- Submissions

Full Text
Research & Investigations in Sports Medicine
A Case Study of Post-Operative Rehabilitation from Arthroscopic Hip Surgery for Femoroacetabular Impingement (FAI) and Labral Tear
Muran AC1*, LaCasse MR2, Treubig DW3 and Coleman S4
1Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, USA
2Pro Sports Physical Therapy, USA
3Evolve Physical Therapy & Sports Rehabilitation, USA
4Hospital for Special Surgery, Weill-Cornell College of Medicine, USA
*Corresponding author:Andrew C Muran, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, New York, USA
Submission: November 14, 2022;Published: January 09, 2023

ISSN: 2577-1914 Volume9 Issue2
Abstract
Femoroacetabular Impingement (FAI) is a clinical syndrome of hip pain and restricted mobility that is becoming an increasingly commonly diagnosed orthopedic condition. FAI is thought to be caused by morphological abnormalities of the femoral head, acetabulum or both and it is believed to be associated with hip labral tears and premature osteoarthritis. There is a need for reports that include detailed post-operative rehabilitation protocols, which could benefit physicians, physical therapists, and patients who are searching for specific plans to guide their recovery. In this report we attempted to present a FAI case in a Division I college athlete from the beginning of symptom onset, to eventual labral tear and surgery, and then through six months post-operative rehabilitation with a successful outcome (spanning 5 years). The novelty of this report lies in its combining of a surgical case study with a detailed rehabilitation protocol that stresses the importance of early and frequent mobilization of the postoperative FAI hip.
Keywords:FAI; Case study; Orthopedics; Arthroscopy; Rehabilitation
Introduction
Femoroacetabular Impingement (FAI) is a clinical syndrome of hip pain and limited motion that has been attributed to morphological abnormalities of the femoral head, acetabulum, or both. FAI has been identified as a cause of pain and labral tears, as well as juxtalabral cartilage damage and premature osteoarthritis [1-3]. Over the past 20 years, there has been a significant increase in arthroscopic hip surgery for the treatment of FAI and labral tears -with one recent estimate at 16.7 per 100,000 among privately insured patients between the ages of 18 and 64 [4-6]. Despite the prevalence of this procedure, the literature on postoperative rehabilitation and physical therapy has been limited. In this case study, we present the details of a particular intervention from initial presentation to surgical procedure and then postoperative recovery with a step-wise description of the physical therapy protocol. To the knowledge of the authors, there has not been a published evidence-based postoperative protocol for rehabilitation following FAI surgery
Case History
A 24-year old male provided informed consent for the publication of his case history. He originally presented with significant pain in the anterolateral left hip in February 2021. He had previously reported pain in that area in April 2016. He competed at the varsity level in squash for four years at a US Division I university and for an additional postbaccalaureate year at a UK university. During this period, he trained and played 20-25 hours per week at the US university and 10-15 hours per week at the UK university. Before this period, he competed in multiple sports through his primary and secondary scholastic years.
Initial presentation 2016
On Apr 1, 2016, the patient at 19 years old presented with consistent aching pain in the anterolateral left hip of six months duration. The patient described the pain as a consistent ache near the pocket region that was sharp when the patient moved from sitting to standing, during athletic competition, and whenever his hip joint went into deep internal rotation. X-Ray and MRI studies were ordered to visualize the bony structures of the hip joint and to look for a possible labral tear.
X-Ray (4/1/16): Findings: The joint spaces of the hips were maintained bilaterally. There was no fracture or dislocation. There was a lack of normal offset of the left femoral head-neck junction with a dysplastic bump involving the femoral head. Impression: Intact joint spaces without evidence of fracture. Lack of normal offset of the left femoral head-neck junction with dysplastic bump of the femoral head (Figures 1&2).
Figure 1:

Figure 2:

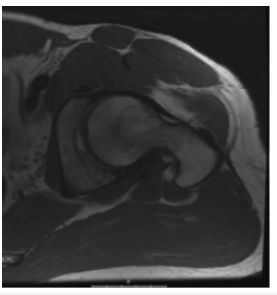
MRI (4/1/16): Findings: Evaluation of the left hip revealed the joint space to be maintained. There was no evidence of cartilage defect. The labrum was normal in signal intensity and morphology without evidence of tear. There was a cam lesion at the anterior aspect of the femoral head-neck junction with loss of normal offset. The alpha angle was 77 degrees at one o’clock. The left femur was anteverted, measuring 20+ degrees. There was no evidence of stress fracture or avascular necrosis. There was no significant joint effusion (Figures 3-6).
Figure 3:Sagittal.
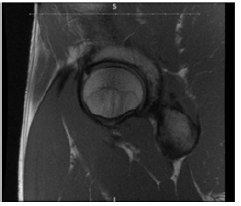
Figure 4:Axial.
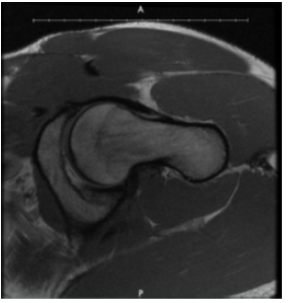
Figure 5:Coronal.
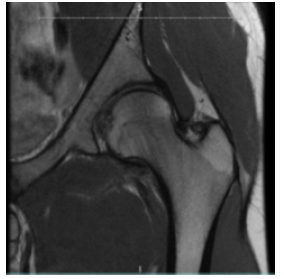
Figure 6:

Impression:Cam lesion at the anterior superior aspect of the left femoral head-neck junction (Figure 7-10).
Figure 7:

Figure 8:

Figure 9:
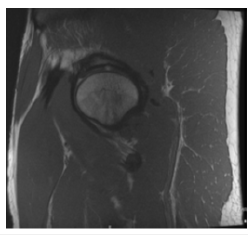
Figure 10:
Disposition (4/2/16):After receiving the diagnosis of Femoroacetabular Impingement (FAI) with no soft tissue damage, the patient was given the go ahead to continue training. With physical therapy (predominantly focused on glute and core strengthening, along with daily foam rolling and stretching exercises) the patient managed to keep the discomfort at bay for five more years of training and competition. The patient reported that if he was consistent with stretching and rolling after training or competition, the pain would be virtually nonexistent; however, if he didn’t maintain the routine, the aching pain in the left anterolateral hip would return. From spring 2016 to winter 2021, the patient managed to play without pain, all the while keeping up with the rolling and stretching routine tailored to manage any discomfort in his left hip.
Second presentation 2021:On February 11, 2021, the patient presented for a second time (almost five years later) and reported that while playing a squash match two months prior, something began to feel like it was “out of place” in the anterior region of the left hip near the psoas muscle. That feeling started after one point within the match, and although it was uncomfortable, the patient didn’t describe the sensation as sharply painful, until after 2-3 weeks of continued play and training when the discomfort in the hip developed into sharper, more consistent pain. The patient reported feeling a debilitating seizing of the hip joint that would produce a sharp stabbing pain deep in the anterolateral hip region, making it difficult to walk for hours after a match. Three weeks after the initial injury, the patient began going to Physical Therapy (PT) and worked for five weeks without any alleviation of pain. On February 24, 2021, two and a half months after the injury, the patient returned for a follow up visit and review results of imaging ordered.
Physical exam findings (2/11/2021):Left hip exam showed limited internal rotation at 90 degrees of flexion. The patient presented with some soreness particularly with external rotation, which was limited, some pinching with straight flexion, and five out of five strength in all planes and no lateral tenderness. It was recommended that the patient should continue with PT and have an X-Ray plus an MRI to rule out a labral tear and re-assess the character of the hip joint.
Physical exam findings (2/24/2021):During the February 24 follow-up visit, radiological studies were reviewed (see results below) and another physical exam was performed. The patient presented with pain with straight flexion, limited internal rotation and external rotation, as well as pain with flexion, internal rotation, and abduction. The patient also reported some discomfort with external rotation although he described it as more of a “stretch”. There was evidence of some lateral tenderness, some psoas tenderness, but no evidence of athletic pubalgia on exam.
X-Ray (2/17/21):Define difference in x-ray procedure
AP pelvis, elongated frog-leg lateral left hip and false profile view
Findings:Hips are located. Negative for fracture. There is lateral undercoverage of the femoral heads. There is bony prominence of the left femoral head-neck junction with fibrocystic change. SI joints are unremarkable.
Impression:Features of cam-type FAI with mild lateral undercoverage of the femoral head (Figures 6-9).
MRI (2/17/21): Findings:No acute fracture or osteonecrosis. Dedicated images of the left hip demonstrate bony prominence at the anterosuperior femoral head-neck junction. The anterosuperior labrum is diminutive and frayed between 2:00 and 3:00 with ossification at its base. Discrete tears of the anterosuperior labrum between 2:00 and 11:00 are noted along its articular surface. There is no detachment. Punctate paralabral cysts are noted on. The femoral head cartilage is maintained. There is a focus of exposed bone along the acetabular rim and 12:00. There is lateral under coverage of the femoral head with degenerative thickening of the ligamentum teres, flattening at the medial aspect of the femoral head and formation of tiny parafoveal osteophytes. There is no synovitis or intra-articular body. The iliofemoral ligament is preserved. The short external rotator, hip abductor, rectus femoris and iliopsoas tendons are intact. There is no greater trochanteric or ischial bursitis. Minimal bilateral hamstring tendinosis is present. The adductor tendon origins are maintained. There is no ischial bursitis. The lower lumbar intervertebral disc signal is maintained. The sacroiliac joints and pubic symphysis are preserved. Muscle bulk is symmetric throughout the pelvis and proximal lower extremities. There is no regional lymphadenopathy. The visualized pelvic organs are unremarkable. Fat planes surrounding the sciatic nerves are preserved. Version analysis, corrected for the degree of distal femoral rotation, demonstrates 19.3 degrees of right femoral anteversion and 26.9 degrees of left femoral anteversion (Figures 10-12).
Figure 11:
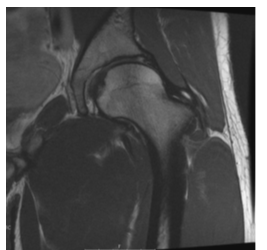
Figure 12:
Impression:MRI of the left hip demonstrates cam configuration of the femoral head-neck junction and acetabular undercoverage of the femoral head. The acetabular labrum is torn between 3:00 and 11:00 with punctate paralabral cyst formation anterosuperiorly. There is a small focus of exposed bone along the lateral acetabular rim. The hip joint cartilage is otherwise maintained, without synovitis.
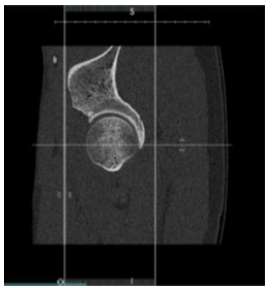
CT (2/17/21): Findings:There is no acute fracture or osteonecrosis. A large bony prominence is noted at the femoral head-neck junction between 2:30 and 12:30. Anterior and lateral acetabular coverage of the femoral head is diminished. Mild flattening of the parafoveal femoral head is noted. There is a focus of lateral acetabular subchondral plate remodeling at the site of a focus of exposed bone seen on MRI. The hip joint space is maintained. The subspine region is normal. 3D volume rendered images provide more accurate depiction of the osseous relationship of the proximal femur to the acetabulum. Findings of the left hip are as follows: Alpha angle at (2:00)=65 degrees; Coronal center edge angle=22 degrees; Tonnis angle=12 degrees; Femoral neckshaft angle=131 degrees; Acetabular version (1:00)=12 degrees anteverted; Acetabular version (2:00)=23 degrees anteverted; Acetabular version (3:00)=24 degrees anteverted; Sagittal center edge angle 50%=38 degrees; Femoral version corrected for rotation demonstrated 17.6 degrees of right femoral anteversion and 24.4 degrees of left femoral anteversion (Figures 13-16).
Figure 13:
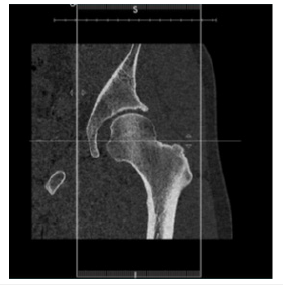
Figure 14:
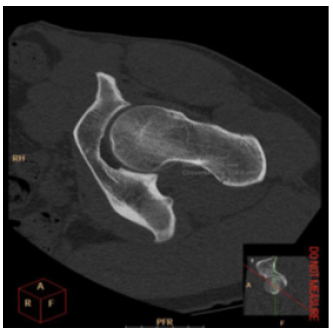
Figure 15:Post-processing CT showing CAM lesion.
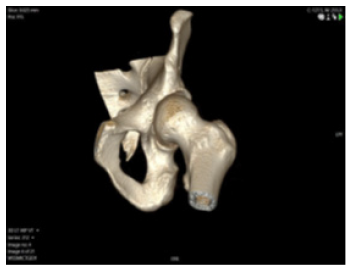
Figure 16:Pre-osteoplasty X-ray.
Impression:CT of the left hip demonstrates mixed features of cam-type femoroacetabular impingement and acetabular dysplasia. There is mild remodeling of the acetabular subchondral plate, without joint space narrowing.
Conclusion:Radiological scans (MRI and CT) of the left hip indicated FAI with a labral tear and the possibility of borderline dysplasia to dysplasia.
Further Consultation and Treatment Disposition
Due to the concern for dysplasia, the patient was referred for a consultation, and it was determined on Mar 22, 2021, that the dysplasia was not significant enough for periacetabular osteotomy to be indicated. In light of the severe labral tear, CAM lesion, and the lack of injury to the articular cartilage, the patient was considered an excellent candidate for hip arthroscopy, debridement of CAM lesion, hip osteochondroplasty, and labral repair. The patient was scheduled for surgery on 4/2/2021, and he continued physical therapy and playing squash (albeit with a modified movement technique to compensate for his injured left hip) up until the surgery.
Procedure for left hip arthroscopy (4/2/21)
On April 2, 2021, the patient underwent arthroscopic left hip surgery for Femoroacetabular Impingement (FAI), specifically, labral tear selective debridement with re-fixation x three anchors, acetabular rim decompression, synovectomy, femoroplasty and capsule repair. The patient was informed and prepared according to customary protocol. Anesthesia was administered without complication. A timeout was performed and the left leg was identified as the surgical site. The left leg was then prepped and draped in the routine fashion. The hip was placed in traction for a total of 33 minutes.
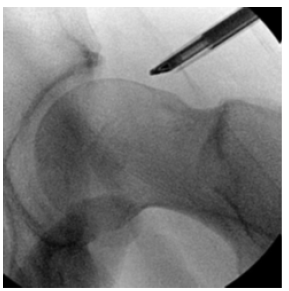
An anterolateral portal was established under fluoroscopic guidance. Under arthroscopic visualization, an anterior portal cut was performed. Using samurai blade, a capsular cut was made. Diagnostic arthroscopy revealed intact articular surfaces of the femoral head. The acetabulum was visualized and the chondral surfaces intact. The ligamentum teres was intact. The labrum was torn from 12 to 2 o’clock. Using stryker sling shot, orthocord traction suture was placed in the capsule. A shaver and Arthrocare was used to remove the soft tissue from the sub spine area. A sharp pincer lesion was identified from 12 to 2 o’clock and then was taken down using a bur as well as removing a small portion of the rim. Having done so, the remaining cartilage was entirely stable. Labral repair was then performed using 3 anchors to repair the labrum from 12 to 2 o’clock and excellent repair was achieved with good tension. At this point, the traction was released and the peripheral compartment was entered and visualized. A CAM lesion was identified. The CAM lesion was decompressed with a 5.5 bur under fluoroscopic guidance. Using a 4.5 shaver a synovectomy was performed. With the Stryker Sling shot using 3 Orthocord, capsular closure was performed. Time length for procedure: Seventy minutes
At the end of the procedure, all arthroscopic instruments were removed and the hip was thoroughly irrigated. The portals were closed with interrupted Nylon sutures and a sterile dressing was applied. The patient was transferred to the recovery room in stable condition. Patient required the use of a hip brace post-surgery in order to provide core support and prevent the hip joint from external rotation.
Intraoperative Pre and Post Osteoplasty
Pre-osteoplasty X-ray
Three hours post op, the patient woke up feeling alert and lucid and in minimal pain. He was advised by hospital staff that due to the effects of the epidural, he would not be able to move his legs for approximately one hour. After about two hours, the patient was able to stand and walk with crutches to a wheelchair. He was then discharged. He used minimal medication (Vicodin) for pain management (Figures 17-19).
Figure 17:Post-osteoplasty X-ray.
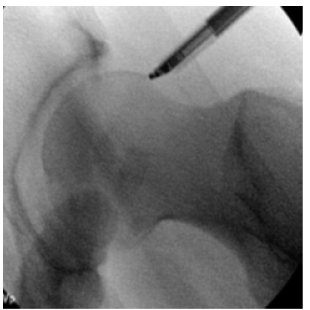
Figure 18:Shaved down CAM lesion.
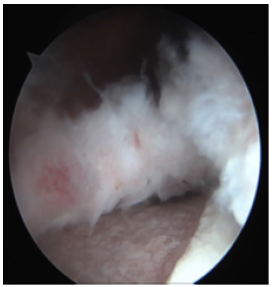
Figure 19:Labral repair.

Post-operative rehabilitation protocol
Week 1:Days 1-3. The patient reported that the first three days post op were particularly difficult, but there was a marked decrease in discomfort after Day 3. Patient attempted to sleep on his back or on the non-operative side. Patient tried not to move the operative leg too much for the first few days so as to let the inflammation settle. However, the patient did attempt to get up to get water, go to the bathroom, and to just move around the house every hour or so. At this point, the patient always used crutches when moving. Throughout these first three days, the patient applied a large ice pack to the hip flexor region roughly seven times a day. The patient found the icing very useful in alleviating pain, but after the first week the ice packs seemed to have less of an effect (and maybe even made the anterolateral hip region feel tighter). So, after a week of consistent icing, the patient discontinued icing.
Day 1. (The patient tried to minimize the amount of time spent in a seated position, so as to let the hip flexors heal without contraction or tightening up.) While lying supine, the patient would isometrically contract his glutes (glute squeezes) roughly three times per day in sets of 10 with a two-second hold per contraction. The patient would also perform three sets of 10 calf pumps while supine per day as well. Both exercises were performed to minimize atrophy in the glutes and calf muscles, however, the patient was careful not to overdo the glute contraction (by performing them too frequently), so as to avoid aggravating the swollen and inflamed hip flexor region (upon contraction of the posterior chain the patient would feel an ache in the hip flexor). The patient would also try to squeeze his glutes while standing to gauge pain levels, as it was a sure way to be able to feel how “angry” the front side of the hip joint was at the moment. He tried to not overdo this action, so as to not aggravate the hip flexor and to avoid developing hip flexor tendonitis. He continued these exercises for the first month post operation.
Day 2. The patient gently rode on a stationary bike for 10 minutes and reported that it was surprisingly tolerable. Also on Day 2, the patient began performing gentle, supine hip range of motion exercises, including. internal and external rotation of the leg and foot whilst lying supine. The patient also began roughly 30 minutes of prone lying per day, to stretch the hip flexors. The patient continued biking, performing the supine range of motion exercises, and prone lying for the first month post operation. Day 3. The patient felt that the pain subsided significantly on Day 3. He reported that the glute contractions were still painful until approximately Day 7 (and that it would still cause him to feel a small ache in the hip flexor regions on occasion even weeks later), but the patient felt that it was beneficial to do the glute contractions periodically throughout the day just to keep the glutes engaged. The patient also felt that in hindsight, he could have begun the gentle supine range of motion exercises the first or second day post op as opposed to the third (especially considering some patients actually see their physical therapist the first day post op). Another exercise the patient would have added in hindsight, would be having a caretaker pick up the injured leg with one hand holding the ankle and the other holding the knee, and just run the leg through gentle passive range of motion exercises (small circles, side to side, and passive flexion for two sets of 10 reps each once or twice a day).
Day 4. On Day 4, the patient began physical therapy as per his surgeon’s direction. During the first session the physical therapist was relatively conservative. The patient was still walking on both crutches. He warmed up with a 10-minutes ride on a stationary bike. The physical therapist performed some gentle range of motion joint mobilization and some deep tissue massage in the lower abdomen. The therapist also performed hip internal and external rotation with mobilization and movement.
Day 5. On Day 6, the patient continued to feel that the pain was subsiding. He continued doing the exercises outlined on Days 1 and 2. Day 6. After discussing with his surgeon, the patient began doing overhead press and bicep curls with a 20lb dumbbell in a lounge chair (semi-supine position). He was advised that he could perform these limited upper body exercises while seated. The patient reported that he started to walk around without crutches on Day 6 (only for short walks around the house). He reported it probably would have been better to wait until Day 9 to walk without crutches since he felt a slight but noticeable increase in pain the following day (though it subsided the day after). The therapist advised to follow the principle of “listening to your body as a guide for what you’re ready for” -in other words, wait to see how you feel the day after an exercise and adjust accordingly. The patient also reported attempting to sit down for an extended period of time for the firsttime post op and found it difficult to sit with 90-degree hip flexion.
Days 7. Patient reported that after weaning off the crutches in the house, he started experiencing some twinges in the left hip flexor, which were similar in location and quality to the original injury. Until this point, the progress had been steady and surprisingly rapid.
Week 2: Day 8-10. The patient continued doing the exercises outlined above in Week 1. Day 10 (2nd PT session). On Day 10, the patient had his second physical therapy session and moved on to walking with one crutch as per the physical therapist’s recommendation. The patient reported that the physical therapist was surprisingly aggressive (though still seen as positive), as they started building up an at home rehab routine. Session 2 included biking to warm up, quadruped rocking in pain-free range (20reps), standing side gliding against a wall (10 times loading the left side for two sets - the purpose of this exercise being to load the left hip and get it used to accepting load as opposed to sensing load as a threat), soft tissue work (the therapist began to massage the hip flexor region), a rectus femoris stretch (patient was supine on the table with hanging off), and halfkneeling hip flexor stretch, which the patient reported was slightly painful. However, the therapist compared the pain to a yellow light - if a rep hurts, ease out of the position, try again, and if the pain isn’t consistent, then finish the reps (if the pain continues then stop). In other words, don’t necessarily be alarmed and stop whatever you’re doing if you feel one twinge.
The patient reported feeling significantly better after this
second PT session on Day 10 post op, and was surprised at the
intensity of the stretching. Also on Day 11 (at the end of the PT
session), the patient began re-introducing pull ups (using a stool to
get up and down with his non-injured leg) and reported no issues.
The patient reports that he likely could have started doing pull
ups even earlier (maybe on days 7,8,9). Note: The patient reported
that he has always had very tight hip flexors, and that the therapist
could see this just from stretching the non-injured right hip flexor.
This tightness informed the PT emphasis on stretches that would
improve tissue extensibility/pliability (or improve tissue stretch
tolerance) the iliopsoas (hip flexor) so as to prevent contraction of
that already naturally tight muscle in this patient. On Day 10, the
patient began going through a protocol at home that included the
following exercises:
A. Stationary bike for 10 minutes
B. Quadruped rocking (mobilization)
i. Patient began this exercise on Day 10 and incorporated it into his daily mobilization/stretching routine (to start the routine). The patient would perform it for 20 reps 2-3 times per day until roughly Month 5 (when he had less time to devote to rehab and began performing the exercise 1 time per day).
C. Quadruped hip circles (mobilization)
Patient began this mobilization exercise on Day 10 and
incorporated it into his daily mobilization/stretching routine. The
patient would perform it for 20 reps 2-3 times per day until roughly
Month 5 (when he began performing the exercise 1 time per day).
D. Quadruped active hip external/internal rotations
Patient began this mobilization exercise on Day 10 and
incorporated it into his daily mobilization/stretching routine
(to start the routine). The patient would do 10 sweeps in each
direction reps 2-3 times per day until roughly Month 5 (when he
began performing the exercise 1 time per day).
E. Half kneeling hip flexor stretch (stretch)
Patient began this stretch on Day 10 and incorporated it into
his daily mobilization/stretching routine (to start the routine).
The patient would hold the stretch for a minute on each leg 2-3
times per day until roughly Month 5 (when he began performing
the exercise 1 time per day). In addition to holding the stretch, the
patient would perform three trunk rotations in each direction while
in the half kneeling hip flexor stretch position.
At roughly the four-month mark the patient would finish the stretch on each side by adding an extra 20 second of deeper hip flex stretching by going into an extended/deep lunge with elbows on the ground. Day 11. On Day 11, the patient had his first post op visit with the surgeon. His sutures were removed. The surgeon was pleased with the patient’s progress but recommended that the patient not leave the one crutch behind altogether (yet) until the patient was walking with a normal gait. During short walks at home, the patient worked on normalizing his gait and used the one crutch for longer walks or whenever the patient felt like the hip was sore/tired. The patient reported that his hip no longer hurt, except for an occasional twinge in the hip flexor, and that his gait was normalizing.
Day 12 (3rd PT session). The patient reported feeling very sore on Day 12 due to some extended walking the day before. The patient also reported that despite a slightly altered gait, he felt comfortable walking without crutches. The physical therapist thought that the patient’s gait was good enough for him to begin mostly walking without a crutch. PT began with the bike, longer exhale than inhale breathing exercises (hooklying diaphragmatic breathing - to decrease tone in the hip/pelvic musculature), supine pelvic tilts, and glute bridges. As per the patient’s request, they experimented with push-ups and as they didn’t cause any pain, the therapist gave the patient the ok to do push-ups on his own. Next the therapist placed a BFR band around the patient’s left quad, as well as an ankle weight on the left ankle.
The patient then proceeded to perform four sets of 30 BFR/ ankle weighted quad raises with the lower leg hanging off the edge of the table. The patient then did three sets of maximum rep pushups and pull ups after the PT session. Later that day, the patient felt that his quadriceps muscles were tired from their first intensive exercises post op (with the BFR bands) and that the hip flexor was hurting more than usual (likely also due to the quad exercises). However, the patient did a mobilization session in the afternoon, which included: quadruped rocking, quadruped hip circles, quadruped active hip external/internal rotations, standing side gliding against a wall, and half kneeling hip flexor stretch and felt a significant alleviation of pain
Days 13-14. The patient reported performing his mobilization routine 2-3 times per day every day as well as 4 sets of pull ups and push-ups 1 time per day. The patient added a quadruped single leg adductor stretch. The leg mobilization routine (quadruped rocking, hip circles, quadruped active hip external/internal rotations, standing side gliding against a wall, half kneeling hip flexor stretch, and quadruped single leg-adductor stretch) provided the patient with significant pain alleviation. During this interval the patient also began walking in a pool. The pool routine, which the patient did roughly two times per week included walking 20 yards forward, then walking backwards 20 yards four times, walking laterally 20 yards two times in either direction (four lateral walks in total). The patient reported that the pool walking helped him feel more stable when attempting to walk outside of the pool. The patient performed these exercises in the pool roughly two times per week from week 2 through the first three months post op.
Week 3: Day 15-16 . The patient continued doing the exercises outlined above. Day 16 (4th PT session). At this point the patient reported walking almost entirely without a crutch and that his pain was continuously lessening. However, the patient still reported an altered gait, which he was concerned had plateaued progress wise (he was particularly concerned that he stopped with the crutches too early). The patient visited a second physical therapist, who was particularly focused on working on the patient’s altered gate. He confirmed that crutches were no longer necessary in the house, but recommended that the patient might want to use them in a grocery store for example, where the patient might have to pivot spontaneously. The therapist recommended that the patient begin performing mini squats (not a full range of motion squat) in the pool in addition to the forward, backward, and side walking that he was doing two times a week.
So at Day 16 the patient also introduced the following to his pool sessions: mini squats (limited range of motion squats where the patient didn’t go into full hip flexion), balancing on one-leg, lunges, split squat (static lunge), and Bulgarian squats with his back leg pushing against a wall of the pool. He continued doing these exercises in the pool along with the original set of pool exercises two times per week from Day 16 through the third month postoperation. The therapist also emphasized performing hip flexor stretching, especially because the patient had notably tight hip flexors prior to the surgery. Note: Even after two weeks post op, the patient rarely attempted to sit down in a position where his hips flexed 90 degrees. Days 17-21. The patient continued doing the exercises outlined above.
Weeks 4-24 (Months 1-6): Days 19-70. During this period, the patient found that walking without crutches during this period helped to accelerate the normalization of the gait. By Day 70 (at the two months and 10 day post op mark), he reported his gait was normal. The following will include a summary of the exercises and mobilization routine that the patient performed during this interval. At around three weeks post op, the patient began to use the foam roller to massage the hip flexors and glutes. The patient reported that rolling on the surgical site itself was painful at first, but that it greatly helped to reduce pain and tightness in the iliopsoas and that the pain from rolling lessened each time he rolled. From three weeks post operative, the patient performed the mobilization routine 2-3 times per day and would roll 1 time per day (typically in the afternoon) before starting the second or third mobilization routine. If the patient had physical therapy or performed a more re-strengthening focused routine, then he would finish that routine with rolling and stretching (the mobilization routine=stretching).
The patient reported that he started performing the same upper body lifts that he did before the surgery at around 30 days (one month) post op. He returned to his sport at three months with solo drills (hitting with minimal movement). At roughly three and a half months, the patient began to slowly reintroduce sport specific movement drills to his routine. Around five months (20 weeks) after the surgery, the patient’s occupational circumstances changed, which made it significantly more difficult for the patient to perform the mobilization routine 2-3 times per day. After about a month of only stretching one time per day at night (six months post op mark), he began to feel some stiffness in the left hip flexor. To work on that tightness the patient created a morning routine and performed a modified, shorter stretching/strengthening routine, which includes a 1.5-minute plank, two sets of 12 SL glute bridges, and half kneeling hip flexor stretch for one minute per leg. The patient continues to do this routine in the morning and usually rolls and stretches at night after exercising.
The patient added the following hip exercises to his protocol
1. Plank (strengthening)
The patient performed a 1.5-minute plank essentially every day
from Month 2 Month 6 Thereafter he.
Around month 6 the patient incorporated it into his morning
routine, and he also found it useful as a full body warm-up
before any training session.
2. Single-leg glute bridge (Strengthening)
The patient began single-leg glute bridging 13 days post
operation and continued using the exercise, sometimes
within the mobilization routine and often within his rehab/
strengthening sessions (typically 2 sets of 12).
At around the six-month mark the patient incorporated the SL
glute bridge into his morning routine.
At first it was painful for the patient to keep the left leg straight
during the SL glute bridge, so the patient modified the exercise
by keeping the injured leg bent at the knee, while the noninjured
leg is doing the work of the bridge.
This exercise can also be made easier by doing a normal glute
bridge
3. Modified side plank with hip abduction (strengthening)
The patient performed this exercise in physical therapy starting
in week 3 up until month 2 when he progressed to normal side
planking with a side leg raise.
4. Side plank with hip abduction (strengthening)
This patient performed this exercise roughly 1-2 times per
week (one set of 10reps per side) beginning at the two-month
postoperative mark and continues to perform the exercise as
a part of his rehab/strengthening sessions. The patient would
spend roughly a minute in a side plank and would slowly raise
the free leg laterally upwards.
The patient would do this during a physical therapy session or
during a solo rehab/strengthening session.
5. Normal side plank (strengthening)
The patient also did side planks without the leg raises 1-2 times
per week from Month 2 to Month 6.
6. Lunges (strengthening)
At roughly the 2.5 month mark the patient began lunging in
physical therapy with either no weight for three sets of 10
lunges per leg or with a 20lbs kettlebell for two sets of 10 lunges
per leg. The patient performed this exercise 1-2 times per week
either at physical therapy or during a rehab/strengthening
session on his own.
The patient has progressively added more weight to the lunges
and continues to perform this exercise during his rehab/
strengthening sessions.
7. Physioball table-top holds (strengthening)
At the 1.5 month mark the patient would perform a physioball
table-top hold with a 20lbs plate on his abdomen for two
minutes.
The patient did this during physical therapy from roughly
Month 1.5 through to the present once per week.
8. Leg to the back and side on a slider and bring it back two
times 10reps (mobilization)
The patient began performing this exercise at the 1.5-month
mark roughly once per week during physical therapy sessions
and continued doing it in physical therapy.
9. Band resisted lateral walk 2 times 10reps
The patient began performing this exercise at around the
1.5-month mark and would perform it 1 time per week during
physical therapy sessions until the five-month mark when he
stopped regularly going to physical therapy.
The patient had a large rubber band strapped around his waist and side walked away from the band’s attachment point against tension
The patient would then slowly side-walk backwards fighting the pull back towards the band’s attachment
The patient took 10 sideways strides per set and performed two sets per leg
10. Band resisted forward/backward walk
The patient began performing this exercise at around the
1.5-month mark aand performed it 1 time per week during
physical therapy sessions until the five month mark when he
stopped regularly going to physical therapy.
The patient had a large rubber band strapped around his waist and would walk away from the band’s attachment point against resistance.
The patient then slowly walked backwards fighting the pull back towards the band’s attachment.
The patient would take 10 strides per set and would perform two sets.
11. Iron cross side to side switching (mobilization/stretch)
Before the patient could hold an iron cross stretch (as it was
painful to hold the position) the patient would perform the iron
cross stretch but would switch the stretch from side to side
after holding the stretch on each side for roughly 5-10 seconds.
The patient began this stretch around 1.5 months post op and around the second month progressed this mobilization/ stretching exercises to a static iron cross holding stretch (which he holds for one minute on each side and performs once per day as a part of his fully progressed mobilization/stretching routine (which is included at the end of this section).
12. Modified Turkish get ups at home two times 10reps
The patient began performing this exercise once per week at
physical therapy and occasionally on his own during rehab/
strengthening sessions starting at the 1.5 month post operative
mark.
13. Inchworms (two sets of 10 reps)
The patient began performing this exercise at around the
1.5-month mark and would perform it 1 time per week during
physical therapy sessions until the five-month mark when he
stopped regularly going to physical therapy.
14. Physioball bridges with eccentric hamstring curl (two
sets of 10 reps)
The patient began performing this exercise at around the
1.5-month mark and would perform it 1 time per week during
physical therapy sessions until the five-month mark when he
stopped regularly going to physical therapy
15. SL RDL
The patient began performing single leg RDL’s at around the
three-month mark and continues to use this exercise in his
strengthening sessions (once per week).
16. Split lunges with jump
The patient began performing split lunges without weights at
around the five-month mark and continues to use this exercise
in his strengthening sessions (one time per week).
He has progressed to performing these explosive jumping split lunges with 25lbs dumbbells in each hand.
17. Deadlift
The patient began deadlifting with a kettlebell or a barbell at
the two-month postoperative mark.
He would perform the exercise at physical therapy sessions and now performs hex bar deadlifts roughly one time per week as a part of his strengthening sessions.
18. Thrusters with dumbbells and a jump
The patient began performing squats with 25 lbs dumbbells
followed by an overhead press and jump off the ground to
retrain explosivity at roughly the five month postoperative
mark.
At roughly the three month (12 week) mark and through the present, the patient progressed to performing the following mobilization routine one time per day, ideally immediately after exercising, but if the patient didn’t train, then he would still perform the routine.
19. Quadruped rocking for 20reps
20. Quadruped hip circles 10 circles per direction
21. Quadruped active hip external/internal rotations five
times in each direction (internal/external rotation) per leg
22. Frog stretch for 1-2 minutes
23. Sitting toe touch (hamstring) stretch (one min hold)
24. Iron cross stretch for one minute per leg
25 Half kneeling hip flexor stretch for one minute per leg
(with three trunk rotations per side while holding the stretch)
26. Progress from half kneeling hip flexor stretch to a deeper
lunge stretch where the patient tries have his elbows touch the
floor (hold for 30 seconds per side)
27. Quadruped single-leg adductor stretch
The patient returned to solo hitting after three months (12 weeks) and ghosting after three and a half months (14 weeks). Finally, the patient began drilling with a hitting partner at roughly the 4.5 month mark, and began match play at roughly the fivemonth mark. The patient reports that he possessed full range of motion in the left hip and is able to play without pain again at this juncture. At roughly the 7 month mark the patient was back to his prelabrum tear level. However, he reported that as it was important to be diligent with his rolling, stretching and strengthening routines in college pre-labral tear but post FAI diagnosis, the same holds true post operation. To keep any soreness or discomfort at bay, the patient continues to roll on a foam roller and performs the above mobilization routine immediately after training. He also continues to perform the previously outlined morning routine daily.
Discussion and Conclusion
This case study represents a unique combination of a surgical
case study that follows a patient from initial presentation of mild
symptoms (pre-labral tear), through a five-year process of reassessment
and management to eventual surgery and successful
rehabilitation with a detailed rehabilitation protocol developed
by two physical therapists in conjunction with the surgeon and
patient. Though this patient’s case and surgery were typical for
FAI, the rehab protocol includes a uniquely comprehensive and
detailed description of mobilization routines and strengthening
exercises for post-hip arthroscopy rehabilitation with the aim of
returning an athlete to the highest level of their sport. The protocol
is extensive, and we attempted to provide accurate descriptions of
each exercise or stretch in the hopes that this might be of use to
either the athlete on their road to recovery, the surgeon in advising
the patient or therapist, or for the physical therapist in managing
the athlete’s rehabilitation. Though it is hard to identify, which
specific exercises, stretches or routine are most responsible for the
patient’s successful outcome, the two most salient points that can
be drawn from this case study with its emphasis on rehabilitation
are:
1. It is important to begin working on mobilization of the
post-operative hip joint soon after surgery;
2. Diligence and consistency in mobilization and
strengthening on the part of the patient are paramount.
Though this paper reports only a single-case study, it does fill the need for a report that longitudinally describes an otherwise typical FAI case in an elite athlete that includes a novel and detailed post-operative rehabilitation protocol.
References
- Bedi A, Kelly BT (2013) Femoroacetabular impingement. J Bone Joint Surg Am 95(1): 82-92.
- Dickenson E, Wall PDH, Robinson B, Fernandez M, Parsons H, et al. (2016) Prevalence of cam hip shape morphology: A Systematic review. Osteoarthritis Cartilage 24(6): 949-961.
- Ganz R, Leunig M, Ganz KL, Harris WH (2008) The etiology of osteoarthritis of the hip: An integrated mechanical concept. Clin Orthop Relat Res 466(2): 264-272.
- Maradit KH, Schilz SR, Houten HK, Herrin J, Koenig KM, et al. (2017) Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplast 32(3): 750-755.
- Mascarenhas VV, Rego P, Dantas P, Fátima M, Justin M, et al. (2016) Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: A systematic review. Eur J Radiol 85(1): 73-95.
- Neil VS, Maximilian S, John JK, Alexandr A, James PD, et al. (2018) Demographics and rates of surgical arthroscopy and postoperative rehabilitative preferences of arthroscopists from the Arthroscopy Association of North America (AANA). J Orthopaedics 15(2): 591-595.
© 2023 Muran AC. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






