- Submissions

Full Text
Research & Investigations in Sports Medicine
Delayed Diagnosis of Exercise Induced Compartment Syndrome After Treatment of Functional Popliteal Entrapment
Zachary Sukin1* and Charlie Yoo2
1Idaho College of Osteopathic Medicine, Idaho, USA
1UPMC Central PA, Pennsylvania, USA
*Corresponding author:Zach Sukin, Idaho College of Osteopathic Medicine, Idaho, USA
Submission: March 11, 2024;Published: April 01, 2024

ISSN: 2577-1914 Volume10 Issue2
Abstract
Popliteal Entrapment Syndrome (PAES) is a relatively uncommon diagnosis, that is commonly misdiagnosed. Treatment is also challenging, with patients often requiring subsequent surgeries. This is a case report of a 24-year-old male presents for surgery for his bilateral popliteal entrapment syndrome with concurrent exercise-induced compartment syndrome. He had symptoms for almost two years, saw multiple providers before being diagnosed with PAES. Once the patient was finally diagnosed with PAES and underwent surgery, the patient continued to have symptoms, that was misdiagnosed multiple times, before being diagnosed with exercise-induced compartment syndrome. The patient then underwent a bilateral fasciotomy and has had complete relief of all symptoms ever since.
Introduction
Popliteal Artery Entrapment Syndrome (PAES) is when the popliteal artery, popliteal vein and/or tibial nerve becomes compressed by surrounding myofascial structures in the popliteal fossa, primarily by the gastrocnemius’s medial head and the soleus’ fascial bands resulting in reduced blood flow during activity [1]. Symptoms include painful claudication, paresthesia, and foot drop. PAES can present in two different forms: functional or anatomical. Functional PAES is caused by a hypertrophied gastrocnemius which compresses the artery during exercise. Functional PAES is more commonly seen in younger more active patient populations and can present with bilateral symptoms. Anatomical PAES is more commonly seen unilaterally in older patients and is caused by a congenital abnormality in the attachments of the posterior calf musculature and or the popliteal vessels course. Distinguishing between functional and anatomical PAES is important as the pathology is different and will affect treatment pathways. Patients with anatomical entrapment experience progression to popliteal artery occlusion from the chronic deformity and eventually leading to severe ischemia of the lower extremity. Patients with functional PAES, typically have more reproducible claudication with intense exercise but due to their normal anatomic course of the artery [2], but if left untreated, it can lead to potential vascular damage, and lead to a limb threatening injury [3].
Chronic Exertional Compartment Syndrome (CECS) is nonspecific leg pain that occurs with the onset of activity and classically is difficult for providers to diagnose. CECS is caused by elevated pressures within a closed myofascial space during exercise, leading to decreased tissue perfusion and ischemia, with some patients reporting neurological impairments such as foot drop. Symptoms usually subside over several minutes following the cessation of activity [4]. Pain is classically described as feelings of hardness and is typically isolated to one or more fascial compartments in the leg, with the least common being the superficial posterior compartment, this contrasts with CECS where majority of the pain is reported in the superficial posterior compartment [5,6]. Due to the similar symptom presentation between PAES and CECS, patients are classically misdiagnosed for one or the other, leading to unsatisfactory results following treatment [1]. Consistent physical exam findings are lacking, and there is controversy around appropriate imaging techniques and protocols, specifically patients with PAES, classically have a normal CT-angiogram in the neutral foot position, with compression occurring only with foot plantarflexion, which causes the medial gastrocnemius to compress the popliteal artery against the lateral femoral condyle [5]. Patients with Functional PAES, classically have a 22-month delay in the diagnosis of the condition, which is primarily attributed to the low frequency of occurrence, compared to those with CECS [7]. The diagnosis of PAES does not exclude the diagnosis of CECS, as there have been a few reported case studies of patients being diagnosed with both. A retrospective study found that 31% of patients that underwent surgical intervention for Functional PAES, had been previously worked up for CECS. We present a case of a 24-year-old male initially diagnosed and treated for PAES, however continued to have worsening symptoms, and later diagnosed and treated for CECS.
Case Report
The patient described in this report has provided written informed consent to publish details of his medical care. A 24-yearold male initially presented with severe pain in both legs that was induced about a quarter of a mile into running. The patient reports that the symptoms have rapidly progressed over the last eight months. The patient played football up to his sophomore year of high school and varsity lacrosse all four years. He denies having these symptoms prior to now. The patient is an advanced skier and denies having parathesis in his lower extremities while skiing. The patient initially presented with a BMI of 24.8 and demonstrated a lean build with little body fat. The patient’s calves were well-defined bilaterally but did not demonstrate significant hypertrophy. The patient had well-defined and toned muscles, particularly in the legs and core. The patient has a past medical history of being treated for popliteal artery entrapment syndrome, bilaterally, ten months ago, which was treated surgically. Prior to this surgery, the patient had reported progressively worsening symptoms over the last year, which initially started from an increase in running intensity. The patient initially only noticed numbness in his right first metatarsal on the dorsal side following running at an incline or hiking uphill. The pain and numbness initially improved in his right foot after he rested for about 15 minutes. Over the course of several months, the patient had worsening symptoms to where the numbness progressed to the entire dorsum of his right foot and he eventually started to notice identical symptoms on his left foot. Eventually, the patient noticed complete numbness from the knee down bilaterally, affecting the anterior and posterior aspect of the lower leg and the dorsal and plantar aspect of both feet. Following this escalation in patient symptoms, the patient was referred to vascular surgery, where, on physical exam, he was found to have reduced palpable posterior tibialis pulses and dorsalis pedis pulses bilaterally which worsened with plantarflexion, with the right being worse than the left.
Figure 1:(a) CT-angiogram of right lower extremity, with foot in neutral position, (b) Foot in plantarflexion.
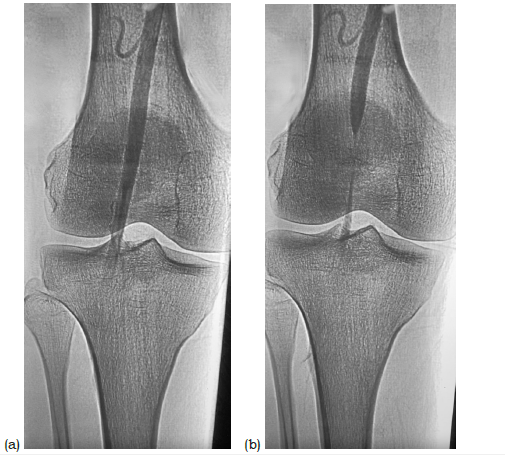
Neither popliteal fossa demonstrated signs of swelling or deformity. The patient was also noted to have a capillary refill of 7 in both lower extremities, and a normal Ankle-Brachial Index (ABI) of the lower extremities. Following this, the patient underwent a CT angiogram, where he was noted to have no compression of the popliteal artery when the foot was in the neutral position (Figure 1a). The patient was noted to have compression of the popliteal artery with plantarflexion manipulation of the foot (Figure 1b), with no evidence of a popliteal aneurysm. These findings confirmed the diagnosis of PAES, and no further tests were performed. The patient underwent partial resection of the medial gastrocnemius and the soleus muscle tendinous arch to release the popliteal artery. It was noted intraoperatively that damage to the popliteal artery in the right extremity started to show vascular damage from the muscle compression (Figure 2). Following the surgery, the patient was on ten weeks of activity restrictions and a physical therapy protocol. Once the patient was cleared for regular activity, the patient reported complete relief of symptoms running for three months. The patient now presents with severe calf pain bilaterally but denies any paresthesia in either extremity like before his PAES surgery. The patient noted severe pain in his anterior and posterior leg, which was brought on about a quarter mile into running and then persisted for up to 30 minutes following cessation of exercise. The patient reports that the pain has progressively worsened over the last several weeks as his activity level has picked up. The patient also says they now have severe pain in both legs, even upon walking. Upon physical exam, the patient had a lean athletic build, with a BMI of 23.6. The patient was noted to have a standard capillary refill and regular pulses in the distal lower extremity bilaterally. A repeat ABI was normal. At this time, the patient continued to note an increase in pain in both legs, leading to the patient having a repeat CT-angiogram of the right lower extremity, where the patient was found to have no compression of the popliteal artery with the foot in neutral and or with plantarflexion (Figure 3).
Figure 2:Intraoperative photo of right popliteal fossa, demonstrating endothelial damage to popliteal artery.
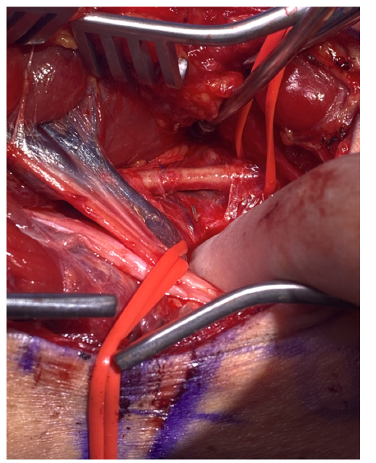
Figure 3:Repeat CT-angiogram of right lower extremity.
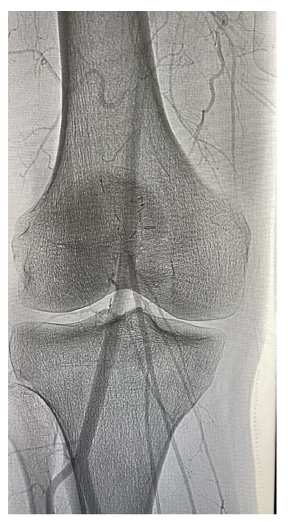
Table 1:Pre-post exercise compartment measures in the right lower extremity.

At this point, the patient was then referred to sports medicine, where he was noted to have tightness of compartments in the lower extremities bilaterally. The compartment pressure test was then ordered for the right lower extremity (Table 1), which shows slightly above normal resting compartment pressures and severely elevated compartment pressures following 1 minute of running at no incline on the treadmill. The patient’s symptoms and elevated compartment pressures following exercise were consistent with a diagnosis of CECS. The patient was then referred to orthopedic surgery to have the release of all four compartments in both lower extremities. Three incisions were made on each leg to perform a fasciotomy of all compartments. Following this, the patient was on crutches for three weeks and underwent six weeks of physical therapy that focused on restoring motion, strength, and function of his lower extremities. At ten weeks, he was able to resume regular activity. At six months post-fasciotomy, the patient reports complete relief of symptoms, specifically no pain in either leg upon running [8,9]. The patient is now 1.5 years out from this surgery, continues to note complete relief of symptoms, and is back to his prior standard activity regimen.
Discussion
Differentiating between anatomical and functional popliteal entrapment syndrome is important as they typically have differing clinical courses and are present in different patient populations. Functional popliteal entrapment syndrome is typically seen in younger competitive athletes, often describing vigorous exercise training prior to the onset of symptoms. Most of these patients have undergone extensive orthopedic evaluation consisting of compartment pressure testing, which is often positive in patients with functional entrapment, leading to a diagnosis of CECS alone and the patient undergoing a fasciotomy without relief of symptoms [10]. Differentiating between Popliteal Artery Entrapment Syndrome (PAES) and Chronic Exertional Compartment Syndrome (CECS) based on history alone can be tricky since both can present with deep calf pain, specifically in the superficial posterior compartment, that classically occurs during exercise alone. Symptoms include pain and cramping throughout the leg during exercise that improves following cessation of exercise. A physical exam can be helpful in the diagnosis of PAES. First, the examiner should palpate the Dorsalis Pedis (DP) pulse with the foot in the neutral position. Regardless of what the examiner finds with the DP pulse with the foot in the neutral position, the examiner should then have the patient perform both the plantar and dorsal flexion of the foot, with the DP pulse either disappearing or becoming weaker in either position, but rarely in both [11]. When the patient is plantar and dorsal flexing the foot, the gastrocnemius muscle, whose head is inserted at the level of the popliteal fossa, contracts, causing the muscle to stiffen and compress the popliteal fossa, which can lead to sudden changes in the DP and PT pulses. Various imagining modalities are currently used to work up PAES, such as Doppler ultrasound, ABI, or MRI, depending on the institution. The surgical treatment for PAES is a partial division of the medial head of the gastrocnemius, along with partial removal of the small fibers of the soleus. A recent study found that only 77% of patients with functional PAES have found a complete resolution of symptoms following surgery. In Turnipseed et al. [12], they evaluated 240 patients with atypical lower extremity claudication and found that thirty percent of patients with CECS, also had positive entrapment screening studies. In another cohort they evaluated patients with PAES, and reported an 86% incidence of concomitant CECS [9].
For CECS, the intramuscular pressure criteria described by Pedowtiz et al. [10] for diagnosis of CECS of the lower extremity is commonly used (1) pre-exercise pressure >15mm Hg, (2) a1- minute postexercise pressure of >30mm Hg. The surgical treatment for patients diagnosed with CECS includes a fasciotomy of all four compartments of the lower extremity. Patients with CECS are classically worked up for PAES alone prior to a diagnosis, leading to a long delay in treatment. Due to the similarity in symptom presentation between PAES and CECS, and without specific physical exam findings, we recommend the diagnostic protocol for either diagnosis, including vascular imaging such as Doppler ultrasound or MRA, along with measurement in compartment pressures. Doing this would prevent patients from undergoing one surgery rather than multiple, as did the patients in this study. Over 75% of athletes with functional PAES were able to return to prior activity levels following a fasciotomy and partial removal of the medial head of the gastrocnemius muscle [12]. Several of these patients were unable to return to their prior activity levels after their initial fasciotomy for CECS, suggesting that the concurrent diagnosis of PAES was either missed or developed following the fasciotomy. Considering the well-documented nature of functional PAES being misdiagnosed or mistreated for CECS, a workup to rule out the presence of FPAES with screening ABIs and a CTA with provocative maneuvers should be considered in all patients with CECS prior to surgery. This would allow for them to be treated surgically at the same time if both are present. The posterior compartment is already exposed for the partial removal of the medial head of the gastrocnemius; additionally, releasing the superficial and deep posterior compartments during the same procedure provides this convivence and prevents secondary surgeries afterward. Additionally, the morbidity of four-compartment fasciotomies remains relatively low, with major complications occurring 8.3% of the time, further backing the benefit of performing in patients with functional popliteal entrapment syndrome regardless of which compartments the symptoms are localized to [13].
Conclusion
This case report underscores the diagnostic challenges and therapeutic complexities encountered in managing Popliteal Entrapment Syndrome (PAES) and Exercise-Induced Compartment Syndrome (CECS). The presented case of a 24-year-old male highlights the recurrent nature of nonspecific symptoms and the potential for misdiagnosis, leading to delayed and ineffective treatments. The distinction between anatomical and functional PAES is crucial due to their differing clinical courses and treatment approaches. Additionally, the overlapping symptomatology between PAES and CECS demonstrates the necessity for a comprehensive diagnostic workup, including imaging studies and compartment pressure measurements. The successful management of this patient through bilateral fasciotomy not only relieved symptoms but also restored functionality, emphasizing the importance of accurate diagnosis and timely intervention. Heightened awareness among clinicians regarding the diagnostic nuances of PAES and CECS is imperative to prevent mismanagement and optimize patient outcomes. Additionally, considering the possibility of concurrent diagnoses in patients presenting with CECS symptoms, a thorough evaluation for PAES should be incorporated into the diagnostic algorithm to ensure comprehensive and effective treatment strategies.
Conflict of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. The patient described in this report has provided written informed consent to publish details of his medical care.
References
- Gaunder C, McKinney B, Rivera J (2017) Popliteal artery entrapment or chronic exertional compartment syndrome? Case Rep Med 2017: 6981047.
- Mustapha JA, Sarkar R, Rastogi U (2022) Awareness and early diagnosis of popliteal artery entrapment syndrome is needed. JACC Case Rep 4(7): 429-432.
- Lovelock T, Claydon M, Dean A (2021) Functional popliteal artery entrapment syndrome: An approach to diagnosis and management. International Journal of Sports Medicine 42(13): 1159-1166.
- David R, Roberts AJ, Hulse D (2015) Intramuscular compartment pressure measurement in chronic exertional compartment syndrome: New and improved diagnostic criteria. The American Journal of Sports Medicine43(2): 392-398.
- George CA, Hutchinson MR (2012) Chronic exertional compartment syndrome. Clinics in Sports Medicine 31(2): 307-319.
- Hislop M, Tierney P, Murray P, Brien MO, Mahony N (2003) Chronic exertional compartment syndrome: The controversial “fifth” compartment of the leg. The American Journal of Sports Medicine 31(5): 770-776.
- Lawley RJ, Kasitinon D, Sisk Daniel, Lavingia KS, Lee JT, et al. (2022) Concurrent diagnosis of functional popliteal artery entrapment syndrome and chronic exertional compartment syndrome in athletes. Current Sports Medicine Reports 21(10): 366-370.
- Dyer K, Hogrefe C (2018) Don’t just blame it on the veins: An update on vascular exertional limb pain. Curr Sports Med Rep 17(10): 347-353.
- Frontera W (2002) Essentials of physical medicine and rehabilitation. (4th edn), Hanley and Belfus, Philadelphia, USA, pp. 256-261.
- Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH (1990) Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. Am J Sports Med 18(1): 35-40.
- Sinha S, Houghton J, Holt PJ, Thompson MM, Loftus IM, et al. (2012) Popliteal entrapment syndrome. J Vasc Surg 55(1): 252-262.
- Turnipseed WD (2002) Popliteal entrapment syndrome. J Vasc Surg 35(5): 910-915.
- Gatenby G, Haysom S, Twaddle B, Walsh S (2017) Functional outcomes after the surgical management of isolated anterolateral leg chronic exertional compartment syndrome. Orthopedic Journal of Sports Medicine5(11): 2325967117737020.
© 2024 Zachary Sukin. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






