- Submissions

Full Text
Research & Investigations in Sports Medicine
Use of External Dynamic Arm Stabilizer with a Collegiate Baseball Player with a Glenohumeral Labrum Tear
Cage SA1*, Jacobsen AP2,3, Skowron P2,3, Wang A2,3, Trail LE1,3 and Hodges C3
1The University of Texas at Tyler, USA
2The University of Texas Health Science Center at Tyler, USA
3UT Health East Texas, USA
*Corresponding author:Cage SA, The University of Texas at Tyler, USA
Submission: July 27, 2023;Published: August 11, 2023

ISSN: 2577-1914 Volume9 Issue5
Abstract
Glenohumeral labrum tears are a relatively common injury experienced by overhead athletes, particularly baseball players. Labrum tears have the potential to lead to time lost from sport, along with loss of financial compensation. There is a need for reports that detail non-operative interventions for glenohumeral labrum tears that allow for a safe and expedient return to activity. In this report, we present the case of a collegiate baseball player with a glenohumeral labrum tear who underwent five weeks of treatment and rehabilitation for his injury. To return to play for post-season competitions, the patient made use of an external dynamic arm stabilizer to provide support and attenuate force when throwing and swinging. This appears to be the first case study detailing the use of an external dynamic arm stabilizer in conjunction with rehabilitation and treatment to align with a patient’s goal of a safe, expedited return to participation.
Introduction
It has been well documented that the glenohumeral joint and surrounding shoulder complex undergo a large amount of force when a baseball is being thrown [1,2]. When exposed to these forces, there is an increased risk of ligamentous and musculoskeletal structures of the shoulder, and microtrauma has been documented at the shoulder as well [1,2]. In baseball players, the glenohumeral labrum is a structure that causes particular concern when considering potential shoulder pathologies [3,4]. A study researching baseball players who had undergone labrum repair surgery found that on average, players took 315 days to return to full participation [5]. As individuals reach elite college and professional levels, this amount of time lost from injury may be associated with a risk of loss of future earnings and other financial compensations [6]. In this case report, we present the details of the use of an external dynamic arm stabilizer in a collegiate baseball player with an anterior glenohumeral labrum tear to expedite return to participation. To the authors’ knowledge, there has not been a published report describing the use of a dynamic arm stabilizer for enhancing a baseball player’s return to sports-related activities.
Case History
A 22-year-old collegiate male baseball player reported to the athletic training staff immediately after attempting to slide into a base. The patient stated that once his hand met the base, he felt his right shoulder shift anteriorly. After feeling the shift, the patient felt a sharp pain in the anterior aspect of his shoulder, along with diffuse weakness. When the patient attempted to throw a ball in the next half inning, he was unable to throw and the patient was removed from the competition.
Initial presentation
Evaluation in the team dugout revealed weakness with shoulder abduction, flexion and external rotation. Tenderness to palpation was noted along the proximal long head of the biceps tendon and the posterior aspect of the shoulder capsule. Anterior Apprehension, Jobe’s Relocation and Empty Can tests were all positive. The differential diagnosis at this time consisted of an anterior glenohumeral subluxation, glenohumeral labrum tear, and biceps tendon sprain. The team physician was contacted to set an appointment for further evaluation.
Evaluation and diagnosis
The day following the injury, the patient was evaluated by the team physician, whose exam yielded a differential diagnosis consistent with athletic trainers. During his exam, the physician noted the patient was lacking in active range of motion for shoulder internal rotation, external rotation and abduction. X-rays revealed no bony abnormalities and an MRI with contrast was ordered for further evaluation. Eight days after the initial injury, the patient’s MRI with contrast revealed a 180-degree anterior labrum tear. There was no evidence of injury to the rotator cuff, joint capsule, or other cartilaginous structures. Upon noting the extent of the labrum tear, the team physician referred the patient for further consultation with a sports medicine trained orthopedic surgeon. Eleven days after the initial injury, the surgeon noted that the patient’s strength and range of motion had begun to improve when compared with the previous two evaluations. It recommended that the patient attempt conservative treatment. At this time, the patient was educated on potential return-to-play issues with glenohumeral labrum repair in overhead athletes. The patient consented to attempting a conservative course of treatment at this time, with a plan to follow-up with the team physician every two weeks. An additional follow-up was planned with the surgeon at six weeks following the initial injury.
Treatment and return to play
Twelve days after the initial injury, the patient began a treatment and rehabilitation program intended to decrease pain, increase range of motion and strength at the shoulder. During the early phases of the treatment and rehabilitation program the patient was withheld from all baseball activities, along with weightlifting activities that involved upper extremity exercises or having to grip an implement. After further discussion between the athletic trainer, team physician, and the patient, he was also prescribed a course of meloxicam 15mg to address any lingering inflammation from the patient’s injury.
Week 2: Treatment during the first two weeks of conservative management was aimed at decreasing pain and increasing blood flow to the injured area. As such, the patient received cupping therapy three times a week. Prior to each cupping session, the treatment site was prepared with coconut oil, and the treatment duration was 20-minutes. The cupping therapy treatments were performed over the anterior and posterior deltoid, upper trapezius, bicipital groove, and posterior shoulder capsule using plastic pneumatic cups. Rehabilitation during this phase of treatment is detailed in Table 1.
Table 1: Weeks 2 of rehabilitation performed five days per week.
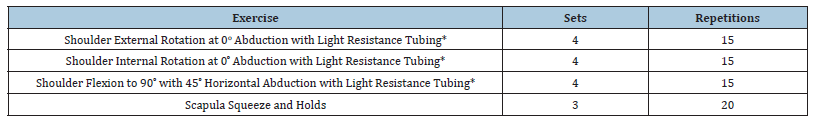
*Exercise performed in conjunction with blood flow restriction at 50% maximum brachial artery outflow.
Week 3: By the third week, the patient reported significant improvement in pain. Thus, cupping therapy was shifted to an as needed basis. A follow-up evaluation with the team physician and athletic trainer yielded improvements in strength and range of motion that indicated the ability to progress rehabilitation in terms of volume and frequency. With the decrease in pain, the patient began to participate in fielding exercises while still being withheld from throwing and hitting during practice. During weightlifting sessions, the patient was cleared to begin upper extremity exercises using resistance tubing provided the exercise did not place the patient’s shoulder in an abducted and externally rotated position. Rehabilitation during this phase of treatment is detailed in Table 2.
Table 2:Week 3 of rehabilitation performed five days per week.
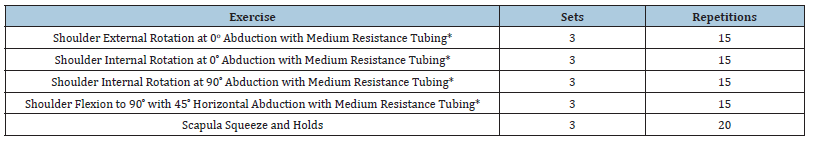
*Exercise performed in conjunction with blood flow restriction at 50% maximum brachial artery outflow.
Week 4: After conferring with the orthopedic surgeon, the patient’s progress in terms of pain, strength and range of motion warranted the initiation of a return to throwing protocol. The patient was also cleared to begin progressing back to hitting. During this phase, the patient continued receiving cupping therapy as needed for post activity soreness. After activity, the patient also underwent a sequential compression treatment using the Norma Tec Pulse 2.0 Recovery System (HyperIce, Irvine, CA) for 30 minutes. The intensity of rehabilitation exercises was also increased as shown in Table 3.
Table 3:Week 4 of rehabilitation performed five days per week.
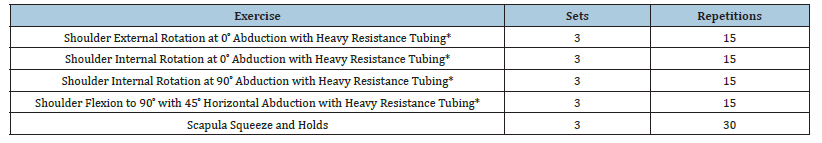
*Exercise performed in conjunction with blood flow restriction at 50% maximum brachial artery outflow.
As the patient began throwing and swinging, he noted that he felt fatigue in his shoulder more rapidly than prior to the injury. The patient also reported occasional pain in the anterior shoulder when throwing, though the intensity of the pain was significantly less than immediately following the injury. At this time, the athletic trainer recommended the use of an external dynamic arm stabilizer (The Kinetic Arm K1 BraceTM, The Perfect Arm, LLC, Chamblee Georgia) seen in Figure 1. After wearing the arm stabilizer for one throwing and swinging session, the patient reported a decrease in feelings of fatigue and a decrease in episodes of pain when throwing. Given these results, the patient agreed to using the arm stabilizer throughout his rehabilitation process. During this time, the patient also expressed his desire to play in his team’s upcoming post season competitions. Through consultation with the athletic trainer, team physician, and orthopedic surgeon, the patient provided informed consent to accelerate his return to participation to align with his goals. In this accelerated process, the patient was instructed to take the minimum number of throws and swings possible during practice to ensure he was prepared for participation in competitions. Throughout this process, the patient was told to report any increases in pain or prolonged soreness. Frequency of cupping therapy was increased to three times a week to increase blood flow and promote recovery.
Figure 1:Kinetic Arm K1 BraceTM.

Week 5-6: The patient experienced post-activity soreness to increase frequency, volume, and intensity of practice sessions. The patient stated that when wearing the arm stabilizer he did not experience any episodes of instability or pain. Ultimately, the patient was able to compete in all four of his team’s post season competitions with no complications. Following each competition, the patient underwent sequential compression, followed by cupping therapy to mitigate the effects of post-activity soreness. At the conclusion of the patient’s season, the patient consented to abstaining from baseball activities for a month while still completing rehabilitation and treatment sessions.
Week 10+: After a month of rest from baseball specific activities, the patient resumed sport specific activities. Progression to returning to sport specific activity was prolonged, due to the patient being in his offseason. At this time, the patient obtained an updated model of the external dynamic arm stabilizer (The Kinetic Arm K2 BraceTM, The Perfect Arm, LLC, Chamblee Georgia) seen in Figure 2. The patient initiated a maintenance rehabilitation program at this time, consisting of the exercises listed in Table 3 being performed three times a week. Sequential compression and cupping therapy were used when indicated due to post activity soreness. Aside from occasional soreness, the patient has been able to maintain an uncomplicated return to activity in preparation for his upcoming season.
Figure 2:Kinetic Arm K2 BraceTM.

Discussion and Conclusion
This case study describes the expedited return to play of a collegiate baseball player suffering from a glenohumeral labrum tear. Through the combination of compliance with the rehabilitation program and use of an external dynamic arm stabilizer, the patient was able to participate in competitions relatively quickly following injury. This case study is noteworthy, as it appears to be the first publication to describe the use of an external dynamic arm stabilizer to facilitate an uncomplicated expedited return to participation in a baseball player suffering from a glenohumeral labrum tear. Further research is needed to validate the use of an external dynamic arm stabilizer for use in overhead athletes. Additionally, future studies should focus on analyzing the amount of force attenuation that occurs at the shoulder and elbow during overhead physical activity when wearing an external dynamic arm stabilizer. While this paper describes a single case study, it describes the successful use of an external dynamic arm stabilizer for allowing a patient to return to activity sooner than expected. The paper also includes a detailed rehabilitation protocol that was used in conjunction with the stabilizer.
- Anz AW, Bushnell BD, Griffin LP, Noon TJ, Torry MR, et al. (2010) Correlation of torque and elbow injury in professional baseball pitchers. Am J Sports Med 38(7): 1368-1374.
- Braun S, Kokmeyer D, Millett PJ (2009) Shoulder injuries in the throwing athlete. J Bone Joint Surg Am 91(4): 966-978.
- Chalmers PN, Erickson BJ, Ball B, Romeo AA, Verna NN (2016) Fastball pitch velocity helps predict ulnar collateral ligament reconstructions in Major League Baseball pitchers. Am J Sports Med 44(8): 2130-2135.
- Erickson BJ, Harris JD, Tetreault M, Bush-Joseph C, Cohen M, et al. (2014) Is Tommy John surgery performed more frequently in major league baseball pitchers from warm weather areas? Orthop J Sports Med 2(10): 1-6.
- Gilliam BD, Douglas L, Fleisig GS, Kyle TA, Kylie AM, et al. (2018) Return to play and outcomes in baseball players after superior labral anterior-posterior repairs. Am J Sports Med 46(1):109-115.
- Cage SA, Volpi JD, Jacobsen AP, Trail LE, Warner BJ, et al. (2022) Competitive baseball pitchers’ use of wearable technology. Res Inves Sports Med 9(1): 781-785.
© 2023 Cage SA. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






