- Submissions

Full Text
Research & Investigations in Sports Medicine
Acetabular Labral Lesions Always Present in End-Stage Osteoarthritis
Bashar Reda1, Adam Harris2, Nathan Urquhart3, Douglas LeGay3, Mark Glazebrook3, and Ivan Wong3*
1Assistant professor, King Abdul-Aziz University, Saudi Arabia
2Department of Emergency Medicine, Faculty of Medicine, Dalhousie University, Canada
3Division of Orthopaedic Surgery, Department of Surgery, Faculty of Medicine, Dalhousie University, Canada
*Corresponding author: Ivan Wong, Dalhousie University, 5955 Veteran’s Memorial Lane, Room 2106 VMB, Halifax, Nova Scotia, Canada
Submission: May 04, 2020;Published: June 19, 2020
ISSN: 2577-1914 Volume6 Issue4
Abstract
The purpose of this pilot study was to explore the relationship between pathologies in the acetabular labrum and end-stage osteoarthritis (OA). The study design was a prospective observational case series of 10 patients undergoing total hip replacement for end-stage OA. The arthroplasty procedure was performed using a standard lateral approach. An arthroscope was used along with a 5-mm probe to examine the labrum and the cartilage on the femoral and acetabular sides. Two blinded hip arthroscopy surgeons viewed the recordings and assessed the presence and location of labral tears and cartilage lesions according tothe Lage and Outerbridge classifications, respectively. The mean age of the 10 patients was 67 years. Labral pathology clustered in the anterior-superior quadrant was detected in all 10 hips. Tear patterns included longitudinal peripheral tears, fissuring, and large unstable tears. Significant inter-observer variability was noted. In all hips with focal acetabular articular lesions (40%), the lesion was located immediately adjacent to the labral pathology. In conclusion, all patients with end-stage OA were found to have a labral tear. The pathology, which was predominantly located in the anterior-superior part, was also a common site of more focal arthritic changes. This suggests that labral tears could be associated with the development of OA, indicating directions for further studies on this connection.
Level of Evidence: Level II
Keywords: Hip; Labrum; Lage; Lesions; Osteoarthritis; Outerbridge
Abbreviations: OA: Osteoarthritis; THR: Total Hip Replacement
Introduction
In the last decade, there has been growing interest in acetabular labral pathology, with a substantial increase in publications on diagnostic and therapeutic factors related to the preservation of hip joints. The acetabular labrum is a fibro-cartilaginous horseshoe-shaped structure directly attached to the acetabular rim. It is continuous with the articular hyaline cartilage of the acetabulum through a zone of calcified cartilage and inferiorly continuous with the transverse ligament. It is widest anteriorly and thickest superiorly [1]. As the labrum has no intrinsic blood supply, it receives blood from a vascular ring located on its capsular side [1,2].
The labrum was previously thought to perform unimportant biomechanical function [3]. However, recent evidence has revealed its anatomical value [1,4-8]. Its functions include the distribution of upper body pressure, shock absorption, proprioception, cartilage nutrition, and hip joint stability [9,10]. As we are becoming increasingly aware that subtle changes in normal hip anatomy may eventually lead to cartilage pathology, the effects of such changes need to be further quantified. What were previously thought to be “primary” osteoarthritis (OA) of the hip could likely be the result of minor structural changes in the hip, such as femoral acetabular impingement or a labral tear, as suggested by Ganz et al. [11]. Given this new area of inquiry, the role of the labrum in cartilage health and the onset of hip OA should be explored.
The causes of labral tears are defined in the literature as either traumatic or atraumatic. Atraumatic causes include developmental dysplasia, femoral acetabular impingement, degeneration, and microinstability. Traumatic causes are far less common and typically involve either subluxation or dislocation of the femoral head [2,9,10]. Labral tears usually present with anterior hip and groin pain or mechanical symptoms such as clicking, locking, and giving way [9]. Despite health professionals’ increased awareness of the condition, it is one of the frequently missed diagnoses, and often the symptoms remain unidentified for years. This is partly due to the lack of consensus in proper diagnostic tools, as arthrography is considered one of the better diagnostic tools, while arthroscopy is considered the gold standard for detecting labral tears [10,12,13].
A growing number of cadaveric and biomechanical studies have produced evidence suggestive of a potential role of labral tear in the development of end-stage arthritis of the hip joint [1-3,5-7,11,14-20]. A study that included 436 consecutive arthroscopies in hips with mechanical symptoms and no radiographic evidence of OA found that 77% of the patients who had labral tear exhibited articular cartilage damage. In 90% of the cases, the articular cartilage damage and labral tears were located in the same zone in the acetabulum, suggesting that labral tears can double the risk of chondral erosion [17].
In 1996, Lage et al. [21] developed a classification system for labral pathologies, commonly called the Lage classification. The system takes into account the etiology, shape, and extent of tears in the labrum [21] and can be used to quantitatively assess the extent of labral damage. For the assessment of acetabular cartilage damage, Outerbridge developed a descriptive system for a better understanding of the etiology of chondromalacia of the patella, which has been used to grade the severity of cartilage erosion afterwards [22]. The reasoning was that if labral tears were established as a precursor for OA, proper prevention and early intervention programs could be implemented.
Hypothesis and Purpose
We hypothesized that patients with end-stage hip OA present with labral pathologies. Therefore, the primary purpose of this pilot study was to examine the relationship between pathologies in the acetabular labrum and end-stage OA. The primary outcome was the description of the location and severity of the labral pathologies. The secondary outcome was to determine the feasibility and reliability of our measurement tools with a view to conducting a larger cohort study.
Materials and Methods
The study design was a single-center prospective observational case series conducted (blinded for review). Patients diagnosed with end-stage OA who were to undergo total hip replacement (THR) surgery were included in the study. Participants requiring THR for indications other than OA or had previous operations on or prior fractures or metabolic conditions in the hip were excluded from the study. A total of 10 patients (5 males and 5 females) who met the inclusion criteria were enrolled. The patients’ ages ranged between 50 and 85 years, and their mean age was 67 years. Six right and four left hips were examined. The study was approved by the institutional ethics board, and all patients signed informed consent forms.
Routine preoperative X-ray weight bearing anterior-posterior pelvis and frog lateral views of the studied hips were obtained. Using these images, the Kellgren-Lawrence stage for each hip was determined by an orthopedic surgeon blinded to the hips’ conditions.
Surgical technique
A standard THR procedure was performed by an arthroplasty surgeon. The only modification to the technique was a 360-degree assessment of the femoral head and the acetabulum using an arthroscopy system. Following anesthesia induction and endotracheal intubation, the patients were placed in the lateral decubitus position, and after standard surgical site preparation, the hip joint was approached laterally. Once the surgeon was down to the capsule, an arthrotomy was performed, exercising care to avoid iatrogenic injury to the labrum.
Videos recorded by the arthroscope were used to provide magnified views of the labra. A clock face system was used to allow the labral lesions to be localized anatomically along with acetabular lesions using a four-quadrant system (Figure 1), which facilitates reproducibility in future studies. The 6 o’clock position on the femoral head and neck, which corresponds to the middle of the transverse ligament on the acetabulum, was double-marked by electrocautery prior to making the neck cut to avoid losing the orientation to the head once it was out of the acetabulum. Appropriate retractors were then placed to achieve a full 360-degree view of the acetabulum.
Figure 1: Division of the acetabulum into four quadrants to standardize assessment and reporting of findings.

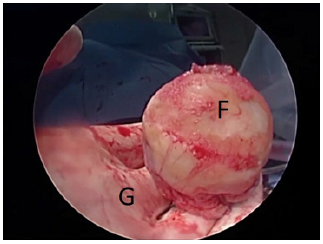
The labrum was dynamically examined using a 5-mm probe and video recording on the arthroscopy system. The surgeon started with a five-second view of the entire labrum and acetabulum (Figure 2). Next, starting at the 6 o’clock position, the surgeon probed the labrum, spending 10 seconds on each quadrant. The surgeon then spent 10 seconds examining the articular cartilage for signs of decay using the transverse ligament as a reference and the 5-mm probe as a gauge for size. The surgeon then examined the femoral head and neck for structural abnormalities and cartilage defects for 15 seconds (Figure 3). The videos were then de-identified and saved for later analysis by the principal investigator, who specializes in hip arthroscopy, and a second researcher with a fellowship in hip arthroscopy. The prevalence of labral tears was determined and qualitatively described and classified according to the Lage classification, the only available arthroscopic classification [21] (Table 1).
Table 1: Comparison of the two blinded surgeons’ findings.
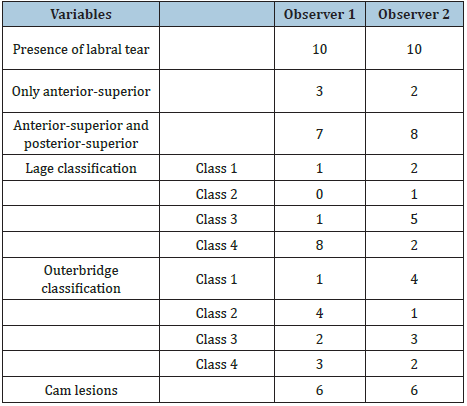
Figure 2: Identification of a labral tear (L:labrum; A:acetabulum).
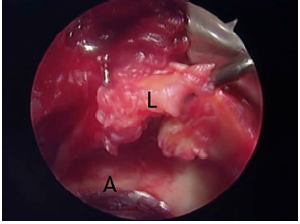
Figure 3: Assessment of the femoral head for pathology (F: femoral head; G: gloved hand).
The observers also described the articular cartilage pathology on the acetabular and femoral sides. The anatomic location of such pathology was described using the same quadrant system used for the labrum, with the midpoint of the transverse ligament being at the 6 o’clock position and the corresponding electrocautery double mark at the 6 o’clock position on the femoral side. The size of the lesion was measured using the 5-mm probe and classified according to the Outerbridge classification [22] (Table 2).
Statistical Analysis
Only descriptive statistics are reported.
Results
Six right and four left hips were included in the study, with an average joint space of <1mm and Kellgren-Lawrence stage 3 or 4, as determined from preoperative images. As shown in Table 1, all hips were found to have a labral tear by both blinded observers. The major focus of the labral tear in all hips was in the anterior-superior location. In 70% of the hips, extension of the labral tear to the posterior-superior quadrant was observed by at least one observer, with 70% inter-observer agreement. The labral pathology was identified as longitudinal unstable tear, fissuring, or large unstable tear. There was significant variability in the two observers’ descriptions of arthritic labral pathology according to the Lage classification, with only 30% agreement (Table 2).
Articular cartilage lesions were detected in all hips, with 100% agreement between the two observers. However, there was only 10% agreement in terms of Outerbridge scores. In 40% of the hips, there was agreement on the location of the cartilage lesion only adjacent to the labral tear and in the same quadrant as the labral tear (Table 2). In one patient, the femoral head was not captured in the video clearly enough to assess cartilage loss and cam lesion. Femoral cartilage loss was observed in all the remaining nine hips, with 100% inter-observer agreement. There was 78% agreement regarding the presence or absence of cam lesions (seven of nine hips). Cam lesions were detected by both observers in five of the nine hips (56%) (Table 2).
Discussion
In this study, both observers found a labral tear in all (10) patients undergoing THR for end-stage OA. All of them had tears in the anterior-superior location, and most (at least seven) had tears in the posterior-superior location as well. To the best of our knowledge, no previous studies have investigated the prevalence of labral tears in living patients with end-stage OA. However, cadaveric studies have shown a high prevalence in individuals with osteoarthrosis and hip pain [1,23]. Seldes et al. [1] examined 55 hips of adult individuals with a mean age of 78 years and found that 96% had labral tears, 74% of which were located in the anterior-superior quadrant. They also found grade 1-4 articular cartilage lesions in more than 85% of the femoral heads and acetabula and reported that in 33% of the hips, the focal articular cartilage pathology on the femoral head was in the same location as the labral tear. These findings are consistent with our study, where the focus of labral pathologies was mostly located in the anterior-superior quadrant of the labrum. McCarthy et al. [17] attributed this high prevalence of anterior labrum pathology to its hypovascularity and inferior mechanical properties, as well as to the fact that it is subjected to greater mechanical stress than other parts of the labrum.
Table 2: Labral tear and acetabular cartilage lesion localization and grading by the two blinded observers using video recordings of THR prior to excision of the femoral head.
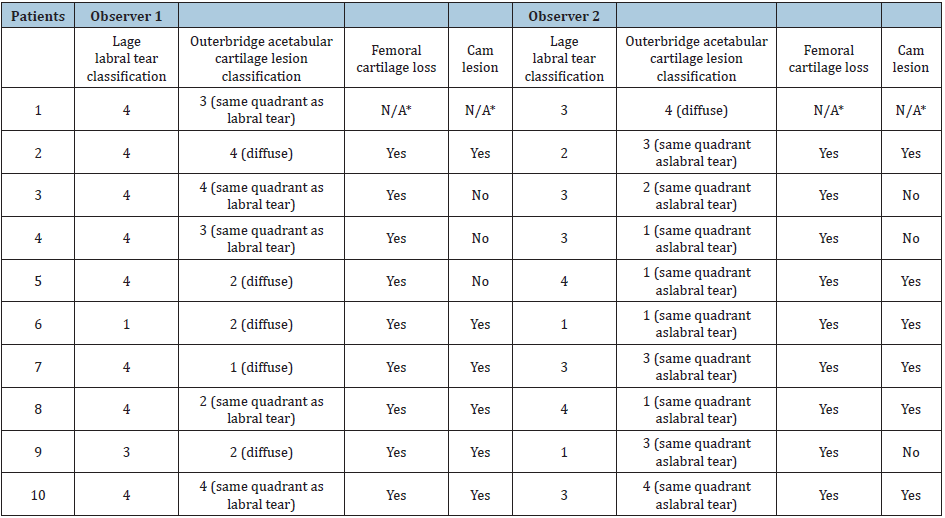
*Femoral cartilage loss and cam lesions were not assessed in Patient 1 due to poor video quality.
Acetabular articular cartilage lesions were detected in all 10 hips by both observers in this study. In 40% of the cases, the cartilage defect was limited to the area immediately adjacent to the labral tear, which is in line with other studies’ findings [2,24]. The rest of the patients had cartilage lesions both adjacent to the labral tear and diffused to other areas. This is suggestive of an association between labral tears and the arthritic process, although it does not establish causality.
In this study, there was only 10% agreement between the observers regarding the articular cartilage grade according to the Outerbridge classification. This can likely be attributed to the visualization difficulty when using the arthroscope in an open dry environment, as well as to the fact that the Outerbridge classification was also developed for assessing patellar cartilage rather than acetabular cartilage [22]. That being said, to the Outerbridge system may slack validity as an acetabular cartilage damage classification system, which results in the lack of agreement between the observers.
A growing body of evidence suggests that the acetabular labrum plays an important role in maintaining normal hip mechanics and that labral pathology is involved in the development and progression of hip arthritis [2,4-8,11,14-19,25]. However, despite our increased understanding of labral pathology, it is still difficult to draw conclusions on the relationship between labral tears and the development of hip OA. Our findings provide important insight into a close relationship between labral tear and end-stage OA. This study’s major strength is that it is the first to examine the labrum in a patient population undergoing THR through the assessment of videos and radiographs by blinded fellowship-trained orthopedic surgeons.
However, this study has several limitations. The main limitation concerns the significant inter-observer variability when describing the labrum pathology according to the Lage classification [21]. This could be attributed to several factors. One factor is related to the difficulty of obtaining adequate videos intraoperatively due to the arthroplasty surgeon’s limited experience using the arthroscope for assessing hip pathology. Second, the Lage system was not designed to classify labral pathology in patients with end-stage OA. Lage et al. [21] arthroscopically assessed labral pathology in 267 hips belonging to patients with a median age of 40 years [21].
Our study’s population had an average age of 67 years and relatively complex labral pathology related to end-stage OA, which was difficult to classify consistently according to the Lage classification. Another major limitation is the study’s low sample size. With only 10 participants, no definite conclusions can be drawn. Nevertheless, the highly narrowed scope of the study should be acknowledged. Lage et al. [21] started their observations of labral pathology with a sample size of 367 hips; the first 100 hips were excluded, as they were considered a learning curve for the observers to gain experience identifying and describing labrum tears. This ensured higher inter-rater reliability. Therefore, it is possible that a sample size large enough to allow for the allocation of some participants for practice may have yielded greater inter-observer agreement in our study. An additional limitation is that key demographic characteristics were not considered in the inclusion/exclusion criteria. Factors such as gender, race, history of physical activity, and body mass index may have a considerable impact on the labrum’s condition in end-stage hip OA. For example, a strong correlation has been found between culture and the location of labral tears: anterior tears are more common in the North American population, whereas posterior tears are more common in Asian populations, primarily due to their different seating habits, which subject the hip to more posterior stress [26]. Finally, even though arthroscopy is considered the gold standard for labral tear viewing, there was some difficulty utilizing the arthroscope to achieve adequate quality for the video recordings without the presence of an arthroscopist during the procedure. To ensure acceptable data quality, the involvement of an arthroscopist and/or the use of different techniques to achieve better viewing of the labrum is highly recommended.
As previously mentioned, this was a pilot study on the labrum in patients with end-stage hip OA. Considerably more research needs to be undertaken. First, a new system for the classification of labral tears in arthritic hips needs to be developed, as there is currently no gold standard for classifying labral tears in end-stage hip OA. Second, larger sample sizes are required for drawing reliable conclusions. Third, the relationship between demographic characteristic sand labral tears should be further examined. Finally, the procedure should be replicated using a variety of imaging equipment to find the best possible way to view labral tears.
Conclusion
Overall, the results of this study suggest a high prevalence of labral pathology in patients undergoing THR for OA. This labral pathology was predominantly found in the anterior-superior quadrant of the hip. Further research is required to substantiate the evidence suggesting a possible causal relationship between labral tears and the development of OA. The use of the Lage classification for the labrum and the Outerbridge classification for cartilage showed poor inter-observer reliability. A novel classification system for degenerative labral tears in end-stage OA hips is required.
References
- Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, et al. (2001) Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res 382: 232-240.
- McCarthy J, Noble P, Aluisio FV, Schuck M, Wright J, et al. (2003) Anatomy, pathologic features, and treatment of acetabular labral tears. Clin Orthop Relat Res 406(1): 38-47.
- Konrath GA, Hamel AJ, Olson SA, Bay B, Sharkey NA (1998) The role of the acetabular labrum and the transverse acetabular ligament in load transmission in the hip. J Bone Joint Surg Am 80(12): 1781-1788.
- Crawford MJ, Dy CJ, Alexander JW, Thompson M, Schroder SJ, et al. (2007) The 2007 Frank Stinchfield Award: the biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res 465: 16-22.
- Ferguson SJ, Bryant JT, Ganz R, Ito K (2000) The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech 33(8): 953-960.
- Ferguson SJ, Bryant JT, Ganz R, Ito K (2000) The acetabular labrum seal: a poroelastic finite element model. Clin Biomech (Bristol, Avon)15(6): 463-468.
- Ferguson SJ, Bryant JT, Ganz R, Ito K (2003) An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech 36(2): 171-178.
- Song Y, Ito H, Kourtis L, Safran MR, Carter DR, et al. (2012) Articular cartilage friction increases in hip joints after the removal of acetabular labrum. J Biomech 45(3): 524-530.
- Groh MM, Herrera J (2009) A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med 2(2): 105-117.
- Kelly BT, Weiland DE, Schenker ML, Philippon MJ (2005) Arthroscopiclabral repair in the hip: surgical technique and review of the literature. Arthroscopy 21(12): 1496-1504.
- Ganz R, Leunig M, Leunig-Ganz K, Harris WH (2008) The etiology of osteoarthritis of the hip. Clin Orthop Relat Res 466(2): 264-272.
- Farjo LA, Glick JM, Sampson TG (1999) Hip arthroscopy for acetabular labral tears. Arthroscopy 15(2): 132-137.
- Fitzgerald RH (1995) Acetabular labrum tears. Diagnosis and treatment. Clin Orthop Relat Res 311: 60-68.
- Altenberg AR (1977) Acetabular labrum tears: a cause of hip pain and degenerative arthritis. South Med J 70(2): 174-175.
- Greaves LL, Gilbart MK, Yung AC, Kozlowski P, Wilson DR (2010) Effect of acetabular labral tears, repair and resection on hip cartilage strain: a 7T MR study. J Biomech 43(5): 858-863.
- Harris WH, Bourne RB, Oh I (1979) Intra-articular acetabular labrum: a possible etiological factor in certain cases of osteoarthritis of the hip. J Bone Joint Surg Am 61(4): 510-514.
- McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J (2001) The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res 393: 25-37.
- Nepple JJ, Carlisle JC, Nunley RM, Clohisy JC (2011) Clinical and radiographic predictors of intra-articular hip disease in arthroscopy. Am J Sports Med 39(2): 296-303.
- Neumann G, Mendicuti AD, Zou KH, Minas T, Coblyn J, et al. (2007) Prevalence of labral tears and cartilage loss in patients with mechanical symptoms of the hip: evaluation using MR arthrography. Osteoarthr Cartil 15(8): 909-917.
- Peelle MW, Della Rocca GJ, Maloney WJ, Curry MC, Clohisy JC (2005) Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res 441: 327-333.
- Lage LA, Patel JV, Villar RN (1996) The acetabular labral tear: an arthroscopic classification. Arthroscopy 12(3): 269-272.
- Outerbridge RE (1964) Further studies on the etiology of chondromalacia patellae. J Bone Joint Surg Br 46: 179-190.
- Byers PD, Contepomi CA, Farkas TA (1970) A post mortem study of the hip joint. Including the prevalence of the features of the right side. Ann Rheum Dis 29(1): 15-31.
- Putz R, Schrank C (1998) Anatomy of the labrocapsular complex of the hip joint. Der Orthopäde 27(10): 675-680.
- Tan V, Seldes RM, Katz MA, Freedhand AM, Klimkiewicz JJ, et al. (2001) Contribution of acetabular labrum to articulating surface area and femoral head coverage in adult hip joints: an anatomic study in cadavera. Am J Orthop (Belle Mead NJ) 30(11): 809-812.
- Mason JB (2001) Acetabular labral tears in the athlete. Clin Sports Med 20(4): 779-790.
© 2020 Ivan Wong. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






