- Submissions

Full Text
Research & Investigations in Sports Medicine
Hydration and Physical Activity
Bojan Knap*, MD, PhD
Specialist of Internal Medicine, University Ljubljana, Slovenia
*Corresponding author: Bojan Knap, MD, PhD , Medical faculty, University Ljubljana, University Clinical Centre Ljubljana, Zaloška 6, Ljubljana, 1000, Slovenia
Submission: March 30, 2021;Published: April 20, 2021

ISSN 2578-0271 Volume7 Issue4
Abstract
The importance of water homeostasis is extremely important. Maintaining hydration, the state of preserving body water within its optimal homeostatic range, is essential to sustain life. Water is an essential nutrient and contributes 50-70% of total body mass. An assessment of hydration during physical activity can prevent dehydration, which impairs physical and cognitive performance. A 2% body mass loss is a recognized threshold beyond which exercise dehydration impairs exercise performance. Liquid needs for recreational sports and physical activity are individual and are rarely higher than 500ml of hypotonic fluid per hour. If fluid requirements are low, concentrated sports drinks (providing energy intake) can help sustain exercise performance. Overhydration could be dangerous and can result in hyponatremia. Individual evaluation of water needs is important. In warm environmental conditions, an individual nutrition and hydration plan is crucial for the health and optimal performance and using existing recommendations in clinical sports nutrition to prevent over - and dehydration.
Keywords: Water homeostasis; Hydration plan; Physical activity
Introduction
Water can be considered an essential nutrient in the diet because our body is mainly made up of water. Keeping the Total Body Water (TBW) content within the appropriate levels is important for health and well-being. Maintaining hydration, the state of preserving body water within its optimal homeostatic range, is essential to sustain life. Water contributes 50-70% of total body mass and is compartmentalized within intracellular (65%) and extracellular (35%) spaces [1]. Euhydration is typically maintained throughout day-to-day life via behavioural and biological controls [2].
Regulation of Water Homeostasis
Regulation of fluid intake
The main signal for water intake is thirst. Similarly to appetite, water intake is regulated by thirst, and the right amount of water intake is dictated by the balance between the intake and the losses. The intake comes from both fluids and solid foods. Fruit and vegetables are the major sources of water from food. Water is also produced during the oxidation of macronutrients, although the amount is often negligible. Water loss from the body occurs through the urinary system, the skin, the gastrointestinal tract, and the respiratory surface. In extreme circumstances, water intake regulation by thirst is impaired which can have a negative influence on optimal body fluid content. In such circumstances an individual nutrition and hydration plan is necessary.
Fluid needs of the human body
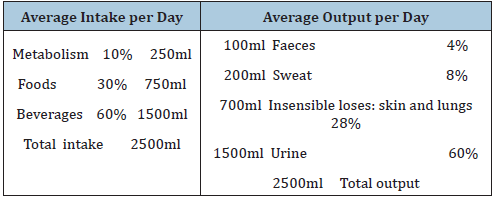
Generally, the human body needs about two litres of water per day [3]. A typical balance of human fluid needs per day is shown in Table 1; [3].
Humans have a remarkable capacity to maintain constant osmolarity of Extracellular Fluid (ECF) through both behavioural responses and physiological mechanisms that restore ECF to the homeostatic values which are crucial to maintaining the circulatory system. A normal circulatory system is crucial for normal homeostasis of human body cells, efficient thermoregulation and normal gastrointestinal function. Water is constantly being lost from the body together with metabolic products excreted through kidneys (1 litre of urine), gastrointestinal tract (100ml in faeces) and insensible losses from skin and lungs (Table 1). Osmoreceptors in the hypothalamus and controlled secretion of the antidiuretic hormone are crucial for the regulation of osmolality of the plasma, acting together with the renin-angiotensin system on the kidney to maintain fine regulation of the
content of body water [2].
Table 1: Balance of human fluid (adapted from 3).
Influence of exertional stress on hydration
Intense prolonged exercise can cause an acute disruption of body fluid balance through increased loses of hypotonic fluid in the form of sweat. Dehydration causes cardiovascular strain and if prolonged, in extreme situations also hyperthermia, gastrointestinal system failure, heat cramps and death [4]. Fluid balance - the optimal ratio between fluid intake and losses is crucial for the athlete’s optimal performance and safety during exercise, especially in hot environmental conditions.
Thermoregulation and Exercise Performance
Influence of normal body fluid contents and thermoregulation
Normal thermoregulation depends on the body being in a hydration state with a healthy cardiovascular system, both of which are dependent on the correct long-term balance between loss and intake of fluids. Many factors impact total fluid volume, including water and sodium intake, environmental temperature, evaporation, intensity and duration of physical activity. Dehydration increases cardiovascular strain by reducing blood volume through fluid loss, thereby decreasing stroke volume, and increasing heart rate. When core temperature increases as a result of exercise and dehydration, elevated skin blood flow displace blood away from the central blood volume, exacerbating cardiovascular strain [4,5]. In addition to this increase in cutaneous blood flow, sweat production increases to dissipate heat to the environment through evaporative cooling. Sweat glands produce a fluid hypotonic about plasma, by drawing fluid from the ECF concomitant with reabsorption of sodium and chloride. This results in both a decrease in total body water volume and an increase in ECF osmolality which triggers water movement from plasma and intracellular stores to restore osmolality in the interstitial fluid compartment [6]. Osmotic fluctuations in extreme circumstances, if severe enough, can have serious health consequences, such as weakness, cardiac arrest, spasticity, coma, seizures, and death [7].
Loss of more than 2% of body weight impairs thermoregulation and exercise performance
Dehydration higher than 2% of body mass impairs thermoregulation and negatively affects exercise aerobic performance, independent of thermal, dietary, or metabolic stressors [4]. The results of successful prevention of water loss >2% of total body weight are shown in Figure 1. For example, an athlete with a weight of 70kg would need to drink a volume of fluid equal to 2.6 ± 0.7L to prevent >2 ± 1% dehydration when losing 4L of body water, such as during a marathon (42.1km). During shorter distances such as 5 or 10km when fluid losses are unlikely to reach or exceed 2% dehydration, the same athlete would not need to ingest fluids during the competition as fluid losses are <2% body mass [3].
Figure 1: Target fluid replacement to avoid loss of 2% of body mass.

Extreme exertional heat stress in extreme circumstances
Exercising in a hot environment amplifies dehydration which can lead to a vicious circle. During exercise, heat stress is present in hot environments (high air temperature and high humidity, without wind) and sports with clothing or equipment that prevent loss of body heat (eg motorsport, ice hockey). This process can lead to prolonged stress that can perturb thermoregulatory, cardiovascular and gastrointestinal systems. Prevention of dehydration and its detrimental impact on exercise performance can be achieved by careful planning of pre-and inter-race fluid and electrolyte replenishment.
Assessment of acute and long-term fluid needs
Factors influencing hydration status of the body.
Many factors influence the hydration status of the human body:
1. Environmental conditions,
2. Availability of fluids,
3. Structure of exercise (duration, type and intensity of
exercise,) and
4. Intrinsic factors (body weight, acclimatization status,
thirst drive) and sport-specific factor (bodyweight categories,
body composition) [3].
Assessment of hydration needs of the body
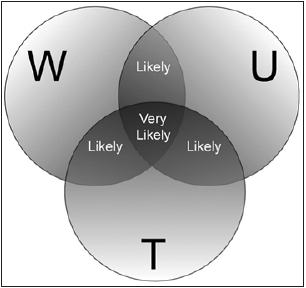
Hydration assessment can be utilized to indicate the current hydration state, but if measured repeatedly, it can also be used to track changes in hydration and indicate fluid needs. Bodyweight changes, thirst, amount and colour of urine are important evaluation indices in long term observation and prevention of dehydration [8] (Figure 2). Bioelectrical Impedance Analysis (BIA) is relatively new and very convenient, considered by some to offer the current gold standard to evaluate body hydration. Plasma osmolality, changes in plasma volume, and the volume, osmolality and specific gravity of urine are the most commonly published metrics to assess changes in hydration status in clinical settings. Infield applications, the careful assessment of changes in body mass over a bout of physical activity provides a reasonably accurate assessment of body water deficits incurred during the session since sweat loss and fluid intake during the session underpin the major changes in body mass and body water content [9].
Figure 2: The diagram showing the likelihood of
dehydration related to certain conditions. From
Cheuvront & Sawka [8] (public domain).
Abbreviations: W: Weight; U: Urine; T: Thirst
Sweat loss assessment as acute evaluation of fluid needs
The method for assessing sweat losses is the assessment of the athlete’s body mass before and after exercise. Sweat loss (water and sodium) varies greatly between individuals ranging from 0.6 to 1.9 litres per hour [10-12]. Accounting for any fluid consumed or urine excreted, the difference between body weight before and after exercise can be used to calculate the amount of sweat lost as well as the residual fluid deficit that should be addressed in postexercise recovery plans [13]. The monitoring of daily changes in body mass, coupled with urine colour and thirst sensation status provides adequate sensitivity for most athletic situations except for sports in high mountain situations where the respiratory loss of fluids could be important [14]. In winter condition (cold and dry air) in some long-term exercise (long ski run, long-endurance skating, alpine skiing, alpinism, cross country skiing) respiratory fluid loss is important.
Constant evaluation of fluid needs
Useful criteria established for evidence of sustained dehydration include body mass changes greater than 1.1%, a conscious desire for water (thirst), and dark-coloured urine, indicating varying degrees of fluid inadequacy [15,16]. Two of these factors combined suggest that daily fluid intake is likely inadequate, while the presence of all three factors indicate that daily fluid intake is very likely inadequate (Figure 2). It should be noted that this assessment technique is based on first morning values and requires baseline body mass values to provide the most useful information to athletes.
Practical recommendations on hydration in physical activity
Rule of 2% of body mass: The basic principle is using the assessment of fluid needs in an environment similar to race conditions. Recreational runners rarely achieve weight loss greater than 2% of body weight (1.4kg in 70kg athletes) if exercise/ competition is started in a well-hydrated state [17,18]. Starting exercise in the euvolemic state is very important. Good nutrition and hydration planning also include a hydration strategy during exercise and for optimal recovery after exercise as well [10].
Intensity and duration of exercise in warm weather
Carefully monitoring acute changes in body mass over an exercise bout is important to determine sweat rate and adequacy of fluid replacement. Fluid replacement is crucial in recovery optimization. Changes in body mass, urine colour, and thirst upon awakening are useful in tracking daily changes in hydration status. Slow pace runners generally show a loss of 2% of body weight due to dehydration only in marathon runs in hot weather (temperature of ≥30 degrees Celsius). Runners who participate in 10km and half-marathon distances lose less than 2% of body mass [18]. Fluid losses of more than 2% of body mass are considered significant for exercise performance and are associated with decrements in aerobic performance [11]. Therefore, intensive rehydration is not always necessary, but it is important in warm weather and during the exercise of long duration (more than 2 hours).
Exercise intensity is the main factor that determines metabolic heat production, meaning that the rate of fluid losses from sweat for a given exercise session can be partially explained by the intensity of exercise. Total fluid losses are a result of the sweat rate of given exercise intensity and the total duration of that activity [17]. In most circumstances, there is an inverse relationship between the exercise intensity of a session and the duration of that session. However, given the wide variability in individual sweat rates, the unique interplay between intensity, duration and sweat rate must be considered in unison. For example, a runner with a 2L/h sweat rate who completes a marathon in 2h will accumulate the same fluid losses as a runner with a 1L/h sweat rate that completes the race in 4h [17-19]. Ultra-endurance racers such as RAAM (Race Across America) competitors (except for the part of the race that takes place in the desert) prefer relatively small volumes of hypotonic fluid (300-600ml per hour) and solid food [20-22]. General recommendations for nutrition and hydration regime are very difficult and unusable in individual conditions.
Overhydration occurs at a slow pace, whereas at a fast pace fluid intake is sometimes inadequate
Slower runners sometimes overhydrate and are at risk for Exercise-Associated Hyponatraemia (EAH) [23]. EAH is defined
Slower runners sometimes overhydrate and are at risk for Exercise-Associated Hyponatraemia (EAH) [23]. EAH is defined as a serum sodium concentration less than 135mmol/l during or up to 24 hours after prolonged physical activity [23]. A sodium concentration of less than 135mmol/l can be associated with a range of sign and symptoms, such as nausea, headaches, and seizures. EAH is a potentially fatal condition (pulmonary, cerebral oedema, unconsciousness, death) that can be prevented by avoiding excessive water or hypotonic fluid intake. The use of thirst as a guide for the hydration plan, with the evaluation of sweat rate and checking body weight before and after the race, is the best prevention strategy for EAH. About 5% of runners in the 2014 London marathon planned to drink more than 3.5l of fluid during the race and those runners were surely candidates for EAH. On the contrary Gastrointestinal (GI) dysfunction is commoner in runners competing at a high intensity (an intensity at which oxygen consumption reaches >75% VO2max) [24]. At oxygen consumption,>75% VO2max gastrointestinal strain increases, and adequate fluid and electrolyte intake are often impossible. Prolonged intensive exercise in hot conditions exacerbates the exercise-induced gastrointestinal syndrome which causes the redistribution of blood flow away from the gastrointestinal tract toward skeletal muscles and results in gastrointestinal ischemia [24]. The hydration regimen must also be allowed to adapt to specific rehydration fluids at the right time for adaptation of the gastrointestinal system as well. This has to be done in the preparation period to avoid GI dysfunction during competition. Comparison of body mass pre-and post-exercise will help guide the athlete in understanding whether their hydration strategy during activity was effective in achieving acceptable fluid balance, as well as knowing the volume of fluids that are needed following exercise to return to baseline hydration levels before the next exercise session [10]. Water or beverage intake must be tailored to specific needs of exercise, especially in situations where access to liquids is limited or when frequent breaks for urination are not possible [9]. Dehydration could also affect cognitive, technical and physical performance in team sports [25]. The race strategy for individual evaluation of fluid and energy needs should be developed before a race and in similar conditions. A nutrition protocol with optimization of glycogen reserves forms part of the hydration protocol for successful racing [10]. About 500ml of isotonic fluid before exercise and a similar amount per hour of exercise, if the exercise is for longer than 1.5 hours, is usually enough. After racing optimal hydration is achieved with an intake of approximately 150% of hypotonic or isotonic fluid for the amount of fluid loss (change in body mass before and after the race) [18].
Summary
Liquid needs for recreational sports and physical activity, especially in prolonged exercise in hot conditions, are individual and are rarely higher than 500ml of hypotonic fluid per hour. About the importance of hydration, a 2% body mass loss is a recognized threshold beyond which exercise dehydration impairs aerobic exercise performance and this is further exacerbated in warm and hot environments. If fluid requirements are low, concentrated sports drinks (providing energy intake) or gels can help sustain exercise performance. Overhydration could be dangerous in slower events of longer duration, where more than 500ml of water per hour can result in hyponatremia. Individual evaluation of water needs is important. In warm environmental conditions, an individual nutrition and hydration plan is crucial for the health and optimal performance.
References
- Sawka M, Pandolf KB (1990) Effects of body water loss on physiological function and exercise performance. In: Gisolfi C, Lamb DR (Eds.), Perspectives in Exercise Science and Sports Medicine. Benchmark Press, Carmel, CA, USA, 3: 1-38.
- Sawka MN, Wenger CB, Pandolf KB (2011) Thermoregulatory responses to acute exercise-heat stress and heat acclimation. in comprehensive physiology. In: Terjung R (Ed.), John Wiley & Sons, Hoboken, NJ, USA, pp. 97-151.
- Belval LN, Hokosawa Y, Casa DJ, Adams WM, Armstrong LE, et al. (2019) Practical hydration solutions for sports. Nutrients 11(7): 1550.
- Mountain SJ, Coyle EF (1992) Influence of graded dehydration on hyperthermia and cardiovascular drift during exercise. J Appl Physiol 73(4): 1340-1350.
- Cheuvront SN, Carter R, Sawka MN (2003) Fluid balance and endurance exercise performance. Curr Sports Med Rep 2(4): 202-208.
- Bhave G, Neilson EG (2011) Body fluid dynamics: back to the future. J Am Soc Nephrol 22(12): 2166-2181.
- Bourque CW (2008) Central mechanisms of osmosensation and systemic osmoregulation. Nat Rev Neurosci 9(7): 519-531.
- Cheuvront SN, Sawka MN (2005) Hydration assessment of athletes. Gatorade Sports Science Institute. Sport Sci Exch 8: 1-5.
- Maughan RJ, Watson P, Cordery P AA, Neil P Walsh, Samuel J Oliver, et al. (2016) A randomised trial to assess the potential of different beverages to affect hydration status: development of a beverage hydration index. Am J Clin Nutr 103(3): 717-723.
- Maughan RJ, Shirreffs SM (2010) Dehydration and rehydration in competitive sport. Scand J Med Sci Sports 20(Suppl3): 40-47.
- Sawka MN, Burke LM, Eichner ER, Maughan RJ, Montain SJ, et al. (2007) American college of sports medicine position stand. Exercise and fluid replacement. Med Sports Exerc 39(2): 377-390.
- McDermott BP, Anderson SA, Armstrong LE, Casa DJ, Cheuvront SN, et al. (2017) National Athletic trainers association position statement: fluid replacement for the physically active. J Athl Train 52(9): 877-895.
- Armstrong LE, Casa DJ (2009) Methods to evaluate electrolyte and water turnover of athletes. Athl Train Sports Health Care 1(4): 1-11.
- Cheuvront SN, Kenefick RW (2016) Am I drinking enough? yes, no, and maybe. J Am Coll Nutr 35(2): 185-192.
- Armstrong LE, Maresh CM, Castellani JW, Bergeron MF, Kenefick RW, et al. (1994) Urinary indices of hydration status. Int J Sport Nutr 4(3): 265-279.
- Cheuvront SN, Sawka MN (2005) Hydration assessment of athletes. Sports Sci Exch 18(2): 1-12.
- Cheuvront SN, Kenefick RW (2017) CORP: Improving the status quo for measuring whole-body sweat losses. J Appl Physiol 123(3): 632-636.
- Kenefick RW, Cheuvront SN (2012) Hydration for recreational sport and physical activity. Nutr Rev 70(2): 137-142.
- Shirreffs SM (1999) Heat stress, thermoregulation, and fluid balance in women. Br J Sports Med 33(4): 225.
- Hoffman MD (2019) Proper Hydration during ultra-endurance activities. Sports Medicine and Arthroscopy Review 27(1): 8-14.
- Nikolaidis PT, Veniamakis E, Rosemann T, Knechtle B (2018) Nutrition in ultra-endurance: State of the art. Nutrients 10(12): 1995.
- Knap B (2011) Nutritional practice of the race across America winner: A case report. In: Doral MN, Reha NT, Gideon M, René V (Eds.), Sports injuries: prevention, diagnosis, treatment and rehabilitation. (2012th edn), Springer Publications, USA, pp. 1247.
- Knechtle B, Chlíbková B, Papadopoulou S, Maria Mantzorou, Rosemann T, et al. (2019) Exercise-associated hyponatremia in endurance and ultra-endurance performance-aspects of sex, race location, ambient temperature, sports discipline, and length of performance: A narrative review. Medicine (Kaunas) 55(9): 537.
- McCubbin AJ, Allanson BA, Odgers JNC, Cort MM, Costa JSR, et al. (2020) Sports dietitians Australia position statement: Nutrition for exercise in hot environments. Int J Sport Nutr Exerc Metab 30(1): 83-98.
- Nuccio PR, Barnes AK, Carter MJ, Baker LB (2017) Fluid balance in team sport athletes and the effect of hypohydration on cognitive, technical, and physical performance. Sports Med 47(10): 1951-1982.
© 2021 Bojan Knap. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






