- Submissions

Full Text
Research & Investigations in Sports Medicine
Effect of Cupping Therapy on Skin Surface Temperature as Measured by Infrared Imaging
Cage SA1*, Singh G2, Trail LE3 and Warner BJ4
1The University of Texas at Tyler, USA
2The University of Texas at Tyler, USA
3The University of Texas at Tyler, UT Health East Texas, USA
4Grand Canyon University, USA
*Corresponding author:Cage SA, The University of Texas at Tyler, USA
Submission: May 20, 2024;Published: May 27, 2024

ISSN: 2577-1914 Volume10 Issue3
Abstract
Cupping therapy, an ancient healing practice with roots in diverse cultures worldwide, has gained popularity in recent years for its therapeutic benefits in treating numerous musculoskeletal conditions. In western medicine cupping therapy is used with the goal of achieving therapeutic effects including decreased musculoskeletal pain and increased regional and localized blood flow. To date, there does not appear to be any general guidelines for the prescription and application of cupping therapy. Nevertheless, cupping therapy has continued to grow in popularity in the sports medicine setting. One factor in the lack of consensus on best practices for the use of cupping therapy is a lack of high-quality studies with large sample sizes. Therefore, the purpose of this retrospective study was to assess the effects of cupping therapy on skin surface temperature in collegiate baseball players. Review of medical records found that 26 male baseball players (age 21±1 year) had undergone 134 treatments that yielded includable data. Players received cupping therapy if they reported to the athletic training staff complaining of subacute or chronic musculoskeletal pain. Once the treatment site was identified, the skin was prepared using a light layer of coconut oil. Plastic cups were then applied to the treatment site, and two pumps of air were removed from each cup with a handheld pump. Cups remained in place for 20 minutes before being removed. Skin surface temperatures were taken with an infrared camera before and after treatment, and at five-minute intervals during treatment. A paired samples t-test was performed to assess skin surface temperature differences before and after cupping therapy. A one-way ANOVA test was performed to assess changes in temperature of the central most cup over time. On average, players receiving cupping therapy experienced significant increases in skin surface temperature (Pre-Cupping=31.47±1.03 °C, Post-Cupping=33.57± 0.73 °C, t(266)=-19.233, p<.001). Additionally, significant temperature increases were noted at the center most cup during treatment. To the authors’ knowledge, the number of treatments assessed in this study was more than any study evaluating the effect of cupping therapy on skin surface temperature in the current literature. Cupping therapy produced an increase in skin surface temperature, which likely indicates an increase in localized blood flow. Future research should examine the relationship between skin surface temperature and therapeutic effects of cupping therapy.
Introduction
Cupping therapy is an ancient healing practice with roots in diverse cultures worldwide and has gained popularity in recent years for its therapeutic benefits in treating numerous musculoskeletal conditions, such as plantar fasciitis, lower back pain, neck pain, and sports-related muscular injuries [1-3]. Despite its increasing utilization, the precise mechanisms underlying the therapeutic effects of cupping therapy remains a subject of ongoing research and debate. Several theories have been proposed to explain the physiological effects of dry cupping therapy. These theories suggest that cupping therapy may lead to improvements in range of motion, exert analgesic effects, and enhance blood circulation [4-6]. However, the exact mechanisms through which cupping therapy exerts these effects are not yet fully understood and require further investigation [4]. Research on cupping therapy has highlighted the significance of blood flow in assessing its therapeutic effects [7,8]. The Release of Nitric Oxide Theory suggests that cupping therapy may lead to increased nitric oxide release, promoting vasodilation, and enhanced blood flow to treated areas [4]. Studies have indicated that dry cupping therapy can significantly boost peak skin flow, with the intensity of this effect depending on the treatment pressure and duration. Doppler Flowmetry was utilized to accurately measure the increased blood flow to an area in both pre- and post-cupping therapy, providing valuable data on the physiological changes induced by the treatment [8].
While increased blood flow is correlated with greater oxygen delivery to damaged tissue, the negative pressure generated by cupping therapy directly causes capillaries to dilate under the skin, often leaving behind ecchymosis and possible capillary rupture as side effects [9,10]. These side effects are often associated with the style of cupping, application, and frequency of cupping, prompting users to clearly define the intended goal of therapy [10]. This is most likely the reason professional athletes have begun using cupping therapy to recover after rigorous training, yet little information provides support on whether cupping therapy actually provides a performance advantage [11]. Further research into measuring blood flow may provide a deeper understanding of how cupping therapy can affect recovery and performance. Aside from Doppler Flowmetry, measuring skin temperature has also been theorized to be correlated with increased blood flow following cupping therapy [12,13]. In this study, we investigated the effect cupping therapy had on skin temperatures via infrared photography, both before, during, and after cupping therapy treatments.
Methods
Design
This study was conducted using a retrospective analysis of data collected review of electronic medical records compiled during treatment of collegiate baseball players at an NCAA Division II institution.
Participants
Subjects were identified for this study through review of electronic medical records that were regularly compiled by the treating athletic trainer. The documentation included skin surface temperatures intended to ensure that blood flow had increased following treatment. Measurements were taken before and after the intervention, using an infrared camera with smartphone interface (TC002 Thermal Camera, TOPDON USA, Rockaway, NJ) for skin surface temperatures. A total of 26 male baseball pitchers (age 21±1 year) had undergone 134 treatments that yielded includable data.
Data collection
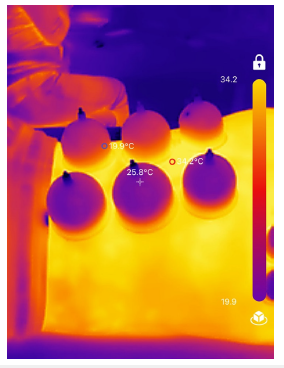
Players received cupping therapy if their current symptoms warranted treatment. The 134 treatments included in the study were all performed in response to a complaint of muscular pain that had been present for longer than 48 hours. The skin at the treatment site was prepared using coconut oil to allow the cups to have greater adherence. Cups were then applied to the treatment site, with two pumps of air being removed using the handheld pump included with the cupping set (Figure 1). Cups were left in place for 20 minutes before being removed. Any remaining coconut oil was then wiped off with a terry cloth towel. Prior to the treatment being applied, the skin surface temperature was measured at the center of the patient’s painful muscle area. The measurement site was determined by measuring the widest point of the treatment area in centimeters. Temperature measurements of the central most cup was taken at the time of application, at five-minute intervals until removal, and following removal of the cups. No pitchers reported adverse reactions to the treatment protocol (Figure 2).
Figure 1:

Figure 2:
Statistical analysis
Relevant data was collected from electronic medical records then was transferred to, and analyzed using, a commercially available statistics software package (SPSS Version 28, IBM, Armonk, NY). A total of 134 treatments from 26 medical records were included in the data analysis. Means and standard deviations were calculated where appropriate. A paired samples t-test was performed to assess skin surface temperature differences before and after cupping therapy. A one-way ANOVA test was performed to assess changes in temperature of the central most cup over time. Significance was set a p<0.05 a priori.
Result
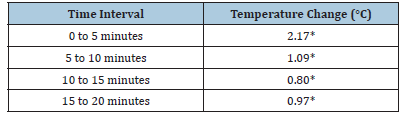
A total of 134 cupping therapy treatments were analyzed for the purposes of this study. Treatment sites are detailed in Table 1. On average, players receiving cupping therapy experienced significant increases in skin surface temperature (Pre-Cupping=31.47±1.03 °C, Post-Cupping=33.57±0.73 °C, t(266)=-19.233, p<.001). Results of the temperature increases of the central most cup are shown in Table 2.
Table 1: Treatment sites.
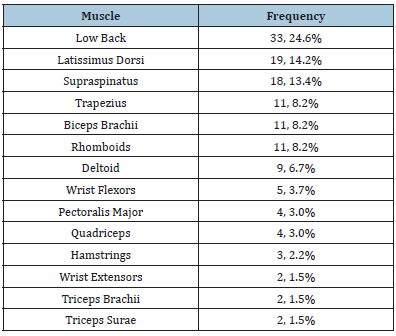
Table 2:Temperature changes of central most cup over
time.
*Significant at p<.001
Discussion
The purpose of this retrospective study was to assess the effectiveness of cupping therapy for increasing skin surface temperature. Previous research has shown that cupping therapy has been effective for improving blood flow and increasing skin surface temperature [12-14]. Previous research has identified the effectiveness of cupping therapy for decreasing muscular tenderness [13,14]. However, these studies have suffered from limitations in sample size. The goal of this study was to use a retrospective technique for the purpose of capturing more encounters for data analysis. To the authors’ knowledge, the current study captures the largest number of data points related to using cupping therapy to improve blood flow or increase skin surface temperature. A possible limitation of this study was that data was collected from multiple muscles. It is possible that muscle size, vascularity of the treatment site, and amount of subcutaneous tissue may influence the potential increase in skin surface temperature. Future research should use point of care ultrasound to quantify the depth of subcutaneous tissue at the treatment site. This would allow researchers to assess a possible correlation between depth of subcutaneous tissue and skin surface temperature increases resulting from cupping therapy. Another possible limitation of this study was that it did not assess the relationship of increases in skin surface temperature and therapeutic effects. Future research should assess the relationship between increases in skin surface temperature and benefits of cupping therapy such as decreased muscular tenderness.
This information may also help determine the amount of tissue temperature increase needed to achieve a therapeutic effect. This study also did not establish a direct correlation between skin surface temperature and localized blood flow. However, previous research he has shown that skin surface temperature appears to have a linear relationship with localized blood flow [15-17]. Further research should be conducted in a prospective manner to gain additional information to build on the current study. A randomized controlled trial that assessed depth of subcutaneous tissue and muscular tenderness in addition to skin surface temperature would account for the previously mentioned limitations. This information would be valuable for assisting in informing future studies and making progress toward establishing standardized guidelines for prescribing and administering cupping therapy.
Conclusion
In conclusion, cupping therapy appears to produce an increase in skin surface temperature, which likely indicates an increase in localized blood flow. To the authors’ knowledge, the number of treatments assessed in this study was more than any study evaluating the effect of cupping therapy on skin surface temperature in the current literature. Future research should examine the relationship between skin surface temperature and therapeutic effects of cupping therapy. If this research conforms to high standards and uses standardized methodology, a more definitive statement may be able to be made about how best to prescribe and apply cupping therapy for patients with musculoskeletal pain.
References
- Wood S, Fryer G, Tan LLF, Cleary C (2020) Dry cupping for musculoskeletal pain and range of motion: A systematic review and meta-analysis. Journal of Bodywork and Movement Therapies 24(4): 503-518.
- Malik S, Anand P, Bhati P, Hussain ME (2022) Effects of dry cupping therapy on pain, dynamic balance and functional performance in young female with recreational runners’ chronic plantar fasciitis. Sports Orthopedics and Traumatology 38(2): 159-170.
- Zhang H, Zhao M, Wu Z, Wang X, Jiang Y, et al. (2022) Effects of acupuncture, moxibustion, cupping, and massage on sports injuries: A narrative review. Evid Based Complement Alternat Med 2022: 9467002.
- Al Bedah AMN, Elsubai IS, Qureshi NA, Aboushanab TS, Ali GIM, et al. (2018) The medical perspective of cupping therapy: Effects and mechanisms of action. J Tradit Complement Med 9(2): 90-97.
- Furhad S, Sina RE, Bokhari AA (2024) Cupping Therapy. StatPearls Publishing, Florida, USA.
- Cage SA, Warner BJ, Gallegos DM, Sims-Koenig K (2020) Effects of cupping therapy on lower quarter Y-balance test scores in collegiate baseball players. Research & Investigations in Sports Medicine 6(1): 466-468.
- Chen K, Pittman RN, Popel AS (2008) Nitric oxide in the vasculature: Where does it come from and where does it go? A quantitative perspective. Antioxid Redox Signal 10(7): 1185-1198.
- Wang X, Zhang X, Elliott J, Liao F, Tao J (2020) Effect of pressures and durations of cupping therapy on skin blood flow responses. Front Bioeng Biotechnol 8: 608509.
- Lowe DT (2017) Cupping therapy: An analysis of the effects of suction on skin and the possible influence on human health. Complementary Therapies in Clinical Practice 29: 162-168.
- Mehta P, Dhapte V (2015) Cupping therapy: A prudent remedy for a plethora of medical ailments. J Tradit Complement Med 5(3): 127-134.
- Bridgett R, Klose P, Duffield R, Mydock S, Lauche R (2018) Effects of cupping therapy in amateur and professional athletes: Systematic review of randomized controlled trials. J Altern Complement Med 24(3): 208-219.
- Cage S, Warner B, Gallegos, DM (2020) Effect of cupping therapy on skin surface temperature in healthy individuals. Journal of Sports Medicine and Allied Health Sciences: Official Journal of the Ohio Athletic Trainers Association 5(3): 1-6.
- Li T, Li Y, Lin Y, Li K (2017) Significant and sustaining elevation of blood oxygen induced by Chinese cupping therapy as assessed by near-infrared spectroscopy. Biomedical Optics Express 8(1): 223-229.
- Arce AA, Warner BJ, Gallegos DM, Cage SA (2017) Effect of dry cupping on vascular function among young individuals. International Journal of Health Sciences 5(3).
- Alekseev SI, Ziskin MC (2009) Influence of blood flow and millimeter wave exposure on skin temperature in different thermal models. Bioelectromagnetics 30(1): 52-58.
- Jorge J, Hartford M, Villarroel M, Chaichulee S, Davidson S, et al. (2021) Non-contact assessment of peripheral artery hemodynamics using infrared video thermography. IEEE Transactions on Biomedical Engingeering 68(1): 276-288.
- Bateman DD, Mohammad A, Escandon JM, Matsui C, Saha S, et al. (2021) The effects of variations in the skin surface temperature on capillary blood flow using video-capillaroscopy. Plastic and Reconstructive Surgery Global Open 9(10S): 73-74.
© 2024 Cage SA. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






