- Submissions

Full Text
Research & Investigations in Sports Medicine
Available Interventions for Implicit Bias in Athletic Training
Cage SA1*, Decker M2, Vela L3, Scott R4, Jacobsen AP5,6, Volpi JD5,6, Warner BJ7 and Goza JP8
1The University of Texas at Tyler, USA
2The University of Texas at Arlington, USA
3The University of Arkansas, USA
4Abilene Christian University, USA
5The University of Texas Health Science Center at Tyler, USA
6UT Health East Texas, USA
7Grand Canyon University, USA/p>
8Collin College, USA
*Corresponding author: Cage SA, The University of Texas at Tyler, USA
Submission: August 09, 2022;Published: August 24, 2022

ISSN: 2577-1914 Volume9 Issue1
Abstract
Implicit biases are attitudes, emotions, or stereotypes that occur in an unconscious manner. Implicit biases have the potential to negatively affect behaviors, actions, and decisions. These implicit attitudes are not activated by conscious means, and as such can be difficult to acknowledge and address. There do not appear to be any studies that have examined the role of ethnic or racial implicit bias in the healthcare services provided by athletic trainers in current literature. Considering the racial, ethnic, and gender disparity in athletic training, implicit bias is an important factor to consider when assessing quality of patient care. In the absence of literature on implicit bias in athletic training, research on the impact of implicit bias in other healthcare professions must be considered. Current literature suggests that implicit bias toward vulnerable populations can have a negative impact on patient related outcomes. Although currently available research has several limitations, the potential for implicit bias negatively impacting patient outcomes is concerning. Interventions centered around setting goals and forming habits appear to be more effective than one time education sessions. Even in the presence of high-quality interventions, clinicians must still take responsibility for regular reflection and education to ensure they are mitigating the impact of any potential implicit biases on their clinical practice.
Introduction
Implicit biases are attitudes, emotions, or stereotypes that occur in an unconscious manner and have the potential to negatively affect behaviors, actions, and decisions [1,2]. These implicit attitudes are not activated by conscious means, and as such can be difficult to acknowledge and address [3]. Though implicit biases can produce a positive effect, the primary concern in most professions and fields of study are the potentially negative consequences. Whereas explicit biases are conscious attitudes or stereotypes that can be readily acknowledged and addressed, implicit biases can occur even when a person expresses beliefs that everyone deserves equitable care [1]. Because of its unconscious nature, implicit bias can be more difficult to assess and quantify than explicit biases which can be readily examined with verbal self-reports [4].
Presently, the most validated measure of implicit bias is the Harvard Implicit Association Test (IAT) [5-9]. The IAT measures implicit bias by measuring response time of unconscious associations when presented with demographic traits [8]. These traits include, but are not limited to race, disability, gender, ethnicity, and sexuality [8]. By categorizing words, labels, and pictures into opposing classifications as quickly as possible, the IAT provides a measurement of the participant’s implicit bias toward various traits [9]. Although the IAT is considered the gold standard for measuring implicit bias there are still limitations. The IAT requires the participant to have access to a computer or smart phone in order to complete the test. Additionally, the current algorithm for the IAT does not take into account factors such as the current stress level of the participant. Given that previous studies have reported stress as a factor for triggering implicit biases, knowledge of the participant’s level of stress would be valuable for these assessments [10]. Another confounding factor that exacerbates implicit bias is tiredness [11], which is another factor the IAT does not account for. Nevertheless, in the absence of other measures of implicit bias, the IAT remains the recommended tool for identifying and assessing implicit biases [5-9].
Implicit biases toward social groups are separated into two categories, stereotypes and affective evaluations [12]. Implicit stereotypes are characterized by associating members of a given social group with a pattern or theme of representations that may or may not be accurate [12]. Implicit affective evaluations are emotional states toward members of a demographic that can be positive or negative [13]. While both are considered implicit biases, recent studies have reported only a weak correlation between stereotyping and negative affective valences [12]. It is important to note that valence not only influences emotions, but also behaviors and choices. This appears to indicate that even if an individual’s negative emotions are activated, they may not hold unconscious stereotypes toward a given group of people [12]. Based on this information, individuals may engage in unconscious behaviors toward a group of people without unconsciously judging them [12]. The weak connection between implicit stereotypes and implicit emotions further confounds clinicians, educators, and researchers attempting to address implicit biases.
Recent studies have suggested that even when certain factors are controlled for, healthcare workers do not provide equitable care to patients from different demographics [12]. Even with the removal of characteristics traits such as socioeconomic status, level of education, and previous medical history, healthcare workers still appear to treat patients from different backgrounds differently. When patients are receiving different levels of healthcare in diagnostic, therapeutic, and preventative medicine, there is a potential for different patient-related outcomes. The literature describes healthcare professionals as individuals who take oaths to do no harm and espouse virtues such as fairness [14,15]. This makes the previous information both surprising and concerning. The purpose of this review is to describe the impact of implicit bias in healthcare professions, specifically athletic training, and to provide a summary of the most up to date interventions for mitigating the impact of implicit bias on healthcare outcomes.
Impact of Implicit Bias in Athletic Training
Within athletic training, healthcare competency has been rated as the top research priority for the profession [16]. To date, there does not appear to be any studies that have examined the role of ethnic or racial implicit bias in the healthcare provided by athletic trainers [16]. There has been one study that surveyed Gay, Lesbian, Bisexual, Transgender and Queer (LGBTQ+) National Collegiate Athletic Association (NCAA) student-athletes, which found that patients generally felt comfortable seeking healthcare from their athletic trainers [17,18]. Despite the paucity of research, it is a logical assumption that athletic trainers are subject to the same diagnostic and treatment flaws found in other healthcare professions. When considering the demographic composition of the athletic training profession, the potential for implicit bias becomes an even larger concern. Racial and gender demographics of NCAA athletic trainers, NCAA student-athletes, and the United States 2020 Census are presented in Table 1. There appear to be racial, ethnic, and gender disparities when comparing the demographics of NCAA athletic trainers to the general population and to NCAA student-athletes. These disparities have the potential to place individuals with negative implicit biases in situations where they are more likely to have these biases activated. Given the lack of research on the role of implicit bias in athletic trainers, it is valuable to consider the impact of implicit bias on the clinical practice of other healthcare professionals. For context, Table 2 presents demographic information of physicians in the United States compared to the United States 2020 Census and nationally certified athletic trainers.
Table 1: United States, NCAA Athletic Trainer, NCAA student-athletes racial, ethnic, and gender demographics [19,20].

Table 2: United States, physician, and nationally certified athletic trainer racial, ethnic and gender demographics [19,21,22]..
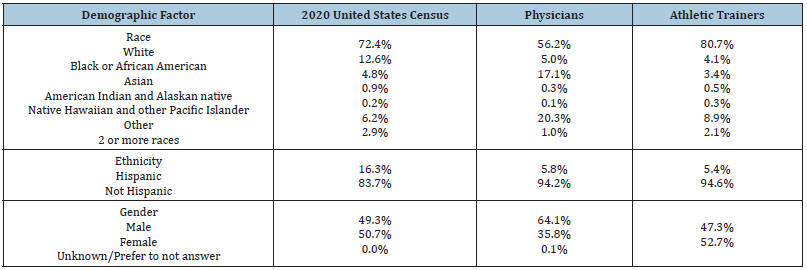
Values present in percentages.
Implicit Bias in Healthcare
Although implicit biases can be both positive and negative, the biases of concern for healthcare professionals are those that may create a disadvantage for a vulnerable population [23]. Often when people think of vulnerable populations, minority ethnic populations, immigrants, low socioeconomic status populations, sexual minority, children, women, geriatric populations, the overweight, and persons with disabilities come to mind [24]. However, it is worth noting that any individual may be considered vulnerable depending on the situation [24]. Another point of concern is the concept of “corrosive disadvantage” [25]. For instance, if an individual has a low socioeconomic status, they may be less likely to have medical insurance. If they do have medical insurance, it will likely have a higher deductible payment required to allow for a lower annual or monthly premium. Higher out of pocket expenses at the time of initial treatment may lead to patients delaying seeking care. If this hypothetical patient is receiving care from a clinician who holds a negative implicit bias toward their population, these disadvantages may have a cumulative impact on the patient’s outcomes.
Previous studies have shown evidence of negative implicit biases among healthcare workers toward black patients [26-40], females [30,32,33,41-45], both younger and older patients [33,41- 44,46], patients who are seen as having contributed to their own injury [47,48], patients with disabilities [49], and patients from lower socioeconomic status [30-32,50]. Despite the growing body of evidence to suggest that healthcare workers have the potential to hold implicit bias toward various vulnerable groups, the current research is not without limitations. A previous review noted the limitations in the current literature examining implicit biases in healthcare include studies that: do not report recruitment methods, do not report response rates, have low response rates, have participants who know the purpose of the study prior to assessment, have small sample sizes, or do not provide full information on statistical methods used [23]. These limitations leave some margin for error, particularly because some participants may have altered their behaviors knowing they were under scrutiny. The number of studies still provide compelling evidence that at least some healthcare professionals harbor negative implicit biases to at least some portion of their patient populations.
Impact of Implicit Bias on Diagnostics
In all facets of the healthcare field errors are inevitable [51]. Indeed, the errors made in diagnostic healthcare may be related to cognitive factors such as stress and tiredness as well as issues related to the healthcare system [47,48,52]. Previous reviews that examined studies describing autopsies that revealed clinically important or major errors reported a median error rate of 23.5% - 28.0% in adult and child inpatient settings [53,54]. Another review found that biases were associated with errors in diagnosis in 36.6% - 77.0% of case scenarios [55]. As hospital systems seek to improve on morbidity and mortality rates, checklists for decreasing risk support emerging research that suggests a correlation between bias and diagnostic errors [56-58]. No studies have examined clinical assessment and diagnostic errors in athletic training, but this evidence in related healthcare fields suggests the need for this same research in athletic training and sports medicine.
Impact of Implicit Bias on Treatment
Logic dictates that errors in diagnosis may impede timely and appropriate treatment. This inference appears to bear out in the current literature. A study by Green et al found that physicians who held pro-white implicit biases were less likely to recommend thrombolysis as a treatment for black patients and more likely to recommend thrombolysis for white patients [26]. There has also been a significant negative difference in choice of recommended treatment for older patients [46]. Physicians’ attitudes related to desire to help a patient also significantly decreased when treating patients who were considered to have contributed to their own injury [48]. Interestingly, pediatricians appeared to be less likely to be affected by any implicit bias they held when treating patients from different demographics [37,38].
Another concern when recommending treatments is patient adherence to a treatment plan. The research is conflicting regarding patient adherence to treatment when being cared for by a clinician with implicit bias. One study showed that pro-white implicit bias among healthcare providers resulted in black patients being less likely to fill a prescription [59]. However, this relationship was not found in Hispanic and Latinx patients [59]. An additional study was unable to find a significant relationship between implicit bias and treatment adherence by black patients at both four- and 16- week follow-ups [60]. This suggests that patients from various backgrounds are likely to remain adherent to a treatment plan regardless of their provider’s implicit bias. As with diagnostics, no studies have been conducted to examine the impact of implicit bias on treatment in athletic training. A review of the current literature examining the effects of clinical bias in other healthcare professions provides compelling evidence that would suggest that there is a need for studies to be conducted on this matter in athletic training and sports medicine.
Impact of Implicit Bias on Research
For healthcare professions to continue to advance in terms of diagnostic and treatment techniques, timely and relevant research is critical. Unfortunately, healthcare research and academia are not unaffected by implicit bias. This is especially concerning given that research is often considered to be free from outside influences. However, current research supports Saini’s commentary in 2019 that, “science is always shaped by the time and the place in which it is carried out” [61].
Studies have shown that small research institutions consistently have a 42% lower chance of being award research grants when compared to larger institutions [62,63]. Additionally, healthcare professionals often associate reputable and worthwhile research with countries with higher gross domestic products [64]. When assessed using a blinded crossover model, healthcare professionals’ assessments of research abstracts improved for lowincome countries [65]. Another systematic review reported that in addition to bias against certain countries, healthcare professionals were less likely to consider studies published in less prestigious journals [66]. This type of geographic and journal bias may lead to researchers not considering quality research from international sources based simply on its country of origin or the journal in which it was published in. These biases may prove to be barriers to research diffusion within the healthcare profession.
Interventions to Address Implicit Bias in Athletic Trainers and Healthcare Professionals
Perhaps the largest methodological flaw in addressing implicit bias is the assumption that the problem stems from lack of awareness [12]. This mindset is an issue because identifying one’s own bias is difficult to accomplish [9]. Additionally, even if a clinician can identify their bias, this recognition is only one component of decreasing the impact of that bias [9]. This is not to say that recognition of implicit bias is not critical to mitigating the issue. To intervene, a clinician must first recognize the flaw in their thinking [9]. In professions not related to healthcare, the most common strategies for mitigating implicit bias center around avoiding tiredness and stress [23]. It has also been suggested that blinding processes such as hiring and auditions can help decrease the impact of implicit biases [67,68]. However, these strategies can be difficult to implement in athletic training and other healthcare professions. Blinding would be unhelpful during diagnosis and treatment, as gender, race, and ethnicity can be important considerations during the clinical decision-making process [23]. Additionally, attempting to avoid tiredness and stress in clinical practice, especially athletic training, can be impractical [23].
Current implicit bias intervention strategies for healthcare professionals center around students taking the IAT and engaging in small group discussions on the nature of their bias [68-71]. Admittedly, the individual proposing these strategies recognize that these interventions may only be moderately effective [23]. Chief among the barriers to these strategies being effective is the risk of encountering resistance from clinicians not wanting to be labeled as biased [22]. Additionally, students must remain continually motivated to self-regulate their behaviors for this strategy to be effective [23]. A further limitation of these strategies is the questionable efficacy of a one-time information session and discussion group [72]. As previously mentioned, stress and tiredness can exacerbate implicit biases [10,11]. This makes increasing the cognitive load of a clinician when attempting to decrease the effects of implicit bias problematic.
Fortunately, there is recent literature that suggests the efficacy of unconscious processes to decrease stereotype activations and thereby decrease the effects of implicit bias on behavior [23]. This strategy aims to utilize the values held by many healthcare practitioners related to doing no harm and working to provide the best care possible [23]. Rather than a one-time intervention, this method seeks to have clinicians approach every patient encounter as an opportunity to reinforce their commitment to these values and behave accordingly [23]. This may be accomplished during education sessions during regular staff meetings, or through dedicated meetings with athletic training personnel. Substantial evidence supports this notion, as clinician who habitually attempt to meet egalitarian goals reflexively inhibit implicit biases when treating patients from vulnerable populations [73]. Even on an unconscious level, pursuing goals can become habitual [74]. Formation of these habits require a long period of education and training, as well as continuing education to reinforce these habits [23].
Summary
In this review we describe the impact of implicit bias on healthcare provided by athletic trainers and other healthcare professionals. Implicit bias is a reflexive reaction to individuals of various demographic backgrounds [1,2]. Individuals who experience implicit bias experience this phenomenon on two levels, stereotyping and affective emotions [13]. Presently, there does not appear to be any studies directly studying implicit biases held by athletic trainers. In the absence of direct evidence, it is still worth considering the role implicit bias plays on the healthcare provided by other clinicians. There is a growing body of evidence to suggest that implicit biases are held by at least some healthcare professionals [27-42]. These biases have the potential to negatively influence the outcomes of diagnosis and treatment of patients from vulnerable populations [27,49,60-62]. As such, this potential for negative patient related outcomes needs to be addressed.
Current interventions focus on one-time interventions that include identifying implicit bias and engaging in small group discussion [72-74]. This methodology does not account for the need to instill new habits to mitigate implicit attitudes and behaviors [73]. Ultimately, in order to better address the impact that negative implicit biases have on healthcare provision, clinicians must engage in regular reflection, education, and intervention to ensure the best possible outcomes for their patients [73,74]. While this undertaking may seem daunting, appealing to the egalitarian ideals upheld by most athletic trainers and other healthcare providers may provide the necessary motivation.
In conclusion, implicit biases have the potential to negatively affect patient related outcomes in healthcare. As responsible clinicians, it is important to maintain the highest possible standard of care for patients regardless of demographic factors. Doing so requires recognition of one’s own implicit biases. In addition to recognizing these biases, clinicians must engage in regular reflection on their practice. Clinicians must also continually affirm that the oath they undertook calls for them to practice in a manner that provides the best possible care for their patient regardless of demographic factors. Additionally, further research must be done to determine the impact of implicit bias on patient outcomes in athletic training. Until more awareness is brought to this issue, implicit bias will continue to have the potential to negatively affect patient outcomes in athletic training and the healthcare field in general.
Dedication
This review is dedicated to Arlo James Hamm, who was welcomed into the world during the production of this manuscript. There is no doubt that he will be raised to shine a light on the need for diversity, equity, and inclusion.
References
© 2022 Cage SA. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






