- Submissions

Full Text
Research & Investigations in Sports Medicine
Perineural Hydrodissection as Novel Treatment for Entrapment of the Dorsal Cutaneous Branch of the Ulnar Nerve: 2 Case Reports
Brandon F. Boldt1, MD, Sarah B. Sturgill1, MD, and Yao-Wen Eliot Hu1,2*, MD, MBA, RMSK, FAAFP
1Department of Physical Medicine, Naval Hospital Camp Pendleton, USA
2Department of Family and Community Medicine, Uniformed Services University of the Health
*Corresponding author:Yao-Wen Eliot Hu, Department of Physical Medicine, Naval Hospital Camp Pendleton, USA; Department of Family and Community Medicine, Uniformed Services University of the Health Sciences, USA
Submission: September 12, 2022;Published: September 26, 2022

ISSN: 2577-1914 Volume9 Issue1
Abstract
The Dorsal Cutaneous Branch Of The Ulnar Nerve (DCBUN) is a pure sensory terminal branch supplying sensation to the dorsal ulnar hand. Extensive literature review revealed that although there are reports of DCBUN neuropathy and injury, the incidence and prevalence is rare. Presented are two cases of spontaneous overuse entrapment of the DCBUN with paresthesia in its corresponding distribution, confirmed via ultrasound showing enlargement and flattening of the nerve. Perineural hydrodissection provided complete symptomatic resolution in these cases, offering a potential novel treatment. Increased clinical suspicion and accurate diagnosis for DCBUN neuropathy is pivotal for effective management, especially when traditional treatment fails.
Keywords: Dorsal cutaneous branch of ulnar nerve; Ultrasound; Hydrodissection; Entrapment; Case report
Abbreviations: DCBUN: Dorsal Cutaneous Branch of the Ulnar Nerve; FCU: Flexor Carpi Ulnaris; ECU: Extensor Carpi Ulnaris; ROM: Range of Motion; OT: Occupational Therapy; MRI: Magnetic Resonance Imaging
Introduction
The Dorsal Cutaneous Branch of the Ulnar Nerve (DCBUN) is one of the pure sensory terminal branches innervating the dorsal aspect of the ulnar hand, fifth finger, and ulnar half of the fourth finger [1]. The nerve originates in the distal forearm approximately five centimeters proximal to the ulnar styloid and runs volar deep to the Flexor Carpi Ulnaris (FCU) tendon [2,3]. The DCBUN then pierces the Extensor Carpi Ulnaris (ECU) muscle dorsally approximately 1.5 centimeters proximal to the ulnar styloid and traverses subcutaneously to its terminal branches [3,4]. Although DCBUN neuropathy is considered rare, there is no epidemiologic data published in the current literature. Despite case reports listing potential causes including compressive accessories and handcuffs, distal ulna resection, traumatic laceration, proliferative wrist synovitis, and repetitive overuse, [5-7] the evidence for perineural hydrodissection as treatment is lacking. The following cases describe DCBUN entrapment neuropathy treated with perineural hydrodissection, offering a potential novel treatment.
Case Presentations
The first case is a 27-year-old, right-handed, military servicemember who presented with two years of atraumatic right dorsal, ulnar-sided distal forearm and wrist pain. The pain was sharp and provoked during computer mouse use and motorcycle riding. The patient reported associated numbness of the proximal dorsal ulnar hand with occasional wrist clicking. Physical examination revealed normal alignment, strength, and full Range of Motion (ROM) of the wrist and hand. He was tender to palpation over the right distal ulnar forearm dorsally proximal to the ECU Musculo-Tendinous junction. ECU and FCU resisted-activation tests both reproduced symptoms and Tinel’s sign over the DCBUN was positive. He had failed prior relative rest, cock-up wrist bracing, and a twelve-week course of Occupational Therapy (OT) focusing on the dorsal wrist tendons. Wrist radiographs were unremarkable.
The second case is a 22-year-old, right-handed, military servicemember who presented with ten months of right ulnarsided wrist pain and dorsal hand pain in the fourth webspace after he started practicing martial arts without specific injury. The patient endorsed general weakness to his grip strength in the whole hand especially notable while shaking hands while his active ROM in all planes of the wrist worsened symptoms. Physical examination showed subtle resting pronation of the right forearm with mild decreased strength in the flexor digitorum profundo’s, lumbricals, and interosseus muscles while sparing the flexor digitorum superficialis. Wrist and hand ROM was normal. ECU and FCU resisted-activation tests reproduced symptoms and Tinel’s sign was positive over the DCBUN. Wrist radiographs were unremarkable and Magnetic Resonance Imaging (MRI) revealed ECU tenosynovitis. A twelve-week course of OT focusing on intrinsic hand strengthening initially helped, but symptoms progressively worsened after initiating throwing exercises.
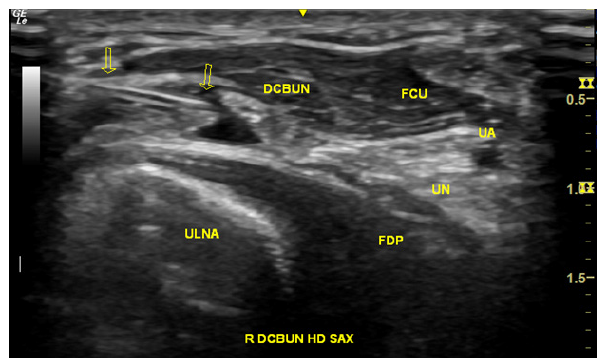
In both cases, dynamic musculoskeletal ultrasound with wrist extension and ulnar deviation illustrated flattening of the honeycomb appearance of the DCBUN in transverse axis, deep to the FCU muscle. Sono-palpation at this location also reproduced symptoms. Given their strong preference for participating in upcoming deployments, both patients underwent diagnostic and therapeutic ultrasound-guided fascial plane and perineural hydrodissection around the DCBUN deep to the FCU muscle (Figure 1). After injection of a ten-milliliter mixture consisting of 10 milligrams of 40mg/mL triamcinolone acetonide, 0.5 milliliters of 1% lidocaine, 0.5 milliliters of 0.5% ropivacaine, and 9 milliliters of 5% dextrose using a 23-gauge 1.5-inch needle, both patients experienced complete and continued symptom resolution at three and six months.
Figure 1:Ultrasound-guided fascial plane and perineural hydrodissection of the Dorsal Cutaneous Branch Of The Ulnar Nerve (DCBUN) in short-axis via an in-plane approach with the needle (arrows) deep to the Flexor Carpi Ulnaris (FCU) muscle. UA, ulnar artery; UN, ulnar nerve; FDP, flexor digitorum profundus.
Discussion
DCBUN neuropathy may be misdiagnosed due to vague symptoms, nonspecific examination findings, and overlap with common conditions. Accurate diagnosis is critical for appropriate treatment. Initial workup includes history, physical examination, and imaging including radiographs, computed tomography, or MRI to rule out other conditions such as fractures, tendinopathy, or space-occupying lesions. Preliminary evaluation may reveal paresthesia and decreased sensation along the dorsal ulnar hand involving the fourth and fifth digits while pain is often provoked with wrist flexion and extension while in ulnar deviation [2]. Given its pure sensory origin, there is intact strength and muscle tone with diminished sensation in DCBUN distribution compared to the contralateral side. Electromyography and nerve conduction studies may help localize the pathology and identify differences between extremities with high specificity and low sensitivity, but further research is needed [3].
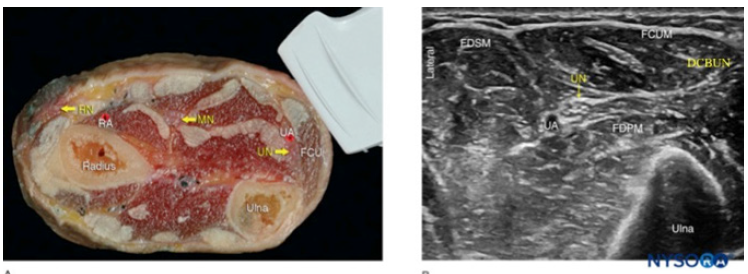
Cadaveric studies reveal variations between the origin, path, and branching but ultrasonography studies demonstrate reproducible identification of the DCBUN despite these differences [3,5,8]. Diagnostic scanning begins in the volar ulnar forearm approximately five centimeters proximal to the ulnar styloid with the transducer placed transverse to the ulnar nerve. The DCBUN is visualized medial to the ulnar nerve, deep to the FCU as the transducer is translated distally [9,10]. Dynamic wrist ulnar deviation, flexion, and extension at this location may reproduce symptoms and illustrate signs of entrapment including flattening and enlargement (Figure 2). DCBUN entrapment is also highly associated with ECU tenosynovitis, warranting careful evaluation of the ECU [9].
Figure 2:(A) Cross-sectional anatomy of the distal forearm. (B) Sonoanatomy of the ulnar nerve (UN) at the forearm. UA, ulnar artery; FCUM, Flexor carpi ulnaris. FDPM, flexor digitorum profundus muscle; FDSM, flexor digitorum superficialis muscle; DCBUN, dorsal cutaneous branch of the ulnar nerve.SOURCE:NYSORA.COM
Both conservative and surgical outcomes are rarely reported in the current literature. Conservative treatment includes rest, antiinflammatory medications, nerve glides, focused rehabilitation, and splinting while refractory cases are historically referred for surgical decompression. Low-level laser therapy has also been reported as adjunct treatment [9]. Given the limited evidence for current treatment options and the time-sensitive nature of upcoming deployments, diagnostic and therapeutic ultrasound-guided perineural hydrodissection of the DCBUN was performed for both patients after detailed discussion and shared decision-making. The intent of hydrodissection is for the hydrostatic pressure of the injectate to release tissue around the nerve. Specifically, the DCBUN is identified in the distal volar forearm with the transducer transverse to the nerve. After a Doppler time-out to ensure safe needle passage, the needle is introduced in-plane next to the DCBUN to place the injectate in the fascial plane deep to the FCU, taking extreme caution not to iatrogenic ally injure the nerve.
These are two cases of reported DCBUN entrapment neuropathy treated with perineural hydrodissection, offering a novel non-operative modality for this rare condition. DCBUN neuropathy may be misdiagnosed or overlooked but ultrasound is an operator-dependent yet readily available modality that aids diagnosis and treatment in the appropriate clinical context. Increased clinical suspicion for DCBUN neuropathy is pivotal for effective management, especially when traditional treatment fails.
Acknowledgments and Funding
The views expressed in this publication are those of the authors and do not reflect the official policy or position of the Department of the Navy, the Department of Defense, Uniformed Services University of Health Sciences, or the U.S. Government. The authors declare no conflicts of interest and do not have any financial disclosures.
The authors are military service members of the United States Government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that copyright protection under this title is not available for any work of the United States Government. Title 17 U.S.C. 101 defines a U.S. Government work as work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
Conflict of Interest Statement
Yao-Wen Eliot Hu: AMSSM- Received honorarium as scanning faculty at the Fundamentals of Ultrasound Pre-conference at the AMSSM Annual Meeting. Brandon Boldt: none. Sarah Sturgill: none.
Permissions
From NYSORA’s website: “NYSORA receives many permission requests to use NYSORA’s material. Since Education and Advancement of Practice of Anesthesiology are NYSORA’s primary missions, we grant you the permission to download and use NYSORA’s teaching material without asking for permission. However, you MUST acknowledge: “Source: NYSORA.COM” in all your slides and publications featuring any NYSORA’s material. Failure to visibly disclose the source constitutes a violation of copyrights laws & NYSORA’s intellectual property
References
- Sulaiman S, Soames R, Lamb C (2015) The sensory distribution in the dorsum of the hand: Anatomical study with clinical implications. Surg Radiol Anat 37(7): 779-785.
- Rotman D, Schermann H, Kadar A (2019) Displaced distal radius fracture presenting with neuropraxia of the Dorsal Cutaneous Branch Of The Ulnar Nerve (DCBUN). Arch Orthop Trauma Surg 139(7): 1021-1023.
- Jung HS, Lee YB, Lee JS (2016) The anatomical relationship between the dorsal cutaneous branch of the ulnar nerve and the ulnar styloid process with variations in forearm position. J Hand Surg Asian Pac 21(1): 64-67.
- Uerpairojkit C, Kittithamvongs P, Puthiwara D, Anantaworaskul N, Malungpaishorpe K, et al. (2019) Surgical anatomy of the dorsal cutaneous branch of the ulnar nerve and its clinical significance in surgery at the ulnar side of the wrist. J Hand Surg Eur 44(3): 263-268.
- Shyamalan G, Jordan RW, Kimani PK, Liverneaux PA, Mathoulin C (2016) Assessment of the structures at risk during wrist arthroscopy: a cadaveric study and systematic review. J Hand Surg Eur 41(8): 852-858.
- Garibaldi SG, Nucci A (2000) Dorsal cutaneous branch of ulnar nerve: An appraisal on the anatomy, injuries and application of conduction velocity studies in diagnosis. Arq Neuropsiquiatr 58(3A): 637-641.
- Mondelli M, Ginanneschi F, Aretini A (2019) Diagnostic accuracy of sensory clinical findings of the hand dorsum and of neurography of the dorsal ulnar cutaneous nerve in ulnar neuropathy at the elbow. Arch Phys Med Rehabil 100(5): 908-913.
- Le Corroller T, Bauones S, Acid S, Champsaur P (2013) Anatomical study of the dorsal cutaneous branch of the ulnar nerve using ultrasound. Eur Radiol 23(8): 2246-2251.
- Chang KV, Wu WT, Özçakar L (2017) Ultrasound imaging for dorsal ulnar cutaneous neuropathy with extensor carpi ulnaris tendinopathy. Am J Phys Med Rehabil 96(10): e191-e192.
- Chang KV, Mezian K, Naňka O (2018) Ultrasound imaging for the cutaneous nerves of the extremities and relevant entrapment syndromes: From anatomy to clinical implications. J Clin Med 7(11): 457.
© 2022 Yao-Wen Eliot Hu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






