- Submissions

Full Text
Research & Investigations in Sports Medicine
Competitive Sport and its Impact on Sleep Quality in Children: First Results of an Innovative Pilot Study
Esther Solano-Pérez1, María Castillo-García1, Carlota Coso1, Sofia Romero-Peralta1, Lourdes Guerra2, María Esther Viejo-Ayuso1,3, Laura Silgado-Martínez1, Leticia Álvarez-Balado1, Eduardo Laviña-Soriano1, Sonia López-Monzoni1, Rosa Mediano San Andrés1, Irene Cano-Pumarega3,4, Manuel Sánchez-de-la-Torre3,5,6, Carlos Egea3,7 and Olga Mediano1,3,8*
1Pneumology Department, University Hospital of Guadalajara, Spain
2OSI Araba, Spain
3Center for Biomedical Research in Respiratory Diseases Network (CIBERES), Spain
4Pneumology Department, Hospital Universitario Ramón y Cajal, Spain
5Respiratory Department, Hospital Universitario Arnau de Vilanova, Spain
6Department of Nursing and Physiotherapy, Universidad de Lleida, Spain
7Respiratory Department, Hospital Universitario IRB de Araba, Spain
8Faculty of Medicine, Autonomous University of Madrid, Spain
*Corresponding author:Olga Mediano, Sleep Unit, Pneumology Department, University Hospital of Guadalajara, 19002 Guadalajara, Spain
Submission: May 14, 2023;Published: May 23, 2023

ISSN 2578-0271 Volume9 Issue4
Abstract
There are data about the impact of sleep quality on the performance of athletes in adults, but little is known in children. Our objective was to evaluate the sleep quality in children who practiced high-performance sports and analyze how it influenced their night rest. Preliminary data of an observational pilot study where 20 children between 4-17 years who practiced sports are presented. Variables of daytime and nighttime activity were recorded for 7 days using an Actimeter. Anthropometric variables and Morningness / Eveningness questionnaires were also collected. Mean Total Sleep Time (TST) was 7.37 (±0.37) hours, presenting 40% of days with a TST lower than 7 hours. 100% of the children went to bed later than 10:00pm, 75% later than 11:00pm and 20% later than 00:00am. 35% of the children presented a severe fragmentation index FI (>40) and 60% a moderate FI (20-40). The 80% had data of insufficient sleep with phase delay syndrome, where only 10% presented normal values. The impact of high-performance sports on sleep quality in children is not negligible: Sleep hygiene disorders negatively decrease the sleep hours and increase the fragmentation and insufficiency of sleep, which could affect their sports performance.
Keywords:Sport; Sleep quality; Pilot study; Sport performance
Abbreviations:TIB: Time in Bed; TST: Total Sleep Time; WASO: Wake Time After Sleep Onset; FI: Fragmentation Index; SI: Sleep Insufficiency; PDS: Phase Delay Syndrome
Introduction
Good sleep quality has a proven positive impact on sports performance. Therefore, it is expected that in high-performance sports, special care is taken to sleep quality as a tool to obtain better results. There are data about the impact of sleep quality on the performance of athletes in adulthood, however, there is little knowledge about this impact in children. Previous studies analyzing the quality of sleep in athletes who practice high-performance sports have shown that elite athletes present a greater alteration of sleep architecture than expected [1].
Quality and quantity of sleep depend independently on bedtime resistance, frequent awakening during the night, and/or difficulty to fall asleep. The clinical repercussions, therefore, are due to lack of sleep and include both nocturnal and daytime disturbances. These may include during the night, sleep latency greater than 20 minutes, Wake Time After Sleep Onset (WASO) greater than 60 minutes, nocturnal awakenings; and excessive daytime sleepiness, attention and memory difficulties, behavioral problems, and poorer school performance during the day [2].
The study of the circadian system is performed by analyzing certain markers, indirect measures of the rhythm generated by the circadian center (sleep-wake rhythm). The most important markers are physical activity, Core Body Temperature (CBT) and plasma melatonin and cortisol secretion, which are autonomously regulated by the exogenous synchronizers of the circadian system, which are the light and ambient temperature [3,4].
Different studies in the field of sports have considered the influence of biological rhythms on people’s behavior or performance [3-7]. At certain hours of the day, doing physical exercise or solving a mental task becomes easier, achieving superior performance. Thus, morning, afternoon and evening are times of the day in which significant fluctuations in the physical and Psychological performance of individuals have been described, whose variation depending on the time slot can represent between 10% and 15% improvement in performance [8]. In fact, the yield is higher at different moments of the day together with temperature [9], which fluctuates throughout the day with high values during the morning that decrease around 08:00pm and are minimal around 06:00am. Thus, gross motor performance is maximum between 06:00-08:00pm [9], and cognitive performance, coordination and accuracy are maximum between 10:00am - 12:00am [3].
Sleep behavior is commonly monitored with actimetry systems [9,10], given their availability and low cost. These Actimeters, based on accelerometry, are non-invasive and inexpensive devices, effective for estimating the quality and quantity of sleep. Within measurement methods of the circadian rhythm markers, an individual motor activity is recorded by a device placed on the non-dominant wrist in order to estimate sleep-wake cycles by measuring sleep duration, latency and efficiency, time in bed, nocturnal activity and fragmentation index [9-12]. Moningness/ Eveningness can determine circadian typologies (morning, evening and intermediate) [13,14].
Poor sleep quality in high-performance athletes could mean that greater sporting demand leads to a state of anxiety that interferes with sleep quality, resulting in lower performance [10]. In addition, training schedules do not always respect the rules established for good sleep hygiene, such as avoiding intense exercise in the late afternoon and respecting an adequate number of hours of sleep. Based on this hypothesis, we wondered whether high-performance sport has the same effects on the pediatric population. Nowadays, children between 4 and 17 years old play sports at a competition level without knowing the impact of this practice on their quality of sleep and vice versa. Therefore, we asked ourselves about the impact of sports performed at competition level in school-age children, and the possible repercussions on their health. The purpose of this pilot project was to evaluate the feasibility of a larger-scale study that aims to assess the quality of sleep in children who perform a sport at competition level and how this influences their night rest.
Materials and Methods
Hypothesis
High-performance sport could have a negative impact on the sleep quality of children who play sports at a competitive level.
Objectives
5.2.1. Principal: Evaluate the feasibility of a larger-scale study that aims to assess sleep quality, through the presence of circadian rhythm disorders, in children between 4 and 17 years who practice a high-performance sport, and to analyze how it influences this in their night rest.
Secondaries:/
A. Assess sleep efficiency in high-performance athletes.
B. Assess the hours of sleep in this population.
C. Assessment of sleep fragmentation through awakenings
during sleep (WASO) and number and index of awakenings.
D. Define the primary variable for the future research study.
Methodology
Design and population: Observational pilot study. 20 boys and girls from the province of Guadalajara (Spain) between 4 and 17 years were recruited from 3 different sports: rhythmic gymnastics, football and swimming.
I. Inclusion Criteria
A. Boys and girls between 4 and 17 years who do sports at a
competition level.
B. Informed Consent (IC) with parental authorization.
C. Belong to a high-performance club and be selected by
their coach.
II. Exclusion Criteria
A. Any situation that may imply the inability to carry out the
methodology.
B. Chronic or disabling disease.
C. Suffering from a previously diagnosed sleep disorder.
III. Withdrawal Criteria
a. Patients could withdraw from the study at any time. The
investigator could retract participants from the study for the
following reasons, among others:
b. Non-compliance with the procedures and
recommendations by the participant.
c. Voluntary withdrawal.
d. Any major adverse event that limits the capacity to
participate in the study.
e. Loss of contact during follow-up.
f. Investigator’s decision that continuation in the study
would not be the best for the participant (e.g., intercurrent
disorder or disease requiring the use of prohibited drugs or
treatments).
At the time of leaving the study, the main reason for withdrawal should be recorded and, if possible, the participant should be reassessed. The children selected based on their sports performance had to meet all the inclusion criteria and none of the exclusion criteria. Once approved by the Ethics and Clinical Trials Committee and with the IC signed by parents and children over 12 years of age, the following procedures were carried out.
Procedure
First, all participants completed two sleep questionnaires: the BEARS questionnaire and the Morningness-Eveningness Scale for Children (MESC) questionnaire. They assess Morningness/ Eveningness in order to determine circadian typologies (morning, evening, and intermediate). In the primary health care area, the BEARS questionnaire (B=Bedtime Issue, E=Excessive Daytime Sleepiness, A=Night Awakenings, R=Regularity and Duration of Sleep, S=Snoring) can help to identify children with sleep disorders with five questions about the mentioned categories. It is an easyto- use child sleep screening tool that significantly increases the sleep information recorded [15]. On the other hand, the MESC questionnaire is designed to assess sleep habits in children and, as well as BEARS questionnaire, it can help to identify sleep disorders. It contains 10 items about the quantity and quality of sleep, the time it takes for the child to fall asleep, the frequency of nighttime awakenings, and other sleep-related factors [16].
In addition, the Actiwatch Spectrum (Philips ©) actimeter was placed on the non-dominant wrist for one week in a noncompetitive training period Figure 1. The device could be removed during training if it was a problem for the athlete, as well as for cletaning and for anything that could be a risk for the child, recording said removals in a diary. In the same vein, in said diary the periods of sleep and wakefulness as well as the periods of training were collected.
Figure 1:Actiwatch spectrum ® (Philips) device.

Study variables
Using said actimeter, variables about daytime and nighttime motor activity were recorded.
Anthropometric and demographic variables:Age, Gender, Weight, Height and Body mass index.
Activity variables:Practiced Sport, Training Schedules, Daily Diary on Awake/Bedtimes, Naps, Meals, Physical Activity (duration and intensity), Social Habits and School Schedules.
Sleep variables:Bedtime, Awake Time, Body Position, Nocturnal Activity, Time In Bed, Time Immobile In Bed, Total Sleep Time, Sleep Latency, Sleep Efficiency, number and rate of awakenings (fragmentation).
Statistical analysis
Descriptive statistics of the mean (standard deviation) are estimated for quantitative variables with a normal distribution.
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki (1964), the Council of Europe Convention on Human Rights and Biomedicine (1997), and the regulations on biomedical research, protection of personal data (Law 14/2007 on Biomedical Research). All patients were informed about the study and asked to express their IC. All data were processed in accordance with the personal data protection law (Organic Law 15/1999, 13-12). In all documents, patients were only identified by the identification code. The investigator maintained an independent and confidential recruitment record that allowed the identification codes to be linked to the names and addresses of the patients. The project was approved by the Ethics and Clinical Trials Committee of the Hospital Universitario de Guadalajara (2019.01.PR).
Result
A total of 20 participants were analyzed. Regarding the clinical characteristics and anthropometric variables, described in Table 1, the mean age was 13,42 (±2,81) years, with a body mass index of 18,31 (±3,24). The Actigram generated from the information collected from the Actiwatch® is shown in Figure 2. During one week, the signals from the variability in sleep schedule, sleep time, and sleep quality data were collected. From this information, together with that provided by the diary, the following results were obtained: the mean Total Sleep Time (TST) was 7,37 (±0,37) hours and the mean minimum TST was 6,04 hours (±1,33), presenting 40% of the nights a TST lower than 7 hours. Sleep latency was 19,26 (±9,83) minutes and WASO was 30,38 (±11,19) minutes. The participants showed an efficiency of 86,10 (±4,62) and 35,95 (±8,86) awakenings Table 2.
Figure 2:Example of an actigram of one week.
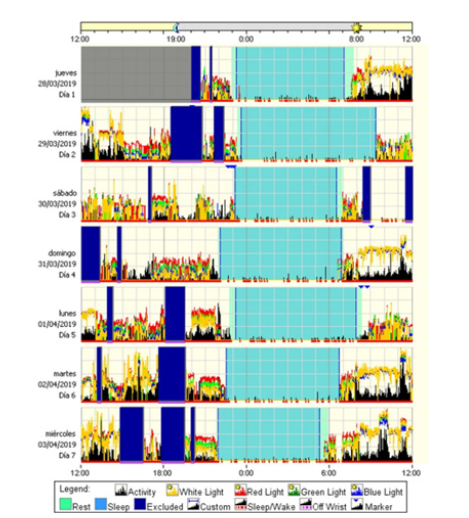
Table 1:Clinical characteristics and anthropometric variables.
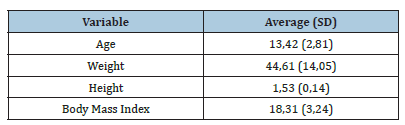
Table 2:Sleep variables

Table 3:Prevalence of sleep variables.
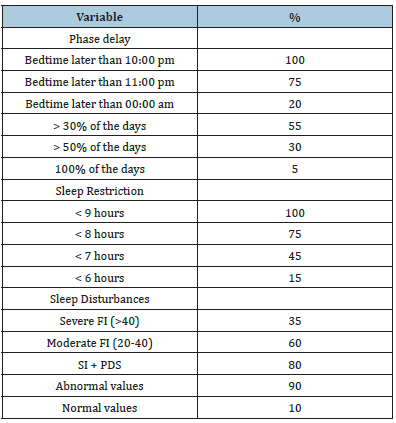
Bedtime hour of 100% of the children was later than 10:00pm, 75% went to bed later than 11:00pm and 20% later than 00:00am, of which, 55% did it more than 30% of the studied nights, 30% on more than half of the nights, and 5% on all nights. The sleep duration of all of them was less than 9 hours, most sleeping less than 8 hours (75%): 45% slept less than 7 hours and 15% slept less than 6 hours Table 3. 35% of the participants presented a severe Fragmentation Index (FI) (>40) and 60% a moderate FI (20-40). 80% had data of Sleep Insufficiency (SI) together with Phase Delay Syndrome (PDS), where only 10% presented normal values in relation to these parameters Table 3.
Discussion
In this pilot study carried out on children who practice highperformance sport, an impact on sleep quality has been observed, mainly affecting their night rest. In the global pediatric population, most children between 4 and 10 years sleep from 9 to 11 hours [17,18], which is the sleep time recommended by the Spanish Sleep Society in 2016 [19]. Besides, the majority of European studies analyzing the quantity of sleep-in adolescents report less than 8 hours per night [20-22], decreasing with age due to a combination in the routine of going to bed late and getting up early, regardless of the physical activity they perform. However, there is controversy with the results published in Spain by the Instituto Nacional de Estadística in 2023 [18], which reports more than 8 hours of sleep in this population, maybe because they included nap time in their statistics. According to these publications and considering that the recommendation for this age is between 8 and 10 hours [19,23], the adolescents in our study did not meet the recommended hours of sleep, presenting a reduced TST and sleep deprivation.
As mentioned above, the sleep schedule is mainly determined by a circadian component. Quality sleep begins approximately two hours after the onset of melatonin production in dim light conditions (Dim-Light-Melatonin-Onset [DLMO]) [2], which coincides with the decrease of CBT. For its part, the end of sleep occurs spontaneously about two hours after the increase in CBT and the cessation of melatonin secretion. This quality sleep is characterized by an adequate duration, normal sleep structure (with light, REM, and deep sleep phases) and absence of interruptions, which allows one to wake up feeling rested. A worse sleep quality would take place when the sleep schedule is far from this DLMO. However, the DLMO of children is commonly disturbed: school-age children go to bed and wake up early, whereas teenagers delay it with the onset of puberty [19]. The participants in the training period analyzed in our study delayed going to bed, altering their DLMO and causing PDS in most of them. Hence, there is an association between later sleep timing and shorter sleep duration since the studied population has a fixed school or institute schedule. Thus, the early awakening time together with the reduced TST, produced them Sleep Insufficiency (SI), which was far from normal values in a small percentage of them..
The effect of physical activity on the circadian system can be different depending on the time of day. Different studies have shown that performing intense exercise during the 2 hours next to the usual sleep time can cause PDS of internal rhythms and difficulty in falling asleep, in addition to presenting a light and fragmented sleep. Nocturnal exercise has been attributed to a possible increase in sympathetic arousal, which increases cortisol levels and CBT, leading to a nocturnal alert level that causes lighter sleep and favors the appearance of awakenings during the night [24,25]. According to this evidence, high-performance sports carried out at the end of the day led to a higher FI in the participating population, being moderate in most of them, and even severe in some cases. Moreover, the majority of this population presented abnormal values of FI together with PDS. However, the lack of sleep in this population has not been reflected in clinical repercussions such as the increase in sleep latency or wake time after sleep onset.
Overall, these findings could lead to other sleep and mental health disorders due to later and reduced sleep time of these participants [26,27]. On the one hand, high school pressure increases with age, being more common in adolescents, and being associated with mental health disorders. On the other hand, the use of electronic devices (video games and social networks) at bedtime could affect sleep, independently of sport, through several mechanisms: the direct reduction of available sleep time and the melatonin-suppressing effect of bright light from the screen, one of the most relevant factors in the context of insomnia [28,29] and severe psychopathologies that include depression [30].
In summary, the disturbance of sleep hygiene measures, such as intense exercise in the hours before going to bed or not maintaining a regular sleep schedule, negatively affects the quality of sleep, mainly altering the TST and the circadian rhythm (phase delay and high sympathetic activity), which in turn can lead to a decrease in sports performance. It is important to highlight that lack of sleep in children can also have a negative impact on their school performance, physical and mental health, as well as their behavior and general well-being [31-33].
Several limitations and strengths in our study deserve discussion. The strengths include the collection of data from different sports, in addition to carrying out the same methodology for all of them, facilitating the analysis of the data and obtaining more rigorous results. On the other hand, The study has several limitations. Firstly, the sample size is small, so significant generalizations could not be obtained from the data. For the same reason, it was not possible to carry out the statistical analysis by subgroups, differentiating by gender or sport, among others. It should be taken into account that this is a tentative pilot study to stablish the methodology for a controlled trial. Thirdly, data from the control group were not collected, preventing the comparison between them in order to obtain significant differences in the quality of sleep-in high-performance athletes. Finally, other factors that could alter sleep timing and bedtime have not been evaluated, such as the use of electronic devices, which are widely used nowadays. Different lines of future research could be considered: evaluating different periods of activity (training, competition and rest) and looking for differences in sleep patterns based on gender, age, and sport. More research studies with a larger sample size are needed to evaluate this sport/sleep relationship.
Conclusion
This pilot project has made it possible to determine that the impact of high performance sports on the quality of sleep in children is not negligible. It translates into a manifest phase delay, decreased hours of sleep, increased fragmentation and insufficient sleep, which could affect their athletic performance.
Author Contributions
Conceptualization, O.M. and L.G.; methodology, O.M. and L.G.; formal analysis, L.G.; investigation, E.S-P., M.C-G., C.C., S.R-P., M.E.V-A., L.S-M., L.A-B., E.L-S., S.L-M., R.M SA., I.C-P., M.S-T., C.E., O.M.; resources, O.M.; data curation, R.M SA., M.E.V-A., L.S-M.; writingoriginal draft preparation, E.S-P. and C.C.; writing-review and editing, O.M.; supervision, O.M.; project administration, R.M SA.; funding acquisition, O.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by funds received by the ISCIII (PI18/00565 and PI22/01653) and FEDER, the Spanish Respiratory Society (Sociedad Española de Neumología y Cirugía Torácica- SEPAR (928-2019), NEUMOMADRID (Sociedad Madrileña de Neumología y Cirugía Torácica) and Philips.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics and Clinical Trials Committee of the Hospital Universitario de Guadalajara (2019.01.PR).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
Not applicable.
Acknowledgment
We greatly appreciate the participation and cooperation of all children and their parents in the study. We also thank the Spanish Sleep Network for their work on the KIDS TRIAL study. Philips was not involved in the scientific discussion or the writing of the paper.
Conflicts of Interest
The authors declare no conflict of interest
References
- Halson SL (2014) Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Med 44(S1): 13-23.
- Arboledas GP, Insuga VS, Luque MJJ, Gomariz CF, Vicario IH, et al. (2017) Insomnia in children and adolescents. Consensus document. Annals of Pediatrics 86(3): 165.e1-165.e11.
- Atkinson G, Reilly T (1996) Circadian variation in sports performance. Sports Med 21(4): 292-312.
- Loat CER, Rhodes EC (1989) Jet- Lag and human performance. Sports Med 8(4): 226-238.
- Adan A (1992) The influence of age, work schedule and personality on morningness dimension. International Journal of Psychophysiology 12(2): 95-99.
- Erren TC, Groß JV, Kantermann T, Kuffer L (2014) Chronobiology and competitive sports: Recent studies and future perspectives. Chronobiol Int 31(5): 746-747.
- Knufinke M, Nieuwenhuys A, Geurts SAE, Coenen AML, Kompier MAJ (2018) Self-reported sleep quantity, quality and sleep hygiene in elite athletes. J Sleep Res 27(1): 78-85.
- Garcia MA, Aguado F, Cuartero J, Calabria E, Jiménez R Sueño, et al. (2003) Sleep, rest and sports performance in young competitive athletes. Sport Psychology Magazine 12: 181-195.
- Aschoff J (1967) Human circadian rhythms in activity, body temperature and other functions. Life Sci Space Res 5: 159-173.
- Doherty R, Madigan SM, Nevill A, Warrington G, Ellis JG (2021) The sleep and recovery practices of athletes. Nutrients 13(4): 1330.
- Bjorvatn B, Pallesen S (2009) A practical approach to circadian rhythm sleep disorders. Sleep Med Rev 13(1): 47-60.
- Sack RL, Auckley D, Auger RR, Carskadon MA, Wright KP, et al. (2007) Circadian rhythm sleep disorders: Part I, Basic principles, Shift work and Jet lag disorders. An American Academy of Sleep Medicine Review. Sleep 30(11): 1460-1483.
- Horne JA, Ostberg O (1976) A self-assessment questionnaire to determine Morningness-Eveningness in human circadian rhythms. Int J Chronobiol 4(2): 97-110.
- Sateia MJ (2014) International classification of sleep disorders-Third Edition. Chest 146(5): 1387-1394.
- Owens JA, Dalzell V (2005) Use of the ‘BEARS’ sleep screening tool in a pediatric residents’ continuity clinic: a pilot study. Sleep Med 6(1): 63-69.
- Díaz-Morales JF, Sorroche MG (2008) Morningness-Eveningness in adolescents. Span J Psychol 11(1): 201-206.
- Whiting S, Buoncristiano M, Gelius P, Abu-Omar K, Pattison M, et al. (2021) Physical activity, Screen time, and Sleep duration of children aged 6-9 years in 25 countries: An analysis within the WHO European childhood obesity surveillance initiative (COSI) 2015-2017. Obes Facts 14(1): 32-44.
- Descanso Y, Ejercicio Físico (2023) Determinantes de la salud. Cifras Absolutas, National Statistics Institute, Spain.
- Merino AM, Álvarez RLA, Madrid PJA, Martínez MMÁ, Puertas CFJ, et al. (2016) Healthy sleep: Evidence and guidelines for action. Official document of the Spanish Sleep Society. REV Neurol 63(S2): 1-27.
- García JMÁ, Salcedo AF, Rodríguez AFM, Redondo MMP, Monterde Aznar ML, et al. (2004) Prevalence of sleep disorders in adolescents from Cuenca, Spain. REV Neurol 39(1): 18-24.
- Garaulet M, Ortega FB, Ruiz JR, Rey-López JP, Béghin L, et al. (2011) Short sleep duration is associated with increased obesity markers in European adolescents: Effect of physical activity and dietary habits. The HELENA Study. Int J Obes 35(10): 1308-1317.
- Galan LP, Domínguez R, Gísladóttir T, Sánchez-Oliver AJ, Pihu M, et al. (2021) Sleep quality and duration in European adolescents (The AdolesHealth Study): A cross-sectional, Quantitative study. Children 8(3): 188.
- Paruthi S, Brooks LJ, D’Ambrosio C, Hall WA, Kotagal S, et al. (2016) Consensus statement of the American academy of sleep medicine on the recommended amount of sleep for healthy children: Methodology and discussion. J Clin Sleep Med 12(11): 1549-1561.
- Hernández Gómez A (2023) Sleep disorders and their influence on behavior. Med Wave 6(2):
- López Flores M (2018) Sleep quality and its relationship with sports practice. Universidad de León, Spain.
- Coico Lama AH, Diaz Chingay LL, Castro-Diaz SD, Céspedes-Ramirez ST, Segura-Chavez LF, et al. (2022) Association between sleep disturbances and mental health problems in medical students during the COVID-19 pandemic. Educación Médica 23(3): 100744.
- Dutil C, Podinic I, Sadler CM, da Costa BG, Janssen I, et al. (2022) Sleep timing and health indicators in children and adolescents: a systematic review. Health Promot Chronic Dis Prev Can 42(4): 150-169.
- de Zambotti M, Goldstone A, Colrain IM, Baker FC (2018) Insomnia disorder in adolescence: Diagnosis, impact, and treatment. Sleep Med Rev 39: 12-24.
- Yen CF, Ko CH, Yen JY, Cheng CP (2008) The multidimensional correlates associated with short nocturnal sleep duration and subjective insomnia among Taiwanese adolescents. Sleep 31(11): 1515-1525.
- Harbard E, Allen NB, Trinder J, Bei B (2016) What’s keeping teenagers Up? Prebedtime behaviors and actigraphy-assessed sleep over school and vacation. J Adolesc Health 58(4): 426-432.
- Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM (2010) The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med Rev 14(3): 179-189.
- Qiu J, Morales MI (2022) Associations between Sleep and Mental Health in Adolescents: Results from the UK Millennium Cohort Study. Int J Environ Res Public Health 19(3): 1868.
- Paiva T (2015) Sleep Deprivation, Sleep Stealers and Risk Behaviors in Portuguese Adolescents - A Cross-Cultural Comparison. MOJ Public Health 3(1): 204-212.
© 2023 Olga Mediano. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






