained from medical record section. The case notes were retrieved, and the necessary clinical data was obtained. Hypotension was defined as systolic blood pressure below 50th centile for the age and gender as per the WHO criteria [10]. Shock was diagnosed if the patient had a capillary refill time of greater than 3 seconds and / or low volume pulse with hypotension and needed fluid bolus or inotropes for improvement of blood pressure.
Haematological data - The order numbers of the haematological investigations requested at the time of admission were noted. These order numbers were retrieved from the lab information system of the hospital and the haematological data was obtained. These data were recorded on a predesigned case report form in Microsoft excel.
Sample collection: Two ml of blood sample is obtained by venepuncture at admission. The sample is collected in ETDA tube and transported to the lab via chute system. The EDTA sample is analysed using Sysmex 1000 within one hour of receipt.
Statistics: Sample size: We included all children admitted for treatment of dengue infection during the study period.
Analysis: Continuous variables are either reported as mean and standard deviation or median and inter quartile range depending on their distribution. Categorical data are summarised as total numbers and proportions.
Results
We had a total of 117 admissions with the diagnosis of Dengue infection. Ninety-four of them had haematological evaluation done at admission. Rest were investigated elsewhere before admission.
Median (IQR) age of our patients was 9 (6-13) years. Median (IQR) duration of fever before admission was 5 (4-7) days. All the patients were in febrile phase of illness at admission and length of stay in the hospital was 6 (5-9) days. Most common serological positivity was for Dengue IgG followed by NS1 antigen. 20% of patients had bleeding manifestations. 2.4% developed haemorrhagic shock. 5.7% of the patients had platelet transfusion and 2.4% had platelet transfusion for low platelet count alone without any bleeding manifestations. 2.4% of our patients got discharged against medical advice due to financial reasons. The mortality rate was 0.8%. Table 1 depicts the detailed clinical characteristics of our patients.
Table 1:Clinical and haematological profile in paediatric dengue illness.

Complete haematological profile at admission was available for 94 patients. 20 patients had bleeding manifestations and only 16 of them had haematological profiles. Of the 7 patients with mucosal bleed, haematological profile was available only in 4 patients. Table 2 depicts the haematological variables with their proportions. Mean (SD) Haemoglobin was 12.6 (2.2) gm/dl, Haematocrit was 37.8 (6.1) % and RBC count was 4.9 (0.7) million/cu mm. Median (IQR) WBC count was 6430 (4190-9790)/cumm.
Table 2:Haematological profile in paediatric dengue illness.
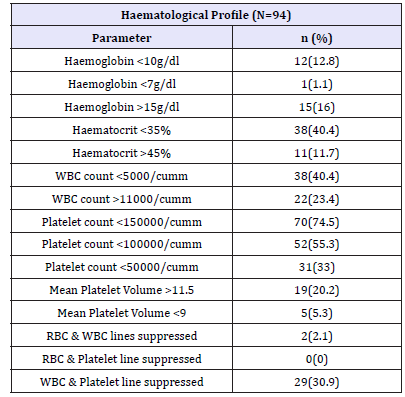
Only 26% of our patients had platelet count above 150000/ cumm and rest of them had thrombocytopenia. Median (IQR) platelet count was 115000 (42000–209000). Mean (SD) MPV (Mean platelet volume) was 10.6 (1.1) and mean P–LCR (platelet large cell ratio) was 30.2 (9.1).
A composite platelet index (CPLI) was calculated by multiplying platelet count (in decimal figures) with MPV. Median (IQR) CPLI in dengue patients with no bleeding was 13.5 (6.6–23.1) where as normal value would range between 13.5 and 46. In patients with any bleeding manifestation, Median (IQR) CPLI was 14.8 (7.4–18.6), in those with skin bleeding alone, it was 17 (12–22) and in children with mucosal bleeding or haemorrhagic shock, Median (IQR) CPLI was 6 (3-9.3).
There were 31 (33%) children with reduced count in more than one cell indirectly suggesting bone marrow suppression. None of the children had reduced count in all the three cell lines.
Discussion
In this study, we have noted that one fifth of patients has some form of bleeding and 2.4% of them develop haemorrhagic shock. A study in Brazil have shown the incidence of petechiae, bleeding and hypotension in less than 1% of their subjects [11]. They also found thrombocytopenia only in one third of their patients compared to more than two third of our patients. The admission practice during study period could offer possible explanation for this difference. The recent guidelines by WHO has prompted management of majority of the stable patients on outpatient basis itself.
Incidence of shock in paediatric dengue illness in a study reported from Taiwan is found to be similar to our study [12]. There are very few studies describing the haematological profile specifically in paediatric population alone. In an adult study, the incidence of neutropenia in dengue illness was found to be 11.8% [13]. Another comparative study between adult and paediatric dengue illness have reported the incidence of leukopenia in 51.9% of adults and 47.4% of paediatric patients [11]. In this study the cut off values for defining leukopenia is neutrophil count less than 4000/cumm. Our findings are similar to this study with leukopenia (WBC less than 5000/cumm) seen in 40.4%.
Decrease in two or more cell lines in the peripheral blood suggesting suppression of bone marrow has been reported in adult patients [14]. Decrease in the RBC count alone cannot be entirely attributed to suppression of bone marrow because of high incidence of anaemia in Indian population [15]. In contrast, decrease in the white cell count is generally considered to be due to decreased production in the bone marrow suggesting marrow suppression. In our study, we have found 33% of the study subjects having decreased count in more than one cell lines. In vitro and animal studies have reported bone marrow suppression in dengue illness [13,16]. This phenomenon needs further studies to determine if there is a sub category of patients with bone marrow suppression who may have different severity of illness, outcome and may benefit from specific treatment strategy.
While analysing the different haematological parameters for predicting bleeding, we recognised that taking single parameter into account would be insufficient. Hence we computed the composite platelet index to factor in the advantage of young platelets in preventing bleeding. In our study we found petechiae to be unrelated to platelet count or CPLI. In contrast, in patients with mucosal or internal organ bleed, CPLI was found to be very low. The statistical significance of this finding in our study is difficult to interpret as the number of patients with mucosal or internal bleed were too less. Future studies which can recruit larger sample would help to determine the significance of this potentially useful index.
Conclusion
Quarter of the paediatric patients with dengue illness do not have thrombocytopenia and one third have indirect evidence of bone marrow suppression. Composite platelet index will be low in patients with mucosal or internal bleeding compared to no bleeding or skin bleeds.
Funding
This study was self-funded. No funding agencies have supported.
Ethics
This study was approved by institutional ethical committee.
References
- Bashir AB, Saeed OK, Mohammed BA, Ageep AK (2015) Role of platelet indices in patients with dengue infection in red sea state, Sudan. IJSR 4(1): 1573-1576.
- Elsewefy DA, Farweez BA, Ibrahim RR (2014) Platelet indices: consideration in thrombocytopenia. Egyptian J Haematol 39(3): 134-138.
- Vaughn DW, Green S, Kalayanarooj S, Innis BL, Nimmannitya S, et al. (1997) Dengue in the early febrile phase: viremia and antibody responses. J Infect Dis 176(2): 322-330.
- Young PR, Hilditch PA, Bletchly C, Halloran W (2000) An antigen capture enzyme-linked immunosorbent assay reveals high levels of dengue virus protein NS1 in the sera of infected patients. J Clin Microbiol 38(3): 1053-1057.
- Jayashree K, Manasa GC, Pallavi P, Manjunath GV (2011) Evaluation of platelets as predictive parameters in dengue fever. Indian J Hematol Blood Transfus 27(3): 127-130.
- Narayanan M, Aravind MA, Ambikapathy P, Prema R, Jeyapaul MP (2003) Dengue fever -clinical and laboratory parameters associated with complications. Dengue Bulletin 27: 108-115.
- Tathe SS, Chincholkar VV, Kulkarni DM, Nilekar SL, Ovhal RS, et al. (2013) A study of NS1 antigen and platelet count for early diagnosis of dengue infection. Int J Curr Microbiol App Sci 2(12): 40-44.
- Cines DB, Bussel JB, McMillan RB, Zehnder JL (2004) Congenital and acquired thrombocytopenia. Hematology Am Soc Hematol Educ Program 1: 390-406.
- Xu RL, Zheng ZJ, Ma YJ, Hu YP, Zhaung SH (2013) Platelet volume indices have low diagnostic efficiency for predicting bone marrow failure in thrombocytopenic patients. Exp Ther Med 5(1): 209-214.
- Bashir AB, Mohammed BA, Saeed OK, Ageep AK (2015) Thrombocytopenia and bleeding manifestations among patients with dengue virus infection in Port Sudan, Red Sea State of Sudan. J Infect Dis Immun 7(2): 7-13.
- De Souza LJ, Pessanhaa LB, Mansur LC, De Souza LA, Ribeiro MBT, et al. (2013) Comparison of clinical and laboratory characteristics between children and adults with dengue. Braz J Infect Dis 17(1): 27-31.
- Kittigul L, Pitakarnajankul P, Sujirarat D, Siripanichgon K (2007) The differences of clinical manifestations and laboratory findings in children and adult with dengue virus infection. J Clin Virol 39(2): 76-81.
- La Russa VF, Innis BL (1995) Mechanisms of dengue virus-induced bone marrow suppression. Baillieres Clin Haematol 8(1): 249-270.
- Wang C, Lee I, Su M, Lin HI, Huang YC, et al. (2009) Differences in clinical and laboratory characteristics and disease severity between children and adults with dengue virus infection in Taiwan. Trans R Soc Trop Med Hyg 103(9): 871-877.
- Patel N, Gunjana G, Patel S, Thanvi R, Sathvara P, et al. (2015) Nutrition and health status of school children in urban area of Ahmedabad, India: Comparison with Indian Council of Medical Research and body mass index standards. J Nat Sci Biol Med 6(2): 372-377.
- Noisakran S, Onlamoon N, Hsiao HM, Clark KB, Villinger F, et al. (2012) Infection of bone marrow cells by dengue virus in vivo. Exp Hematol 40(3): 250-259.e4.
© 2018 Srinivasa Murthy Doreswamy. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






