- Submissions

Full Text
Research & Investigations in Sports Medicine
A Case of Extranodal Nk/T Cell Lymphoma Found in Left Leg
Hongli Xia1, Guoli Liu1, Ansen Wu1, Rong Zhao1, Fei Liu2 and Mincai Li1,2*
1Deparment of Vascular surgery, Xianning Central Hospital, China
2School of Basic Medical Sciences, Hubei University of Science and Technology, China
*Corresponding author:Li Mincai, Hubei Province Key Laboratory on Cardiovascular, Cerebrovascular and Metabolic Disorders, Hubei University of Science and Technology, Xianning 437100, P.R. China
Submission: August 29, 2022;Published: February 24, 2023

ISSN: 2577-1914 Volume9 Issue3
Abstract
Lymphoma is a common disease in the blood system. NK/T cell lymphoma is a rare lymphoma which appeared the abnormalities lymphocyte and the impaired function, following the symptoms of the uncontrolled infection and the tissue damage. We report a case of non-nasal NK/T-cell lymphoma in the leg, which provides for the diversity of NK/T-cell lymphoma.
Introduction
Hemangioma is a common disease in vascular surgery. It is the great benefit for the detection of blood flow status through the vessel imaging methods, which is the basis and key of diagnosis for hemangioma [1]. It can provide great help to detect the blood flow state of hemangioma by imaging method, and it is also the basis and key point of diagnosis of hemangioma. However, it is difficult to diagnose for hemangioma of deeper tissues, the imaging changes may not be specific and may lead to difficult diagnosis [2,3]. Among the patients with hemangioma, we retrospectively analyzed a patient whose mass occurred in the muscle tissues of leg. The imaging of B-mode ultrasound diagnosed as hemangioma and the pathological diagnosis is administrated as the lymphoma after surgery [4]. The report is following:
Case Report
A 56-year-old female patient, who found a mass in her left leg more than 6 months ago, was hospitalized. Before June, swelling and discomfort of the left calf appeared, resulting in limited walking; after anti-inflammatory treatment in the local area, the edema has subsided, and the left calf touched an egg-sized mass. Physical examination: the vital signs were stable. A 3.5cm * 2cm mass was touched on the posterior medial side of the left calf, which was not raised on the skin. The texture is hard when touched, and the mobility is poor. B-ultrasound in the clinic: mixed echo foci in the subcutaneous muscular layer of the left lower limb, considering as hemangioma [5-7].
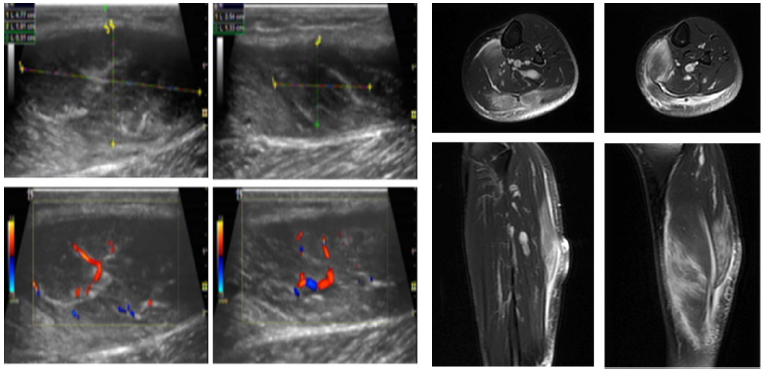
The patient was admitted to the hospital with “hemangioma of the left lower limb”. She has a history of hypertension and self-complained taking antihypertensive drugs, which has a good effect on blood pressure control. She has a history of sinusitis and pharyngitis, intermittent seizures, taking drugs, and no attack within six months. After admission, MRI examination suggested that “the left calf soleus muscle and gastrocnemius muscle abnormal signal, consider the possibility of gastrocnemius space syndrome.” After improving the relevant examination before operation, according to the evaluation of the condition, no contraindication was found, and the left leg mass resection was performed under intraspinal anesthesia The patient was in a prone position, after disinfecting the towel, on the large posterior lateral mass of the left calf make a skin incision to separate the subcutaneous tissue and the deep fascia. A 5cm * 3cm mass was seen on the gastrocnemius muscle. Whose color was different from the muscle tissue? It was lighter in color than gastrocnemius muscle and has no adhesion with the surrounding tissues. A part of the tumor extends to the medial side of the triceps of the calf and continues to separate along the medial side of the gastrocnemius muscle, separating 3.5 cm * 2cm of the tumor, which is not clear from the gastrocnemius muscle. Carefully separate and remove the diseased tissue (Figure 1).
Figure 1: B-ultrasound image of the patient’s lower limbs, showing abundant blood flow (left image). MRI image showed abnormal signal (right image).
According to the intraoperative findings, considering the possibility of hemangioma is less likely. The surrounding lesion tissue was removed as far as possible, and the residual end of gastrocnemius muscle was sutured to the synergistic muscle. After washing the surgical field of vision with normal saline for many times with no obvious bleeding) a drainage strip was given, and the deep fascia, subcutaneous tissue, and skin were intermittently sutured after the gauze was counted, and the elastic bandage was used for pressure bandaging. Anti-infection, lowering blood pressure, regulating fat, protecting liver and kidney and other symptomatic treatment were performed after the operation. The surgically removed specimens were sent for medical examination: the hospital’s surgical pathology report: a small number of skeletal muscles and a large number of coagulative necrotic tissues were observed under the microscope. A small amount of lymphocytelike cells and nuclear debris remained around the blood vessels in necrotic tissue and the size of the cells is not equal, and the morphology is multiform. Combined with immunohistochemistry, the possibility of extranodal NK/T cell lymphoma cannot be ruled out. Immunohistochemistry: CD2, CD3, CD43, CD56 (+), Ki-67 (95% +) , other CD4, CD5, CD8, CD30, CD31, CD68, CD138, Desmin, CKpan, MPO (- ), Acid-fast staining (-).
According to the recommendations of the pathology report, we need to obtain further diagnosis of the higher-level hospital. The pathological consultation opinions of a third class hospital in Wuhan are as follows: the left lower extremity gastrocnemius extranodal NK/T cell lymphoma (nasal type) with extensive necrosis. The tumor tissue is necrotic with only a small amount of degenerated tumor cells, whose immunohistochemistry showed: CD56, GrB, TIA-1 (+), CD3, CD30, C-myc (scattered +), Ki-67 about 95%[8]. Other CD5, CD20, CD79a, PAX-5, CD10, BCL-2, BCL-6, CyclinD1, SOX11, CD21, Mum-1, ALK-1, DES, MyoD1, Myogenin are all (-). Molecular detection: EBER CISH (+) [9].
Discussion
Hemangioma is a frequently-occurring and common disease which can get satisfactory results after surgical treatment. In this case, on the basis of clinical symptoms, signs, auxiliary examination B-ultrasound examination, MRI examination suggested the possibility of hemangioma. However, it was found the mass was not clear and the color was lighter than the muscle tissue during the operation. It was not the appearance of a blood vessel rich in blood vessels, which ruled out the hemangiomas. Two masses were found during the operation. The lesion tissue was dark and light, the blood vessels were not rich, and the boundary with the surrounding tissue was unclear. Considering the possibility of malignant lesions, the whole excision was performed, and the surrounding affected tissues were removed and the lesion was successfully isolated. The operation was successful.
When it was sent for tissue examination after the operation, it was found to be a large amount of coagulative necrotic tissue, which was consistent with the pale color of the lesion tissue in the surgical field of vision and consistent with the non-adhesion of the lateral mass and muscle tissue during the operation. In large areas of necrotic tumor tissue, we found a small number of denatured tumor cells. We think that this part of the tissue belongs to the medial mass. We carefully separated and removed the diseased tissue as far as possible in order to remove the tumor. Skeletal muscle tissue is also mentioned in the medical report. Also in these non-necrotic tissues, immunohistochemical diagnosis was extranodal NK/T cell lymphoma (nasal type [10,11]. It is a rare case that our clinicians should pay attention to.
In the course of treatment waiting for pathological reports, we also found some abnormal clinical phenomena, which have important implications for the existence of tumors. Firstly, the liver function index of the patient is unstable, and five times successively alanine aminotransferase (0 147, 180, 196, 177, 85 U/L, aspartate aminotransferase 83, 170, 95, 119, 45 U/L, glutamine transpeptide. The enzyme is 166, 259, 324, 519, 496 U/L, after liver protection treatment, and finally adjusted to the normal range. Secondly, Looking for the cause of liver disease, in order to find the cause of abnormal liver function, we give out all types of hepatitis virus infection, alpha-fetoprotein test, liver disease autoantibody test, and the results are negative. In order to exclude the impact of autoimmune diseases on the liver, when the ENA test was performed, it was found that the anti-Histone antibody was weak (+) and the anti-SMD1 antibody (+). Check for infectious diseases and conduct Anti-Nuclear Antibody (ANA) inspection. It is found that EB virus core antigen IgG antibody 3.740 and EB virus capsid antigen IgG antibody 3.790. These results, especially the EB virus examination, are consistent with the subsequent pathological examination: EBER CISH (+) at the lesion site.
Ethics
Written informed consent was obtained from the patient for publication of this case report. The report was approved by the institutional review committee of our hospital.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Hwang SL, Wu CH, Chen YT, Tai HT, Cheng WC, et al. (2012) Monoparesis of the leg caused by thoracic vertebral hemangioma: A case report. Neurol Sci 33(3): 709-710.
- Tarca E, Cojocaru E, Rosu ST, Lăcrămioara IB, Petru P, et al. (2019) Differential diagnosis difficulties related to infantile hemangioma - Case report and literature review. Rom J Morphol Embryol 60(4): 1375-1379.
- Aloyouny AY, Mehanny MS, Albagieh HN, Wafa Mohammed A, Soad Mahmoud M, et al. (2020) Intramuscular hemangioma in the zygomaticus muscle: A rare case report presentation and diagnosis. Int J Surg Case Rep 74: 42-45.
- Deka JB, Deka NK, Shah MV, Nidhi B, Anna LN, et al. (2020) Intraneural hemangioma in Klippel-Trenaunay syndrome: Role of musculo-skeletal ultrasound in diagnosis-case report and review of the literature. J Ultrasound 23(3): 435-442.
- Ritchie DS (2008) Is allogeneic stem cell transplantation for transformed follicular lymphoma anti-lymphoma stem cell therapy? Leuk Lymphoma 49(10): 1852-1853.
- Varghese AM, Sayala H, Evans PA, O’Connor SJM, Russell P, et al. (2008) Development of EBV-associated diffuse large B-cell lymphoma in waldenstrom macroglobulinemia and mantle cell lymphoma. Leuk Lymphoma 49(8): 1618-1619.
- Jones D, Dorfman DM (2001) Phenotypic characterization of subsets of T cell lymphoma: Towards a functional classification of T cell lymphoma. Leuk Lymphoma 40(5-6): 449-459.
- Bolwell B, Kalaycio M, Andresen S, Goormastic M, McBee M, et al. (2000) Autologous peripheral blood progenitor cell transplantation for transformed diffuse large-cell lymphoma. Clin Lymphoma 1(3): 226-231.
- Dighiero G, Borche L (1991) B cell malignancies frequently target the autoreactive B cell repertoire. Leuk Lymphoma 5 Suppl 1: 47-51.
- Song MK, Chung JS, Yhim HY, Sung NL, Seong JK, et al. (2017) Tumor necrosis and complete resection has significant impacts on survival in patients with limited-stage upper aerodigestive tract NK/T cell lymphoma. Oncotarget 8(45): 79337-79346.
- Mori N, Yamashita Y, Tsuzuki T, Nakayama A, Nakazawa M, et al. (2000) Lymphomatous features of aggressive NK cell leukaemia/lymphoma with massive necrosis, haemophagocytosis and EB virus infection. Histopathology 37(4): 363-371.
© 2023 Mincai Li. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






