- Submissions

Full Text
Research & Investigations in Sports Medicine
Effects of Virtual Reality and Active Gaming Integration on Performance and Lower Extremity and Trunk Function in Cerebral Palsy Patients: A Systematic Review
Aiden E Cook1, Joseph I Esformes1, Rhiannon A Owens2 and Jeremy A Moody1,3*
1School of Sport and Health Sciences, Cardiff Metropolitan University, UK
2SDR Rehabilitation Ltd, UK
3School of Physical Education and Sports, Nisantasi University, Turkey
*Corresponding author:Jeremy A Moody, School of Sport and Health Sciences, Cardiff Metropolitan University, UK
Submission: December 21, 2023;Published: January 08, 2024

ISSN: 2577-1914 Volume10 Issue1
Abstract
Keywords:SActive gaming; Cerebral palsy; Conventional therapy; Intervention; Virtual reality
Abbreviations: 1MWT: 1-Minute Walk Test; 10MWT: 10-Meter Walk Test; 2MWT: 2-Minute Walk; 6MWT: 6-Minute Walk Test; AG: Active gaming; aBMD: Areal Bone Mineral Density; CP: Cerebral Palsy, d: Days; FMS: Functional Mobility Scale, GMFM-66: Gross Motor Function Measure-66; iso: Isokinetic; min: Minutes; MiTii: Move to Improve It; RCT: Randomised Control Trials; STST: Sit to Stand Test; TGGT: Timed Get Up and Go Test; TUDST: Timed Up and Down Stairs Test; TYMO: Tyromotion GmbH; VR: Virtual reality, wks: Weeks
Introduction
The neurological condition of Cerebral Palsy (CP) occurs due to trauma to one or more areas of the developing brain in children before the completion of cerebral development [1,2]. Most commonly, the causes of 80% of recorded cases occur during the prenatal period of development because of unknown causes. However, complications during pregnancy or labour, such as asphyxia, have been linked to causes of CP in many documented cases [1]. Instances of CP may also occur during the post-natal and neo-natal periods [3], with common risk factors, which may include the birth of a child weighing <2.5kg, premature birth, brain hemorrhage, child abuse and bacterial meningitis [1]. These instances can cause both musculoskeletal and neuromuscular impairments. Such conditions will affect the daily living of children and in later life, adults with CP [2]. Motor impairments commonly affect individuals with CP and can be observed through muscle weakness, hypertonicity, tremors, scissor gait and increased tendon reflexes [4]. Conversely, the neurological condition can also exist with less apparent symptoms such as sensation, perception and cognitive and behavioural performance disturbances [2,5]. Several techniques have been adopted to lessen the severity and tackle CP [6-8]. However, these treatments cannot completely eradicate CP, so treatments throughout the individual’s lifespan must be ongoing. With a shortage of access to therapy in the United Kingdom, especially with increased age [9], time-consuming appointments and increasing equipment expenses, more alternative approaches that are affordable, enjoyable and flexible treatments must be considered to conventional therapies [10].
Rehabilitation methods that integrate technology are a developing area, with Virtual Reality (VR) and Active Gaming (AG) incorporated into clinical therapy and the everyday life of CP patients [11]. VR and AG have recently increased in popularity when completing at-home, in-school and in-clinic rehabilitation interventions [12]. Using computer VR hardware and software allows interactive user stimulation for engaging with the environment, like real-world experiences and objects [13]. These systems can be used to develop and achieve rehabilitation goals by immersing individuals in three-dimensional games while manipulating game types, complexity and intensity for the desired physical, performance and rehabilitation outcomes [14,15]. Two adaptations of VR are currently used within CP rehabilitation. The first is commercial video game devices and platforms, including, but not limited to, systems like Nintendo Wii, Sony PlayStation and Microsoft Xbox consoles [12]. The second involves custom VR systems specifically developed for rehabilitation purposes, systems such as Move to Improve It (MiTII; Mitii Development A/S, Copenhagen, Denmark) [16], E-Link Evaluation and Exercise System (Biometrics Ltd) [17] and Eloton SimCycle Virtual Cycling System (Eloton, Inc., NV, USA) [18]. Both commercial and custom systems offer users a more enjoyable and specific experience and increase motivation and buyin for rehabilitation [19].
Although some studies using varying methods and equipment to elicit a response, compared to other therapies or no other intervention, show no effect [20-25], both commercial video game devices and VR systems have been shown to elicit positive effects in numerous research studies, with improvements in daily living ability [10,20], gait [26-28], mobility [29,30] and limb bone mineral density [26]. These interventions elicit improvements in gross motor function and skill transfer to daily living tasks [28]. However, for the brain to make these motor changes permanent, motor learning needs to be exploited [29,30]. Contributions to motor-learning development are most evident when adopting task repetition, task difficulty and motivation [31,32]. Although the current review is comprised of studies lacking high-quality methodologies, reducing the credibility of some of the findings [33], these studies suggest that motor learning can be potentiated with VR, with these motor skills transferring to motor abilities and real-life integration [34-36]. Therefore, the current study aims to review the existing literature on the effects of VR and active gaming integration for improving performance and lower extremity and trunk function in cerebral palsy patients.
Methods
Methods
The systematic review followed the guidelines for systematic reviews by Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [37], following the Medical Research Methodology for healthcare systematic reviews [38]. A PICO framework (participants, interventions, comparators, and outcomes) was used to provide a clear scope of the research required for the review [38]. PICO framework: P=children with spastic cerebral palsy; I=Virtual gaming; C=a comparison therapy or no therapy; O=Lower extremity function (e.g. GMFM, strength, gait, ambulation). The principal researcher conducted an independent review of the results of the papers included, and the results gathered. A second researcher verified a portion of the search and analysis with 100% accuracy.
Identification and selection of studies
Electronic searches were conducted on the following databases in May 2021: ‘PUBMED’, ‘Google Scholar’ and ‘MetSearch’. The search strategy included terms with the effect of ‘cerebral palsy’, ‘virtual reality’, ‘video games’, ‘virtual gaming’, ‘lower extremity’, and ‘ambulation’. A truncation technique was used to help broaden searches; the method allows for various word endings to be applied by using an asterisk (*) in search bars (e.g. game* allows results for games and gaming). All publications were stored in the citation management centre, and duplicates were removed. Titles were screened, and articles of interest were further inspected for abstracts with keywords related to the literature search. Full copies of relevant studies were found, and their reference list was screened for further studies relating to the research topic.
Eligibility criteria
The inclusion criteria for the systematic review were: (a) randomised control trials or randomised cross-over trials that examined the effects of virtual reality, (b) the papers were required to be peer-reviewed and in the English language, dated between 2011-2021, (c) the target population was between birth and 18 years old, with any type and severity of CP, (d) the study compared VR with conventional therapy or no therapy, (e) the study examined outcome measures surrounding the lower extremity and trunk function, and performance. The research papers provided data describing the magnitude of the intervention effect and data allowing for effect size calculations (e.g., standard deviation). Studies were excluded if immediate responses were measured and the intervention was not implemented over a minimum of three weeks.
Data extraction
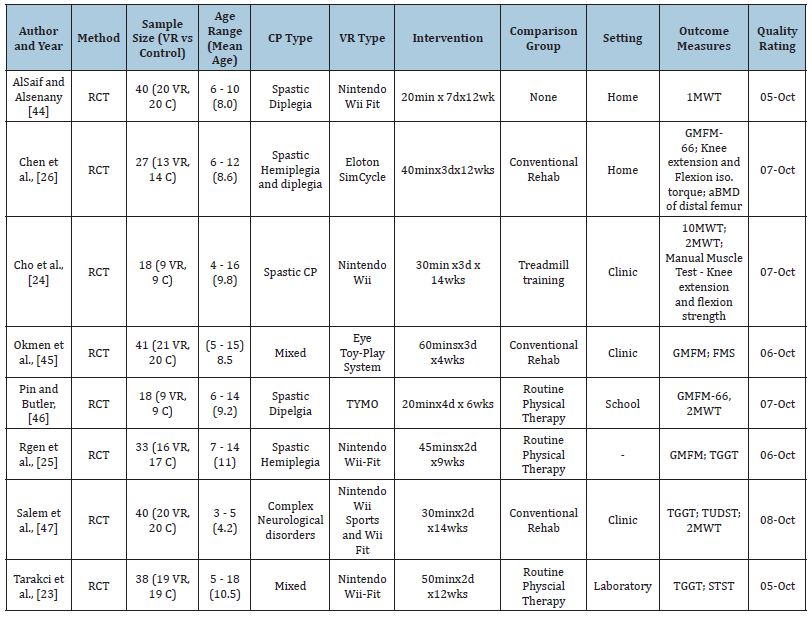
The articles that met the criteria were extracted for a full review of the strength and quality of the study design, study characteristics and outcome measures. The information extracted from the research included methodological design, sample size, participant description (age, sex, type of CP and CP severity), intervention protocol (duration, intensity, etc.), gaming method and the results of the outcome. Other miscellaneous variables, such as year of publication and name of authors, were included. All variables are displayed in Table 1. The included studies often measured multiple outcome measures. Only measures relating to the lower extremities are included (excluding postural or balance-related measures). The quality of the study design was evaluated through the criteria described by the Physiotherapy Evidence Database (PEDro scale). The scale has 11 items, with one referring to the external validity (inclusion criteria and source), which is not included in the final score.
The remaining 10 items assess internal validity through:
a. Random allocation
b. Concealment of allocation
c. Baseline comparability
d. Blinding of subjects
e. Blinding of therapists
f. Blinding of assessors
g. Adequacy of follow up (>85%)
h. Intention-to-treat analysis
i. Between-group analysis
j. Point estimates and variability [39].
Table 1:Characteristics of the Cerebral Palsy (CP) and Virtual Reality (VR) studies that met inclusion criteria. RCT=Randomised Control Trials; min=minutes; d=days; wks=weeks; MiTii =Move to improve it; TYMO = Tyromotion GmbH (Graz, Australia); 1MWT =1-Minute Walk Test; GMFM-66=Gross Motor Function Measure-66; iso = isokinetic; aBMD=areal bone mineral density; 10MWT=10-Meter Walk Test; 2MWT= 2-Minute Walk Test; 6MWT=6-Minute Walk Test; FMS=Functional Mobility Scale; TGGT=Timed Get Up and Go Test; TUDST=Timed Up and Down Stairs Test ; STST=Sit to stand test.
A score of 9 to 10 represents an excellent methodological approach, 6 to 8 represents good, 4 to 5 represents fair and less than 4 represents poor [40]. The scale is widely used in systematic reviews, showing good reliability (Intraclass Correlation Coefficient [ICC] = 0.59-0.91) [40,41] with individual items ranging from fair to excellent (kappa = 0.50-0.88) [40,42]. However, the PEDro scale is not a gold-standard measure, with the study’s validity being imperfect due to nonmethodological factors influencing the results [39].
Data analysis
After studies were screened, the required data was pooled into a Microsoft Excel workbook (Microsoft Excel, Microsoft Corporation, Redmond, WA). All variables were standardized into the same unit of measurement to allow for simple comparison. The mean and standard deviation of the difference between groups were inputted, allowing the mean percentage difference to be calculated for all results. Cohen’s d effect size (d) calculation was determined for all results. Effect size allows for a greater description of the magnitude of differences between groups, with .2, .5 and .8 considered small, medium and large effect sizes, respectively [43].
Result
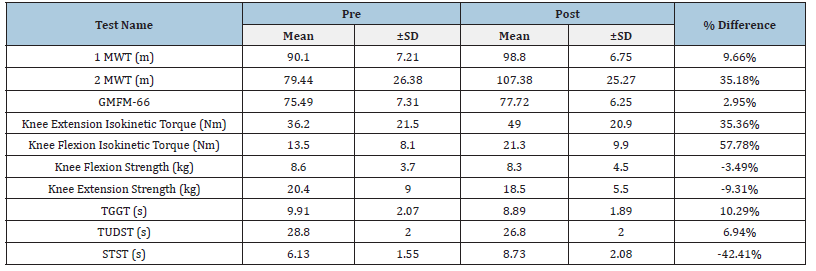
When comparing the results in both Tables 2 & 3 for movement competency, the intervention groups showed greater improvements in the 1-Minute Walk Test (1 MWT), 2-Minute Walk Test (2 MWT), Timed Get Up and Go Test (TGGT) and Timed Up and Down Stairs Test (TUDST) (9.66%, 35.18%, 10.29%, and 9.64%, respectively) when compared to the control groups (0.77%, 16.90%, 5.44%, and 3.36%, respectively). However, the control group showed greater improvements in GMFM-66 (3.92%). All groups elicited reductions in the Sit to Stand Test (STST), but the intervention group showed a higher percentage decrease than the control group (-42.41% vs -8.65%, respectively). Isokinetic measures of knee torque for the control group during extension and flexion were 3.87% and -14.74%, respectively, lower than the improvements in the intervention group, with an increase of 35.36% for extension and 57.78% when completing knee flexion. Knee flexion and extension strength results for the intervention groups displayed reductions in scores of -3.49% (flexion) and -9.31% (extension). In contrast, the control group improved by 20.29% when flexing at the knee and 20.71% during extension [44,45].
Table 2:Mean and ±SD test battery results for the control groups from all reviewed studies. 1 MWT=1-Minute Walk Test; 2MWT=2-Minute Walk Test; GMFM-66 =Gross Motor Function Measure-66; TGGT=Timed Get Up and Go Test; TUDST=Timed Up and Down Stairs Test; STST=Sit to Stand Test; Nm=Newton meter; kg=kilogram; s=seconds.
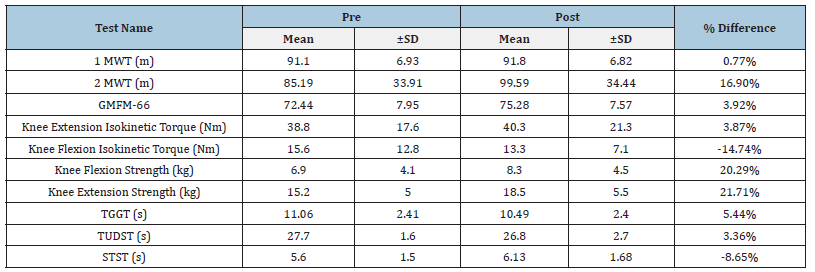
Table 3:Mean and ±SD test battery results for the intervention groups from all reviewed studies. 1 MWT=1-Minute Walk Test; 2 MWT=2-Minute Walk Test; GMFM-66=Gross Motor Function Measure-66; TGGT=Ti.
Discussion
This systematic review examined studies that used the integration of VR and AG as an intervention technique for CP patients. Based on the studies reviewed, VR and AG can elicit improvements in several areas of CP rehabilitation, enhancing the movement quality and muscular strength of individuals with CP [46]. Although the studies showed that VR and AG interventions can elicit positive responses in populations with CP, Salem et al. [47] and Cho et al. [24] reported a decrease in knee movement strength (both flexion and extension) and STST in the intervention groups. STST decreased in both groups from pre- to post-testing, but the magnitude of the reduction was lower in the control group by 33.76% [47]. In the control condition, knee flexion and extension post-testing increased, suggesting that VR and AG may not be efficacious for CP patients if the outcome is to increase knee flexion and extension strength and STST [24]. The potential rationale for these findings is both multifactorial and non-conclusive, based on the range presented for the duration of the studies and the exercise mode used as the primary use of support (treadmill versus conventional rehabilitation). Cho et al. [24] was the only study where the control group performed treadmill training. In contrast, the control group performed conventional physical therapy in the other studies. Treadmill training for individuals with cerebral palsy has been shown to increase lower limb strength and power [48- 50]. Although VR and AG benefit CP rehabilitation, other methods may elicit greater responses depending on the targeted outcome. VR and computer gaming are effective methods in CP rehabilitation due to their interactive nature and psychological impact, which may help with participant compliance and therapy mode adherence.
Computer games may have outcome goals that can intrinsically motivate the individual and increase self-motivation, leading to greater adherence [51]. Furthermore, if VR or computer game outcome goals are achievable, they can lead to an increased sense of mastery [52]. Both psychological benefits can help improve participation in the given activity, which may lead participants to achieve other physical performance parameters.
Conclusion
Although the findings for using VR and AG are encouraging and support their use in CP therapy, they may be best used in a multi-disciplinary approach by using more than one intervention or pairing their use with conventional CP rehabilitation. Future research should compare VR and computer gaming with other intervention methods and consider the outcomes of concurrently using VR and AG with different techniques. Pairing VR and AG with other CP therapies, such as whole-body vibration training [53], will further elucidate the scope of potential physical development using a multi-modal approach.
The authors thank Ms. Mia Washington for helping with the data collection.
- Krigger KW (2006) Cerebral palsy: An overview. Am Fam Physician 73(1): 91-100.
- Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, et al. (2007) A report: The definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl 109: 8-14.
- Krägeloh Mann I, Cans C (2009) Cerebral palsy update. Brain Dev 31(7): 537-544.
- Merck (2011) The Merck manual of diagnosis and therapy. (19th edn), London, UK, p. 3790.
- Ravi DK, Kumar N, Singhi P (2017) Effectiveness of virtual reality rehabilitation for children and adolescents with cerebral palsy: An updated evidence-based systematic review. Physiotherapy 103(3): 245-258.
- Boyd RN, Morris ME, Graham HK (2001) Management of upper limb dysfunction in children with cerebral palsy: A systematic review. Eur J Neurol 8(5): 150-66.
- Ritzmann R, Stark C, Krause A (2018) Vibration therapy in patients with cerebral palsy: A systematic review. Neuropsychiatr Dis Treat 14: 1607-1625.
- Novak I, Morgan C, Fahey M, Finch-Edmondson M, Galea C, et al. (2020) State of the evidence traffic lights 2019: Systematic review of interventions for preventing and treating children with cerebral palsy. Curr Neurol Neurosci Rep 20(2): 3.
- Coombe S, Moore F, Bower E (2012) A national survey of the amount of physiotherapy intervention given to children with cerebral palsy in the UK in the NHS. Association of Paediatric Chartered Physiotherapists 3(1): 5-18.
- Farr WJ, Green D, Bremner S, Male I, Gage H, et al. (2021) Feasibility of a randomised controlled trial to evaluate home-based virtual reality therapy in children with cerebral palsy. Disabil Rehabil 43(1): 85-97.
- Chen Y, Fanchiang HD, Howard A (2018) Effectiveness of virtual reality in children with cerebral palsy: A systematic review and meta-analysis of randomised controlled trials. Phys Ther 98(1): 63-77.
- Demers M, Fung K, Subramanian SK, Lemay M, Robert MT (2021) Integration of motor learning principles into virtual reality interventions for individuals with cerebral palsy: Systematic review. JMIR Serious Games 9(2): e23822.
- Weiss PL, Kizony R, Feintuch U, Katz N (2006) Virtual reality in neurorehabilitation. In: Selzer M, Clarke S, Cohen L, Duncan P, Gage F (Eds.), Textbook of Neural Repair and Rehabilitation. Cambridge University Press, Cambridge, UK, pp. 182-97.
- Burke JW, McNeill MDJ, Charles DK, Morrow PJ, Crosbie JH, et al. (2009) Optimizing engagement for stroke rehabilitation using serious games. Vis Comput 25(12): 1085-1099.
- Levac D, Rivard L, Missiuna C (2012) Defining the active ingredients of interactive computer play interventions for children with neuromotor impairments: A scoping review. Res Dev Disabil 33(1): 214-223.
- Mitchell LE, Ziviani J, Boyd RN (2016) A randomised controlled trial of web-based training to increase activity in children with cerebral palsy. Dev Med Child Neurol 58(7): 767-773.
- Rostami HR, Arastoo AA, Nejad SJ, Mahany MK, Malamiri RA, et al. (2012) Effects of modified constraint-induced movement therapy in virtual environment on upper-limb function in children with spastic hemiparetic cerebral palsy: A randomised controlled trial. Neuro Rehabilitation 31(4): 357-365.
- Chen CL, Hong WH, Cheng HYK, Liaw MY, Chung CY, et al. (2012) Muscle strength enhancement following home-based virtual cycling training in ambulatory children with cerebral palsy. Res Dev Disabil 33(4): 1087-1094.
- Bryanton C, Bossé J, Brien M, McLean J, McCormick A, et al. (2006) Feasibility, motivation, and selective motor control: Virtual reality compared to conventional home exercise in children with cerebral palsy. Cyberpsychol Behav 9(2): 123-128.
- James S, Ziviani J, Ware RS, Boyd RN (2015) Relationships between activities of daily living, upper limb function, and visual perception in children and adolescents with unilateral cerebral palsy. Dev Med Child Neurol 57(9): 852-857.
- Booth ATC, Buizer AI, Meyns P, Oude Lansink ILB, Steenbrink F, et al. (2018) The efficacy of functional gait training in children and young adults with cerebral palsy: A systematic review and meta-analysis. Dev Med Child Neurol 60(9): 866-883.
- Gagliardi C, Turconi AC, Biffi E, Maghini C, Marelli A, et al. (2018) Immersive virtual reality to improve walking abilities in cerebral palsy: A pilot study. Ann Biomed Eng 46(9): 1376-1384.
- Tarakci D, Ersoz Huseyinsinoglu B, Tarakci E, Razak Ozdincler A (2016) Effects of Nintendo Wii-Fit® video games on balance in children with mild cerebral palsy: Balance therapy in cerebral palsy. Pediatr Int 58(10): 1042-1050.
- Cho C, Hwang W, Hwang S, Chung Y (2016) Treadmill training with virtual reality improves gait, balance, and muscle strength in children with cerebral palsy. Tohoku J Exp Med 238(3): 213-218.
- Rgen M, Akbayrak T, Gunel M, Cankaya O, Guchan Z, et al. (2016) Investigation of the effects of the Nintendo Wii-Fit training on balance and advanced motor performance in children with spastic hemiplegic cerebral palsy: A randomized controlled trial. Int J Ther Rehabil Res 5(4): 146.
- Chen CL, Chen CY, Liaw MY, Chung CY, Wang CJ, et al. (2013) Efficacy of home-based virtual cycling training on bone mineral density in ambulatory children with cerebral palsy. Osteoporos Int 24(4): 1399-1406.
- Sajan JE, John JA, Grace P, Sabu SS, Tharion G (2017) Wii-based interactive video games as a supplement to conventional therapy for rehabilitation of children with cerebral palsy: A pilot, randomised controlled trial. Dev Neurorehabil 20(6): 361-367.
- Massetti T, Silva TD da, Ribeiro DC, Malheiros SRP, Ré AHN, et al. (2014) Motor learning through virtual reality in cerebral palsy: A literature review. Med Express 1(6): 302-306.
- Krakauer JW (2015) The applicability of motor learning to neurorehabilitation. Oxford Textbook of Neurorehabilitation. Oxford University Press, Oxford, UK, pp. 55-64.
- Winstein CJ, Kay DB (2015) Translating science into practice: Shaping rehabilitation practice to enhance recovery after brain damage. Prog Brain Res 218: 331-360.
- Kleim JA, Jones TA (2008) Principles of experience-dependent neural plasticity: Implications for rehabilitation after brain damage. J Speech Lang Hear Res 51(1): 225-239.
- Muratori LM, Lamberg EM, Quinn L, Duff SV (2013) Applying principles of motor learning and control to upper extremity rehabilitation. J Hand Ther 26(2): 94-102.
- Golomb MR, McDonald BC, Warden SJ, Yonkman J, Saykin AJ, et al. (2010) In-home virtual reality videogame telerehabilitation in adolescents with hemiplegic cerebral palsy. Arch Phys Med Rehabil 91(1): 1-8.
- Straker LM, Campbell AC, Jensen LM, Metcalf DR, Smith AJ, et al. (2011) Rationale, design and methods for a randomised and controlled trial of the impact of virtual reality games on motor competence, physical activity and mental health in children with developmental coordination disorder. BMC Public Health 11(1): 654.
- Grecco LAC, Duarte N de AC, de Mendonça ME, Pasini H, Lima VLC de C, et al. (2013) Effect of transcranial direct current stimulation combined with gait and mobility training on functionality in children with cerebral palsy: Study protocol for a double-blind randomised controlled clinical trial. BMC Pediatr 13(1): 168.
- Karlsson P, Bech A, Stone H, Vale C, Griffin S, et al. (2019) Eyes on communication: Trialing eye-gaze control technology in young children with dyskinetic cerebral palsy. Dev Neurorehabil 22(2): 134-140.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) Updating guidance for reporting systematic reviews: Development of the PRISMA 2020 statement. J Clin Epidemiol 134: 103-112.
- Smith V, Devane D, Begley CM, Clarke M (2011) Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol 11(1): 15.
- Macedo LG, Elkins MR, Maher CG, Moseley AM, Herbert RD, et al. (2010) There was evidence of convergent and construct validity of Physiotherapy Evidence Database quality scale for physiotherapy trials. J Clin Epidemiol 63(8): 920-925.
- Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M (2003) Reliability of the PEDro scale for rating quality of randomised controlled trials. Phys Ther 83(8): 713-721.
- Foley NC, Bhogal SK, Teasell RW, Bureau Y, Speechley MR (2006) Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomised controlled trials of pharmacological and nonpharmacological interventions. Phys Ther 86(6): 817-824.
- Brandt C, Sole G, Krause MW, Nel M (2007) An evidence-based review on the validity of the Kaltenborn rule as applied to the glenohumeral joint. Man Ther 12(1): 3-11.
- Cohen J (2013) Statistical power analysis for the behavioral sciences. (2nd edn), London, UK.
- AlSaif AA, Alsenany S (2015) Effects of interactive games on motor performance in children with spastic cerebral palsy. J Phys Ther Sci 27(6): 2001-2003.
- Metin Ökmen B, Doğan Aslan M, Nakipoğlu Yüzer GF, Özgirgin N (2019) Effect of virtual reality therapy on functional development in children with cerebral palsy: A single-blind, prospective, randomised-controlled study. Turk J Phys Med Rehabil 65(4): 371-378.
- Pin TW, Butler PB (2019) The effect of interactive computer plays on balance and functional abilities in children with moderate cerebral palsy: A pilot randomised study. Clin Rehabil 33(4): 704-710.
- Salem Y, Gropack SJ, Coffin D, Godwin EM (2012) Effectiveness of a low-cost virtual reality system for children with developmental delay: a preliminary randomised single-blind controlled trial. Physiotherapy 98(3): 189-195.
- Gorter H, Holty L, Rameckers EEA, Elvers HJWH, Oostendorp RAB (2009) Changes in endurance and walking ability through functional physical training in children with cerebral palsy. Pediatr Phys Ther 21(1): 31-37.
- Willoughby K, Dodd K, Shields N (2009) A systematic review of the effectiveness of treadmill training for children with cerebral palsy. Disabil Rehabil 31(24): 1971-1979.
- Molina Rueda F, Aguila Maturana AM, Molina Rueda MJ, Miangolarra Page JC (2010) Treadmill training with or without partial body weight support in children with cerebral palsy: Systematic review and meta-analysis. Rev Neurol 51(3): 135-145.
- Deci EL, Ryan RM (2008) Self-determination theory: A macro theory of human motivation, development and health. Can Psychol 49(3): 182-185.
- Edwin A Locke, Latham GP (2012) New developments in goal setting and task performance. (1st edn), Routledge England, UK, p. 688.
- Cook AE, Moody JA, Owens RA, Esformes JI (2020) A systematic review of the acute adaptations to vibration interventions for individuals with cerebral palsy. ARC Journal of Research in Sports Medicine 5 (1): 20-27.
© 2023 Jeremy A Moody*. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






