- Submissions

Full Text
Research & Investigations in Sports Medicine
Perineural Hydrodissection for Superficial Radial Nerve Compression Neuropathy: A Case Report
Craig J Van Tassel1,3 and Yao-Wen Eliot Hu2,3*
1Naval Health Clinic Quantico, USA
2Department of Physical Medicine, Naval Hospital Camp Pendleton, USA
3Department of Family and Community Medicine, Uniformed Services University for Health Sciences, USA
*Corresponding author: Yao-Wen Eliot Hu, Department of Physical Medicine, Naval Hospital Camp Pendleton, Department of Family and Community Medicine, Uniformed Services University for Health Sciences, USA
Submission: April 21, 2022;Published: May 17, 2022

ISSN: 2577-1914 Volume8 Issue4
Abstract
The Superficial Radial Nerve (SRN) is a sensory branch of the radial nerve that innervates the distal radial wrist and the radial dorsum of the hand. SRN neuropathy may occur at any point along the nerve, but entrapment is commonly noted distally between the brachioradialis and extensor carpi radialis tendons. Although SRN neuropathy is well documented in the literature, there are no reports of treatment involving perineural hydrodissection. Management is usually conservative with surgery reserved for recalcitrant cases. Presented is the first reported case of SRN compressive neuropathy treated with perineural hydrodissection in the literature. Perineural hydrodissection is a novel treatment for entrapment neuropathy that may be considered prior to surgical intervention.
Keywords: Superficial radial nerve; Perineural hydrodissection; Ultrasound; Case report
Abbreviations: SRN: Superficial Radial Nerve; ECR: Extensor Carpi Radialis; NSAIDs: Non-Steroidal Anti-Inflammatory Medications; EMG: Electromyography; MRI: Magnetic Resonance Imaging; D5W: 5% Dextrose in Water; TRPV1: Transient Receptor Potential Vanilloid Receptor-1
Introduction
The Superficial Radial Nerve (SRN) is a sensory branch of the radial nerve that innervates the radial side of the distal wrist and dorsum of the hand [1,2]. The SRN courses deep to the brachioradialis muscle, emerging superficially as it travels distally between the brachioradialis and the Extensor Carpi Radialis (ECR) tendons [3]. Injury or entrapment of the SRN is well documented in the literature dating back to 1932 when Wartenberg first described it as cheiralgia paresthetica in five cases [4,5]. SRN neuropathy may occur at any point along the nerve, but entrapment is commonly noted between the brachioradialis and ECR tendons from repetitive mechanical irritation [6]. Nerve injury is typically observed more distally due to distal radial fractures, handcuffs, wrist watches, wrist arthroscopy, acupuncture, or venipuncture [1,2,6-9]. Although SRN neuropathy is well known throughout the literature, there are no reports of treatment specifically with perineural hydrodissection to date. Historically, treatment options were limited to either conservative or surgical interventions. This is the first reported case of SRN compressive entrapment neuropathy treated with perineural hydrodissection in the current literature.
A 35 year-old right hand dominant male military service member presented with right dorsal radial wrist pain for 8 years. The pain was described as a pins-and-needles sensation or electrical shock with light touch and thumb extension. The symptoms began after a training exercise where he was handcuffed and tried to break free. He had failed prior splinting, Non-Steroidal Anti-Inflammatory Medications (NSAIDs), and physical therapy focusing on thumb extension and abduction. A first dorsal wrist extensor compartment corticosteroid injection performed by his primary care physician for presumed deQuervains tenosynovitis did not provide any immediate or delayed relief of symptoms. On examination, there were no skin changes or muscle atrophy of the forearm, wrist, or hand. He had full range of motion of the bilateral shoulders, elbows, wrists, and fingers with full strength throughout his bilateral upper extremities. There was diffuse discomfort with palpation of the distal radial wrist exacerbated by light touch, but sensation was otherwise intact in the radial, median, and ulnar nerve distributions. He exhibited positive Tinel’s sign along the course of the SRN and positive Finkelstein’s test. Watson’s, Phalen’s, Froment’s signs were all negative (Figure 1).
Figure 1:(A) Cross-sectional anatomy of the distal forearm. MN: median nerve; UN: Ulnar Nerve; UA: Ulnar Artery. (B) Sonoanatomy of the Radial Nerve (RN) at the forearm. RA: Radial Artery. SOURCE: NYSORA.COM
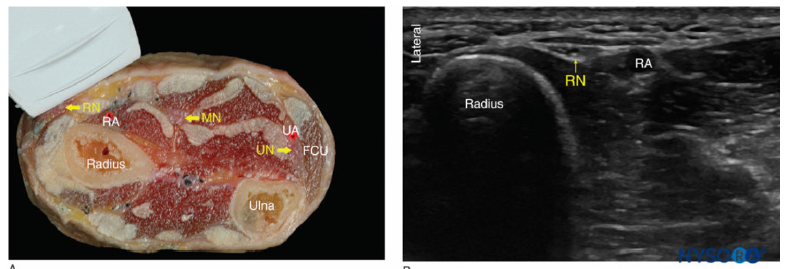
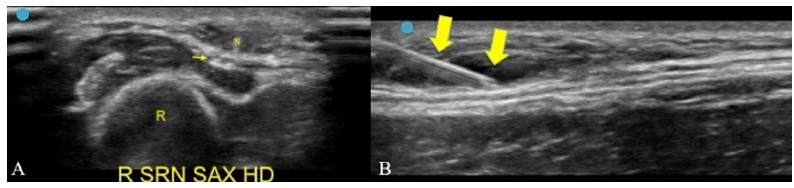
Plain radiographs of wrist were unremarkable. Point-of-care musculoskeletal ultrasound performed with the linear transducer transverse and long axis to first and second dorsal wrist extensor compartment tendons showed normal echogenic appearance without color uptake on power Doppler. Transverse views of the SRN exhibited normal hyperechoic and honeycomb appearance as it coursed between the brachioradialis and ECR tendons (Figure 1). However, as the nerve travelled distally there was flattening of the nerve, mild fascicular enlargement, and hypoechogenicity prior to branching. Further advanced imaging and diagnostic modalities such as Electromyography (EMG) and Magnetic Resonance Imaging (MRI) were not pursued in the interest of patient availability since there were limited clinical resources and he had an upcoming military move. After thorough discussion and shared decision making, he underwent diagnostic and therapeutic SRN perineural hydrodissection under ultrasound guidance (Figure 2). With the linear transducer positioned transverse to the SRN, a 25-gauge needle was used via a combination of in-plane and out-of-plane visualization to advance to the superficial then deep perineural space, where a total of 5 milliliters of 5% Dextrose in Water (D5W) was used to release the surrounding tissue from the nerve. The patient experienced immediate and continued resolution of his symptoms (Figure 2).
Figure 2:(A) Out-of-plane approach for ultrasound-guided perineural hydrodissection of the superficial radial nerve in transverse axis. R: Radius; N: needle tip. Thin arrow, superficial radial nerve. (B) In-plane approach for ultrasound-guided perineural hydrodissection of the superficial radial nerve in long axis. Thick arrows, needle.
Discussion
SRN neuropathy can be caused by compression or traumatic injury such as placement of handcuffs or venipuncture [1,2,6]. Patients often report dorsal radial wrist and hand paresthesia with allodynia [6]. Pain can be exacerbated by thumb and wrist movement, specifically wrist or thumb extension and ulnar deviation of the wrist. Patients often exhibit a positive Finkelstein’s test, leading to the misdiagnosis of deQuervain’s tenosynovitis and delayed treatment [10]. However, Tinel’s sign along SRN distribution is usually positive, distinguishing SRN neuropathy from deQuervains tenosynovitis [1,6]. Hand and wrist rangeof- motion and strength testing are often normal, although they may be decreased due to guarding. Radiographs and advanced imaging such as MRI may be helpful but are usually unremarkable and unnecessary to diagnose SRN neuropathy. EMG and nerve conduction studies also may or may not demonstrate delay [10]. Nerve ultrasonography can be beneficial and may reveal signs of entrapment, such as enlargement, flattening, or hypoechoic appearances with fascicular changes [11]. Management is initially conservative, consisting of activity modification, splinting, and physical therapy focused on improvement of elbow, wrist, and hand biomechanics [1,6]. Adjunct medication management with oral or topical NSAIDs and neuropathic medications such as gabapentin or pregabalin can be considered [1,2,6]. Conservative measures may be beneficial for symptom reduction but definitive treatment via surgical decompression or neurectomy may be needed especially in recalcitrant cases [1,2,6]. This case illustrates the failure of conservative treatment and avoidance of surgical intervention with perineural hydrodissection.
Awareness for perineural hydrodissection is increasing in the literature with use of high-definition ultrasound, leading to promise as novel treatment for peripheral mononeuropathy. Perineural hydrodissection is a procedure involving injection of fluid to separate the nerve from surrounding tissue over distance [12,13]. The injectate can be an anesthetic, saline, or D5W [12]. The benefit of nerve hydrodissection is not well understood, but a leading theory posits that dissecting the surrounding perineural tissue, whether it be fascia, tendons, muscle, or scar tissue, reduces compression of the nerve, allowing the nerves and vasculature supplying the nerve to function properly and the nerve to be healthier [12]. The choice of injectate also seems to be of importance, as D5W seems to provide greater benefit compared to other solutions [12,14]. It is postulated that D5W causes a downregulation of the Transient Receptor Potential Vanilloid Receptor-1 (TRPV1) ion channel and corrects glycopenia of the nerve [12]. In this case, there was no obvious post-procedural entrapment of the nerve exhibited on point-of-care musculoskeletal ultrasound, postulating that the D5W had a significant therapeutic effect.
Perineural hydrodissection is a novel and increasingly popular treatment for peripheral mononeuropathies using high-definition ultrasound. This case illustrates the benefit of perineural hydrodissection for SRN compressive entrapment neuropathy using D5W. There are multiple theories regarding the mechanism of action that provides benefit, whether it is mechanical decompression, chemical effect of the injectate, or a combination of both. More research is needed to show statistical benefit, but perineural hydrodissection may be considered as a treatment option for SRN neuropathy and other peripheral mononeuropathies prior to surgical consideration, especially in recalcitrant cases.
Acknowledgements and Funding
The views expressed in this publication are those of the authors and do not reflect the official policy or position of the Department of the Navy, the Department of Defense, Uniformed Services University of Health Sciences, or the U.S. Government. The authors declare no conflicts of interest and do not have any financial disclosures.
The authors are military service members of the United States Government. This work was prepared as part of their official duties. Title 17 U.S.C. 105 provides that copyright protection under this title is not available for any work of the United States Government. Title 17 U.S.C. 101 defines a U.S. Government work as work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
Conflict of Interest Statement
Yao-Wen Eliot Hu: AMSSM - Received honorarium as scanning faculty at the Fundamentals of Ultrasound Pre-conference at the AMSSM Annual Meeting. Craig J. Van Tassel: none
Permissions
NYSORA receives many permission requests to use NYSORA’s material. Since Education and Advancement of Practice of Anesthesiology are NYSORA’s primary missions, we grant you the permission to download and use NYSORA’s teaching material without asking for permission. However, you MUST acknowledge: “Source: NYSORA.COM” in all your slides and publications featuring any NYSORA’s material. Failure to visibly disclose the source constitutes a violation of copyrights laws & NYSORA’s intellectual property. For more information email: admin@nysora.com.
References
- Klitscher D, Müller LP, Rommens P (2007) Anatomical course of the superficial branch of the radial nerve and clinical significance for surgical approaches in the distal forearm. Eur J Trauma Emerg Surg 33(1): 69.
- Cho NS, Kim KH, Park BK, Kim DH (2016) Superficial radial sensory neuropathy: Medial and lateral branch injury. Muscle Nerve. 53(5): 690-693.
- Abrams RA, Brown RA, Botte MJ (1992) The superficial branch of the radial nerve: an anatomic study with surgical implications. J Hand Surg Am 17(6): 1037-1041.
- Braidwood AS (1975) Superficial radial neuropathy. J Bone Joint Surg Br 57(3): 380-383.
- Massey EW, Pleet AB (1978) Handcuffs and cheiralgia paresthetica. Neurology 28(12): 1312-1313.
- Meng S, Tinhofer I, Weninger WJ, Grisold W (2014) Anatomical and ultrasound correlation of the superficial branch of the radial nerve. Muscle Nerve 50(6): 939-942.
- Spies CK, Müller LP, Oppermann J, Neiss WF, Hahn P, Unglaub F (2016) Die operative Dekompression des Ramus superficialis des Nervus radialis: Das Wartenberg-Syndrom [Surgical decompression of the superficial radial nerve: Wartenberg syndrome]. Oper Orthop Traumatol 28(2): 145-152.
- Massey EW, Pleet AB (1978) Handcuffs and cheiralgia paresthetica. Neurology. 28(12): 1312-1313.
- Sheu JJ, Yuan RY (1999) Superficial radial neuropathy caused by intravenous injection. Acta Neurol Belg 99(2): 138-139.
- Saba EKA (2021) Superficial radial neuropathy: an unobserved etiology of chronic dorsoradial wrist pain. Egypt Rheumatol Rehabil 48: 29.
- Visser LH (2009) High-resolution sonography of the superficial radial nerve with two case reports. Muscle Nerve 39(3): 392-395.
- Lam KHS, Hung CY, Chiang YP, Onishi K, Su DCJ, et al. (2020) Ultrasound-guided nerve hydrodissection for pain management: rationale, methods, current literature, and theoretical mechanisms. J Pain Res 13: 1957-1968.
- Cass SP (2016) Ultrasound-guided nerve hydrodissection: What is it? A review of the literature. Curr Sports Med Rep 15(1): 20-2.
- Wu YT, Ho TY, Chou YC, Ke MJ, Li TY, et al. (2017) Six-month efficacy of perineural dextrose for carpal tunnel syndrome: A prospective, randomized, double-blind, controlled trial. Mayo Clin Proc 92(8): 1179-1189.
© 2022 Yao-Wen Eliot Hu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






