- Submissions

Full Text
Research in Pediatrics & Neonatology
“Triple-Tube-Ostomy” Technique for Management of Duodenal Injuries: A Systematic Review and Meta-Analysis
Mohammad Al-Karsify1,2, Hussein Abou-Abbass1, Fadi Iskandarani3 and Hisham Bahmad1,4*
1Faculty of Medicine, Beirut Arab University, Lebanon
2Department of General Surgery, Rafik Hariri University Hospital, Lebanon
3Pediatric Surgery Division, Rafik Hariri University Hospital, Lebanon
4Department of Anatomy, Cell Biology, and Physiological Sciences, Faculty of Medicine, American University of Beirut, Beirut, Lebanon
*Corresponding author: Hisham Bahmad, MD, MSc, Research Fellow, Faculty of Medicine, American University of Beirut, Beirut-Lebanon; Tel: 961- 70-607690; E-mail: hfbahmad@gmail.com
Submission: April 20, 2018;Published: May 23, 2018

ISSN: 2576-9200 Volume2 Issue2
Abstract
Background: Isolated duodenal injury following blunt or penetrating trauma remains an extremely rare and one of the most challenging hitches confronting trauma surgeons. Triple-tube-ostomy (TTO) technique involving gastrostomy, reverse duodenostomy, and feeding jejunostomy tubes insertion has shown promising results during conservative management of duodenal injuries.
Objective: We aim through this paper to report a successfully managed case of isolated incomplete transverse duodenal injury managed by TTO technique in a 14-year-old boy who presented with severe abdominal pain, one day after sustaining ablunt abdominal trauma due to fall from height. In addition, we aimed to systematically review the literature for the usage and outcomes of the TTO surgical procedure, and evaluate its efficiency and effectiveness in the management of duodenal injuries.
Data Sources: OVID/Medline, PubMed, and Scopus databases were lastly searched on December 8th, 2016 to identify all published research studies on duodenal injuries treated by this surgical technique.
Study Selection: Studies reporting cases of duodenal injuries that were managed by TTO were warranting inclusion.
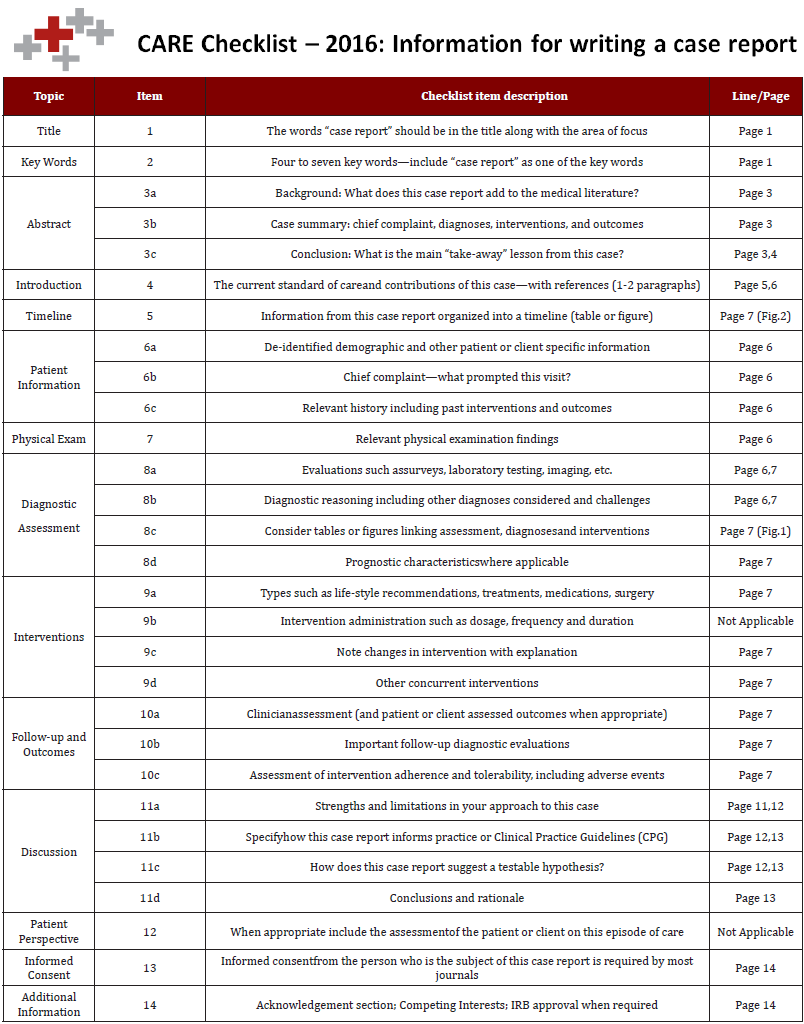
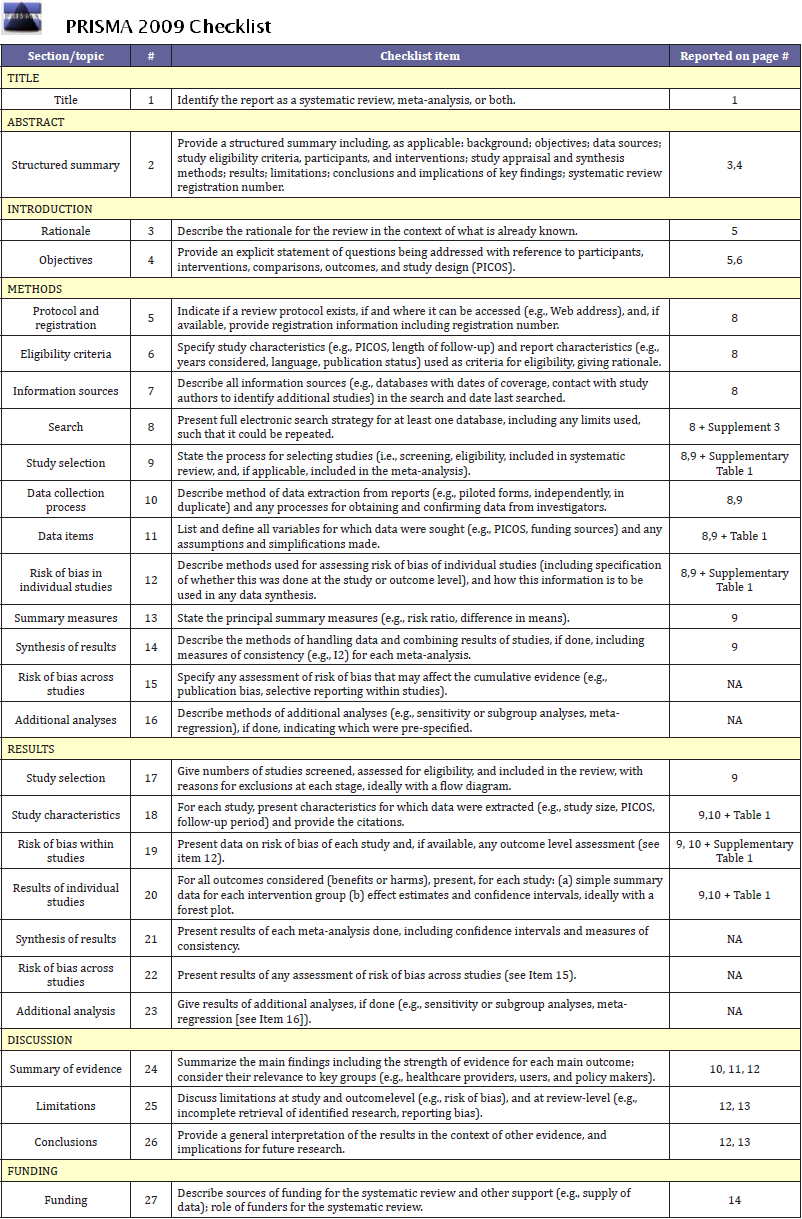
Data Extraction and Synthesis: Both CARE and PRISMA guidelines were followed for conduction and reporting of this study. Throughout the whole review process, two reviewers worked independently and in duplicate to screen titles, assess full texts for eligibility, and abstract data.
Results: Six articles were included in this review. Sixty five cases were reported to have undergone TTO in world literature. Majority of the cases were performed after surgical repair of giant duodenal ulcers, only 2 cases were reported due to perforations following trauma. While majority of cases had uneventful recovery, complications such as wound infections and dehiscence were reported. Mean length of hospital stay was found to be 20.5 days. Mortality occurred in 3 cases.
Conclusion and Relevance: The positive outcomes of our reported case and the structured evaluation of the published studies suggest effectiveness of usage of “triple-tube-ostomy” surgical procedure for management of duodenal injuries. However, further studies are needed to assess the usage of this technique in management of duodenal injuries in comparison to other classical surgical techniques.
Keywords: blunt trauma, abdomen, isolated transverse duodenal transaction, transpyloric “triple-tube-ostomy” decompression, case report, systematic review
Introduction
In contrast to the liver and spleen, injuries to the duodenum are much less frequent, reported as 0.2% of blunt trauma injuries [1,2], and comprising 0.2–3.7% of all trauma-related laparotomies [3]. What makes isolated duodenal injuries scarce is the fact that duodenal trauma is usually associated with one to four other abdominal organ injuries [2,4].
Furthermore, due to its anatomical position, the “protected” retroperitoneal location of the duodenum limits the chance of injury but makes early diagnosis and treatment a difficult task [5,6]. Add to this diagnostic dilemma is the frequency of associated intra-abdominal and/or multisystem injuries such as concomitant injuries that affect the liver in about 17%, pancreases, colon and small bowels each in about 11% [7,8], which can mask subtle physical and radiographic diagnostic signs found in isolated blunt injuries to the duodenum [9]. Hence, diagnosis is challenging, particularly in the setting of acute blunt trauma, since symptoms and signs resulting from these injuries may not be obvious. Additionally, there are currently no modalities that allow the clinician to diagnose duodeno-pancreatic trauma accurately.
Conventional surgical management options of duodenal injuries vary according to the duodenal organ injury scale (DIS), which relies upon an injury classification system from the American Association for the Surgery of Trauma (AAST) [10], from conservative non-operative management to surgical intervention. Surgical intervention ranges from simple debridement and primary closure (duodenorrhaphy) of injured duodenum to much more complex procedures, such as resection and primary anastomosis of the damaged portion, pyloric exclusion [11], duodenal decompression [3,12,13], or pancreaticoduodenectomy [14].
Triple-tube-ostomy (TTO) have been done in several cases, but not yet recommended following duodenal injury repair. TTO entails gastrostomy, reverse duodenostomy, and feeding jejunostomy tubes insertion. Gastrostomy and reverse duodenostomy serve to decrease tension at the repair site and help drain both gastric and duodenal secretions allowing time for anastomosis to heal, thus preventing complications. Other than intraabdominal abscesses and pancreatitis, duodenal fistulas/leak are the most life threatening postoperative complications which may occur in about 7% of cases [7,8].
Hereby, we present a case of a 14-year old boy who was diagnosed to have isolated incomplete transverse duodenal injury due to blunt abdominal trauma, treated with duodenorrhaphy and complicated by a postoperative leak managed by the promising “triple-tube-ostomy” technique for decompression in a transpyloric approach. We also present a systematic review of the relevant literature conducted to describe all prior case reports and studies where this surgical technique was used in managing patients with duodenal injuries, and to determine whether it is efficient to be used in such cases.
Case Presentation
A 14-year-old Lebanese boy, previously healthy, presented to the emergency department of Rafik Hariri University Hospital, one of the tertiary care centers in Beirut, with diffuse abdominal pain and distension, 48 hours after sustaining a blunt abdominal trauma due to fall from height of about 4 meters. Patient reported that the pain had been increasing in intensity over the last 48 hours, stabbing in nature, radiating to the back, not relieved by any medication or position and associated with obstipation and anorexia. High-grade fever was also reported, without chills. No nausea, vomiting or any other associated symptoms were reported.
At presentation, patient was hemodynamically stable with blood pressure of 110/90mmHg, pulse rate of 96 beats per minute, respiratory rate of 18 breaths per minute, body temperature of 36.8℃ and O2 saturation of 99%. On physical examination, abdomen was rigid with diffuse rebound tenderness and normal bowel sounds. No pulsating masses were noted in the abdomen. Otherwise, the rest of physical examination was normal. Total leukocyte count on presentation was 13,000cells/μL (83% neutrophil count), otherwise normal laboratory blood tests (hemoglobin, hematocrit, electrolytes, creatinine, blood urea nitrogen, liver enzymes, amylase, lipase, and C-reactive protein). Plain abdominal and chest radiographs were normal. Computed Tomography (CT) of the abdomen and pelvis was done with IV contrast showing gas and fluid in the right retroperitoneal space with free fluids in the perihepatic, perisplenic and pelvic areas. In addition, hairline hypodensity was seen at the level of the body of duodenum. Patient was thus admitted for emergency laparotomy and suspected duodenal injury repair. Exploratory laparotomy was performed for primary repair of third portion transverse duodenal rupture - duodenorrhaphy, with insertion of Hemovac drain in the periduodenal region. Patient was successfully discharged after recovery on the 3rd postoperativeday (POD) after tolerating PO intake.
Figure 1: (A) Upper GI series radiography with gastrografin swallow showing significant leak of the contrast material from the lower 2nd portion of the duodenal loop at its junction with the 3rd portion. Two fistulous tracts are demonstrated from this area. The 3rd and 4th portions of the duodenal loop could not be filled. (B) Upper GI series radiography with gastrografin swallow repeated 4 weeks following “triple-tube-ostomy” decompression surgical procedure. Contrast material was injected through gastrostomy tube with no evidence of leak or any fistula from the duodenum. The duodenal loops and upper small bowels show no abnormalities.
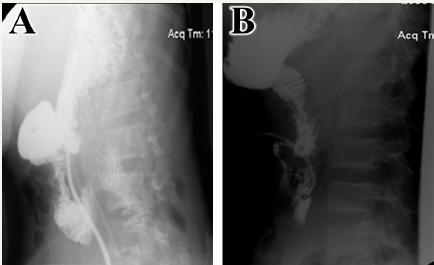
The patient returned to the emergency department with sharp abdominal pain on 7th POD. Vital signs showed an elevated body temperature of 38.3℃, tachypnea with 22 breaths per minute, tachycardia with heart rate of 102 beats per minute and hypotesion with a blood pressure of 90/60 mmHg. Patient’s laboratory results were normal except for an elevated white blood cell count of 18,000 cells/μL with 90% neutrophilic count and 11% band cells. Since a leak was suspected, upper gastrointestinal (GI) series was done using gastrografin and showed significant leak of the contrast material from the lower second portion of the duodenal loop at its junction with the third portion (Figure 1A). Patient was urgently re-operated with “triple-tube-ostomy” decompression procedure involving reverse tube duodenostomy, tube gastrostomy, and feeding jejunostomy. Feeding through jejunostomy started on 3rd POD. Following the second operation, patient showed clinical improvement with normal laboratory values. Gastrografin upper GI series was repeated 4 weeks later showing no evidence of leak or any fistula from the duodenum (Figure 1B). Patient was discharged home on 28th POD following the removal of all –ostomy tubes. Currently, the patient returned to his usual state of health prior to the injury, and had an uneventful recovery. Figure 2 represents the case time line.
Figure 2: Study case time line.

Methods
Data sources and searches
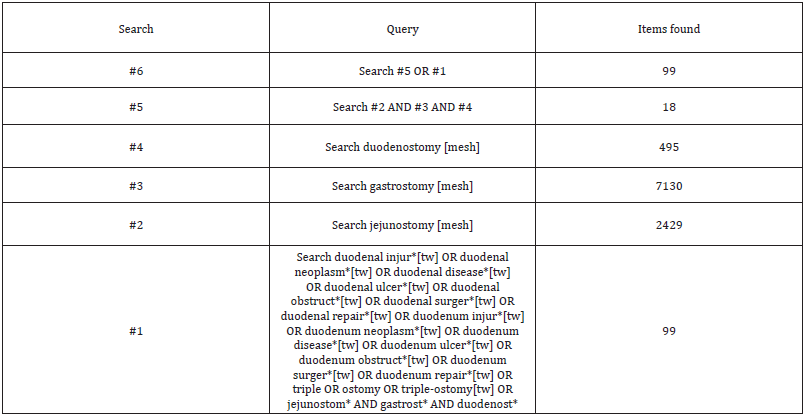
This paper was reported in compliance with CAseREports (CARE) and Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines for reporting case reports and systematic reviews (Supplements 1 & 2). Systematic review of the relevant English literature was conducted encompassing studies documenting the use of “triple-tube-ostomy” technique to manage duodenal injuries of any cause. A comprehensive search strategy was developed by searching 3 databases, PubMed, OVID/Medline and Scopus, for relevant articles since inception up to December 8th, 2016. MeSH terms, keywords and combinations related to the topic were used to search the databases comprehensively: “duodenum”, “duodenostomy”, “jejunostomy”, “gastrostomy”, and “triple-tubeostomy”. Complete search strategy is provided in Supplement 3.
Ovid MEDLINE Search Strategy
Database: Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) < 1946 to Present >
Search Strategy:
-----------------------------------------------------------------------
1 exp jejunostomy/ (2553) [MeSH Term]
2 exp gastrostomy/ (7451) [MeSH Term]
3 exp duodenostomy/ (513) [MeSH Term]
4 1 and 2 and 3 (18)
5 (((duoden* adj3 (injur* or perforat* or neoplasm* or disease* or ulcer* or obstruct* or surger* or repair* or triple or ostom*)) or jejunostomy* and gastrost* and duodenost*).mp. [mp=title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] (50) [Keywords and combinations]
6 4 or 5 (50)
***************************
PubMed Search Strategy
Inclusion Criteria
Articles were considered eligible if they described the usage of “triple-tube-ostomy” technique in the management of duodenal injuries. Abstracts, case reports and other studies not including duodenal injuries or demonstrating usage of this decompression procedure in injuries other than the duodenum were excluded. Papers discussing the usage of duodenal decompression alone were also excluded.
Study review
Two reviewers independently and in duplicate screened study titles and abstracts for relevance, after which full-texts were retrieved and evaluated for eligibility of the inclusion criteria. In case of disagreement, a third reviewer was consulted.
Data extraction and synthesis
For studies that fulfilled the inclusion criteria, reviewers abstracted the data into a specifically designed and piloted data extraction form for the purpose of this review. Data abstracted included the manuscript title, first author (s), year of publication, study design, study time period, site of the study, sample size, patient characteristics (age, sex, cause of injury, complications and mortality. Supplementary Table 1 presents the data of all the articles abstracted.

Data analysis
The abstracted data were organized into descriptive table where basic statistical tests were performed. Categorical variables were represented by numbers and percentages, continuous variables were presented by means and standard deviations.
Ethical approval
A written informed consent was obtained from the patient’s father for publication of this case report and accompanying images. No IRB approval was required for the purpose of the systematic review.
Results
Results of the search
In total, 221 articles were identified using the primary literature search. Thirty-two duplicate articles were removed using the EndNote referencing software to remain with 189 articles (71 from Scopus, 68 from PubMed and 50 from OVID) being eligible for title and abstract screening. During this stage, 174 articles were excluded. As a result, 15 articles were found eligible and selected for full-text screening. At the end of the full-text screening stage, 6 articles were relevant and reported in this review. Figure 3 presents the study screening flow processes and reasons for full text exclusions. Among the 6 studies selected [3,13,15-18], 2 prospective, 1 retrospective and 3 case studies were published between 1988 and 2016.
Figure 3: PRISMA flow diagram depicting study flow process.

Study Setting, time periods and participants
Three studies were conducted in India [3,13,18], one study in United Kingdom [17], one in Georgia [15] and one study in Japan [16]. TTO was reported to be used in 4 studies following giant duodenal ulcers [13,15,17,18], 1 following iatrogenic duodenal perforation after ERCP [16] and 1 case of duodenal perforation following blunt abdominal trauma [3]. The oldest reported usage of TTO was in 1985, in Georgia [15].
In total, 64 cases of TTO’s were reported in literature in addition to our case, of which, 48 males and 17 females underwent this procedure. Age groups ranged between 14–77 years, with a mean of 51.1±14.6 years. Table 1 shows all study characteristics and abstracted data.
Length of hospital stay
The mean length of stay in patients that underwent TTO was 20.5±14.9 days. Thirty one (49.2%) cases had a hospital stay less than 15 days, 11 (17.4%) cases had a hospital stay between 15 -20 days and another 11 (17.4%) patients between 20 -30 days. Two cases (3.2%) had a hospital stay between 25 and 30 days, while 8 (12.6%) cases had a hospital stay more than 30 days. Lengthiest hospital stay was reported to be 88 days postop.
Complications and mortality
Few complications were reported after TTO. Wound infection, dehiscence and burst abdomen were reported only in studies performed in India in nearly all cases reported, and so was mortality [13,18]. Three cases were only reported dead, in which the causes were attributed to septicemia in 2 cases [13] and respiratory failure due to fulminant pulmonary TB in another case [18]. Additional complications included intra-abdominal sepsis in 4 cases; pneumonitis in 8 [18], pneumonia, upper gastro-intestinal bleed [17] and 1 episode of fever [3], each in one case.
sDiscussion
Duodenal injury following blunt abdominal trauma is an uncommon event that is usually associated with other abdominal organ injuries, such as hepatic (38%) or pancreatic (28%) [19], making isolated injury to the duodenum alone extremely rare. It represents around 2-20% of patients with blunt abdominal injury [20], and 0.2% of all blunt trauma injuries [1,2]. Here, we have described a case of isolated transverse duodenal injury treated initially by duodenorrhaphy then re-operated with “triple-tubeostomy” (TTO) decompression surgical technique due to leak. We have also evaluated, through systematic review of relevant English literature and meta-analysis of case studies published in this context, the extent of use of this technique to treat duodenal injuries of any cause.
Duodenal injuries are primarily caused by penetrating wounds (78%), such as gunshots and stab wounds [7], rather than blunt traumas (22%) [8]. Blunt injuries to the duodenum and pancreas are mainly caused by motor vehicle collisions (around 75 – 85%) [8,21], due to crushing of these organs between the vertebral column and steering wheel or seatbelt [7]. Other mechanisms of blunt duodenal and pancreatic injuries include falls and assaults [8,22,23]. In addition, giant duodenal ulcers complicated by perforation have been also reported to be causes of duodenal injury as well [13,15,17,18]. In our current systematic review and metaanalysis, majority of cases (59 out of 65), where TTO was used in the management of duodenal injuries, comprise surgical repair of giant duodenal ulcers perforation [13,15,17,18], whereas this technique was used in 3 other patients with iatrogenic duodenal perforation after ERCP 16 and 3 cases of duodenal perforation following blunt abdominal trauma, including our case [3].
As for morbidity and mortality rates associated with duodenal injury, studies have revealed a 14-20% mortality rate in penetrating injuries and 18-19% in blunt injuries [7,8]. Fifty percent of deaths reported are early, due to bleeding and hemorrhagic shock, while the other 50% are late, caused by complications including fistula formation, sepsis, and multiple organs failure [7,8]. Consequently, no single surgical procedure has yet been recommended to be used for duodenal injury repair, which carries minimal rates of postoperative complications. Surgical intervention in such cases usually ranges from simple debridement of the injured duodenum and primary closure (duodenorrhaphy) of the wound, to other complex procedures, including resection and primary anastomosis of the damaged portion, duodenal decompression using TTO [3,12,113], pyloric exclusion [11], or pancreaticoduodenectomy [14].
no single surgical procedure has yet been recommended to be used for duodenal injury repair, which carries minimal rates of postoperative complications. Surgical intervention in such cases usually ranges from simple debridement of the injured duodenum and primary closure (duodenorrhaphy) of the wound, to other complex procedures, including resection and primary anastomosis of the damaged portion, duodenal decompression using TTO [3,12,113], pyloric exclusion [11], or pancreaticoduodenectomy [14].
In our case, the patient was effectively managed by simple repair duodenorrhaphy followed by duodenal decompression using TTO technique. TTO comprises the insertion of a tube gastrostomy to decompress the stomach and to drain gastric secretions preventing them from reaching the duodenum, a reverse tube duodenostomy passed through the proximal jejunum reaching the second part of duodenum to decompress it and to drain bile, and an antegrade tube jejunostomy for enteral feeding since early feeding for supplementation of adequate caloric intake was found detrimental for early recovery [3]. This surgical procedure was originally described by Stone and Fabian in 1979 where only duodenal decompression was performed through reverse tube duodenostomy [24]. Time of initiation of insertion of gastrostomy tube and feeding jejunostomy as an addition to reverse tube duodenostomy could not be ascertained, but the earlier report of its use dates back to 1988 by Cranford et al. [15]. Cranford et al. [15] also performed vagotomy in order to decrease the gastric secretions to allow time for proper healing of the anastomosis site, a step that was not performed in later studies [15]. Advantages of TTO include but not limited to being rapid and requiring basic surgical experience. It is also cost-effective with least morbidity rates for managing those severely injured sick patients with favorable outcomes [3].
Limitations
Although this is the first paper to evaluate the effectiveness of usage of the TTO technique in preventing leak post duodenal injury repair, few limitations reside: firstly, the small sample size that was evaluated; second, the high rates of complications that were reported only in India especially wound infection; third and last, the fact that results of this study could not be compared to a matching group, thus opening the ground for future research to be done in this area.
Implications for Clinical Practice and Future Research
In conclusion, triple tube ostomy surgical technique is an effective option in assisting the management of duodenal injuries following trauma or duodenal ulcers perforations. Based on the pattern of few complications and very low mortality rates reported in literature, along with short length of hospital stay following this surgery, we advise the coupling of TTO technique to any definitive treatment in duodenal injury repair to prevent reoperation later due to complications, mainly leaks. In our opinion, TTO should be the first choice for managing high risk patients, until their condition stabilizes and are able to undergo definitive treatment. Besides, we recommend conducting further studies to assess the outcomes of this technique in management of duodenal injuries in comparison to other classical surgical techniques.
Acknowledgment
We would like to express our gratitude thanks to the patient and his family for permitting us to publish this case report; and Rafik Hariri University Hospital for their permission to disclose this information. We would also like to thank Faculty of Medicine at Beirut Arab University, for the guidance and support during preparation of this work.
Authors’ Contribution
MAK, HB and HAA worked on study conception and design. FI is the attending surgeon who operated the case. HAA developed the search strategy. HAA and HB screened titles for relevance and abstracted the data from the eligible full-text articles. MAK was responsible for reporting the clinical course of the case. HB, HAA analyzed the data and drafted the manuscript. MAK, HB, HAA and FI critically revised and edited the manuscript. All authors have read and approved the final draft.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available upon request for review by the Editor-in-Chief of this journal.
References
- Allen GS, Moore FA, Cox CS, Mehall JR, Duke JH (1998) Delayed diagnosis of blunt duodenal injury: an avoidable complication. J Am Coll Surg 187(4): 393-399.
- Ballard RB, Badellino MM, Eynon CA, Spott MA, Staz CF, et al. (1997) Blunt duodenal rupture: a 6-year statewide experience. J Trauma 43(2): 229-232.
- Bhattacharjee HK, Misra MC, Kumar S, Bansal VK (2011) Duodenal perforation following blunt abdominal trauma. J Emerg Trauma Shock 4(4): 514-517.
- Velmahos GC, Constantinou C, Kasotakis G (2008) Safety of repair for severe duodenal injuries. World J Surg 32(1): 7-12.
- Hong J, Wang SY, Qian L, Chen ZY (2015) Diagnosis and Treatment of Duodenal Injury: A Clinical Analysis. Hepatogastroenterology 62(139): 641-646.
- Torba M, Gjata A, Buci S, Troci A, Subashi K (2013) Delayed presentation of blunt duodenal injuries in children. Case report and review of literature. G Chir 34(4): 122-124.
- Asensio JA, Demetriades D, Hanpeter DE, Gambaro E, Chahwan S, et al. (1999) Management of pancreatic injuries. Curr Probl Surg 36(5): 325- 419.
- Asensio JA, Feliciano DV, Britt LD, Kerstein MD (1993) Management of duodenal injuries. Curr Probl Surg 30(11): 1023-1093.
- Pandey S, Niranjan A, Mishra S, Agrawal T, Singhal BM, et al. (2011) Retrospective Analysis of Duodenal Injuries: A Comprehensive Overview. Saudi J Gastroenterol 17(2): 142-144.
- Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Champion HR, et al. (1990) Organ injury scaling, II: Pancreas, duodenum, small bowel, colon, and rectum. J Trauma 30(11): 1427-1429.
- Seamon MJ, Pieri PG, Fisher CA, Gaughan J, Santora TA, et al. (2007) A Ten-Year Retrospective Review: Does Pyloric Exclusion Improve Clinical Outcome After Penetrating Duodenal and Combined Pancreaticoduodenal Injuries? J Trauma 62(4): 829-833.
- Ivatury RR, Gaudino J, Ascer E, Nallathambi M, Ramirez-Schon G, et al. (1985) Treatment of Penetrating Duodenal Injuries: Primary Repair vs. Repair with Decompressive Enterostomy/Serosal Patch. J Trauma 25(4): 337-341.
- Ali WM, Ansari MM, Syed Amjad Ali Rizvi, Rabb AZ, Tariq mansoor, et al. (2016) Ten-Year Experience of Managing Giant Duodenal Ulcer Perforations with Triple Tube Ostomy at Tertiary Hospital of North India. Indian Journal of Surgery 80(1): 9-13.
- Phelan HA, Minei JP (2005) Pancreatic trauma: Diagnostic and therapeutic strategies. Curr Treat Options Gastroenterol 8(5): 355-363.
- Cranford CA, Olson R, Bradley EL (1988) Gastric disconnection in the management of perforated giant duodenal ulcer. Am J Surg 155(3): 439-442.
- Fujikuni N, Tanabe K, Yamamoto H, Suzuki T, Tokumoto N, et al. (2011) Triple-tube-ostomy: a novel technique for the surgical treatment of iatrogenic duodenal perforation. Case Rep Gastroenterol 5(3): 672-679.
- Herrod PJ, Kamali D, Pillai SC (2011) Triple-ostomy: management of perforations to the second part of the duodenum in patients unfit for definitive surgery. Ann R Coll Surg Engl 93(7): e122-124.
- Lal P, Vindal A, Hadke NS (2009) Controlled tube duodenostomy in the management of giant duodenal ulcer perforation: a new technique for a surgically challenging condition. Am J Surg 198(3): 319-323.
- Jurkovich G (1996) Injury to the duodenum and pancreas. Trauma. Stamford, CT: Appleton & Lange, 573-594.
- Yutan E, Waitches GM, Karmy JR (2000) Blunt Duodenal Rupture. American Journal of Roentgenology 175(6): 1600-1600.
- Maggio P, Clark D (2016) in UpTo Date. In: Ted W Post, et al. (Eds.), UpToDate.
- Akhrass R, Yaffe MB, Brandt CP, Reigle M, Fallon WF, et al. (1997) Pancreatic trauma: a ten-year multi-institutional experience. Am Surg 63(7): 598-604.
- Ilahi O, Bochicchio GV, Scalea TM (2002) Efficacy of computed tomography in the diagnosis of pancreatic injury in adult blunt trauma patients: a single-institutional study. Am Surg 68(8): 704-707.
- Stone HH, Fabian TC (1979) Management of duodenal wounds. J Trauma 19(5): 334-339.
© 2018 Hisham Bahmad. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






