- Submissions
Full Text
Research & Investigations in Sports Medicine
Proprioception: An Evidence Based Narrative Review
Prakash Jha1, Irshad Ahamad2, Sonal Khurana3*, Kamran Ali2, Shalini Verma2 and Tarun kumar4
1Osteon Physiotherapy Clinic, India
2Centre for Physiotherapy and Rehabilitation Sciences, Jamia Millia Islamia, India
3Indian Spinal Injuries Centre, India
44Amar Jyoti Institute of Physiotherapy, University of Delhi, India
*Corresponding author: Sonal Khurana, Department of Rehabilitation, Indian spinal Injuries Centre, Sector-C, Vasant Kunj, New Delhi-110070, India
September 14, 2017; Published: October 17, 2017
ISSN: 2577-1914 Volume1 Issue2
Abstract
Proprioception plays an important role in the complex mechanism of joint control. Proprioceptive training is popularly applied as preventive or rehabilitative exercise method in various sports and rehabilitation settings. The primary purpose of this narrative review is to evaluate the current literature and to provide further insight about proprioception.
The objective is to answer few important questions:
• What are the factors affecting it?
• How to evaluate proprioception?
• What are the tools and technique required for the assessment?
• How to train, improve, and progress in proprioceptive training?
This evidence based study helps to guide rehabilitation professionals in selecting appropriate, effective strategies when managing issues related to position sense.
Keywords: Proprioception; Balance; Receptors; Fall incidence; Joint position sense; Factors influencing; Assessment; Training
Introduction
Charles Sherrington introduced the term ‘proprioception’ in 1906, he describe “the perception of joint and body movement as well as position of the body, or body segments, in space” [1]. Another term coined by Henry Bastian was kinesthesia which refers to “the body of sensation which results from or is directly occasioned by movement’s kinesthesis. By means of this complex of sensory impression we are made acquainted with the position and movements of our limbs by means of it the brain also derives much unconscious guidance in the performance of movement generally”. Both terms are used currently in the field of neurology, neurophysiology, exercise physiology, orthopaedics surgery, sports and exercise medicine. Some researchers define proprioception as joint position sense only and kinaesthesia as conscious awareness of joint movement [2].
Proprioception function is presumably elaborated in three ways as described in the literature. First, the information from the proprioception helps to protect the joint from excessive and injurious movement via reflex mechanism. Second, it gives information about joint stabilization during static posture. Third, it will help in performance coordination of the movement or complex movement in a precise manner [3].
It has been used as a term to indicate sensory perception and subsequent motor control of posture, balance, audio visual-motor coordination and joint stability. With the ability of proprioception individual can learn new motor skills. Proprioceptive abilities are essential for orientation and moving in space and engaging with the environment. So they act like a key element for goal-directed movements of the limbs. Their functions are controlling of aiming accuracy, performance of movement sequences, reaching and tracking movements like grasping and manipulating objects, and the control and correction of ongoing movements. Proprioceptive deficits cause postural control or balance problems, difficulties and insecurity in many activities of daily living. Proprioceptive feedback is important in the control of many upper and lower limb movements [4].
This paper attempts to sum up all clinically significant data which can be utilized by rehabilitation professional as a guide.
Authors tried to answer following questions regarding proprioception:
1. What is the basic concept of proprioception and its receptors?
2. What are the factors which affect proprioception?
3. What are the measures/tools and techniques for assessment of proprioception?
4. How to train and progress the proprioception to increase functional activity for non-athletic and athletic population?
Proprioception and its Receptors
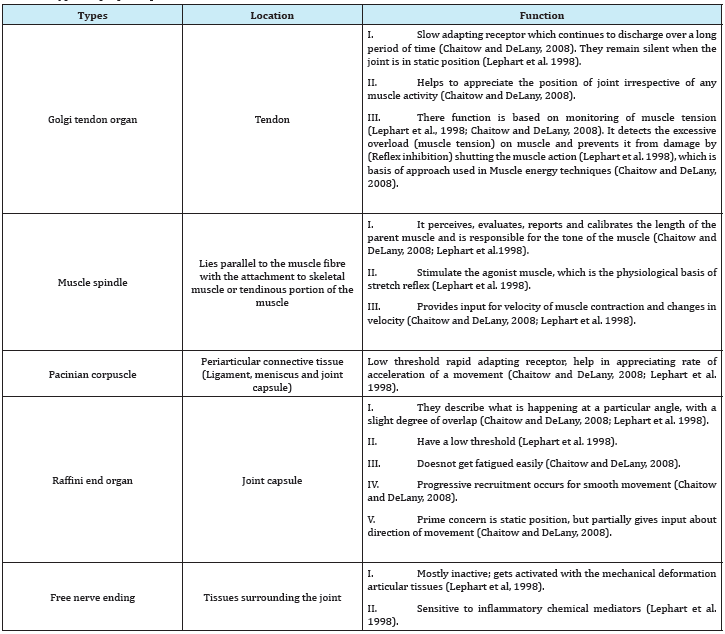
Human body has six exteroceptive human senses that help to detect the outside world (sight, smell, taste, hearing and touch), whereas proprioception provides inputs solely on the status of the internal body (Chaitow and DeLany, 2008). The perception of body or body parts, position or movement dependent on some specific type of receptors, which are located in and around the muscular structure and joint (Corrigan et al. 1992). Different kinds of receptors perform different functions by transferring information to all levels of the central nervous system (Riemann and Lephart, 2002). Accordingly, appropriate motor response chosen during static or dynamic situation of the body or body parts [5]. Thorough understanding of proprioception aids in the clinical practice of physiotherapist, occupational therapist, athletic trainers, sports therapist, orthopedic surgeons and sports medicine experts Table 1.
Table 1: Types of proprioceptors.
Factors Affecting Proprioception
Several evidences exists which focus on factors that induce changes in proprioception in both athletic and non-athletic population in their respective physical activities. In the following sections, we will focus the influence of age, pain, injury, soft tissue tension, regular sports training, warm up etc. Baseline measurement of proprioception is done with sophisticated equipment which guides therapists in order to formulate training program. Proprioceptive training is required accordingly so that the individual can perform their functions optimally.
Osteoarthritis
Old age individuals with or without degenerative joint disease have reduced proprioception (Attfield et al. 1996). This age related reduction is responsible for impaired postural control and increases the risk of fall in geriatric population (Westlake KP, 2007).
Age
Arthritis is a major component in degenerative diseases, which has shown significant proprioceptive deficits in position sense and motion sense when compared with healthy control [6-8]. It has been hypothesized that quadriceps weakness and impaired mechanoreceptors is responsible for the deficits.
Injury and inflammation
Joint receptors, which are damaged due to any degree of articular injury, play an important role in proprioception they have an important role in influencing the gamma motor neuron and supraspinal motor programs (Riemann and Lephart, 2002). A proprioceptive deficit is evident after ligamentous injury around the ankle which is responsible for functional instability following such injury [9,10]. Several studies also found that there is a deficit in the proprioception in patients with ACL deficiency or with meniscal injuries (Corrigan et al. 1992) [11,12]. Inflammatory chemical mediators alter proprioception by stimulating free nerve endings which is specific proprioceptors affected by chemicals (Lephart et al. 1998).
Pain
It is found that there is significant impairment in the proprioceptive accuracy during joint pain [13,14] while some researchers found no association in between proprioception and pain [15,16].
Soft tissue tension
Reloading of lax collateral tissues during the biomechanical adjustment at the time of knee replacement improves proprioception [17]. Soft tissue imbalance is corrected by surgeons in knee replacements so that the collateral structures retain the same amount of tension [18]. Any soft-tissue imbalance still present after total knee replacement affects the position of the resultant force vector through the knee during dynamic activities, which could be perceived proprioceptively as a varus or valgus deviation of the bony alignment (Attfield, 1996). This altered pattern then produce a reflex antagonistic action from the muscles, producing large corrective load applied to the knee replacement. Altered loading pattern may affect the direction of the dynamic force vector through the knee, and move it medially or laterally so that it is applied solely (Attfield, 1996).
Athletic population
Study reported that athletic populations have better proprioception than non-athletic population which was proved by research by comparing the female volley ball athlete to non-athletic females (Sahin, 2015), but some contradictory result was found in ballet dancers with knee joint laxity had reduced proprioception compared with a normal healthy control group [19].
Warm up
5-10 minutes of warm up exercises has positive effect on proprioception and balance, and the duration spend in warm also has positive co-relation with proprioception (Subasi, 2008). FIFA’s 11+ and Harmo Knee warm up program also improves the proprioception at 45 and 60 degree of knee flexion and simultaneous increases static and dynamic balance in male soccer players [20].
Cryotherapy
The number of studies observed an increase in joint position sense error after cryotherapy is similar to the number of studies reporting no changes. Due to the limited number of investigations and the inconsistency of its results, which likely resulted from the methodological differences, the influence of cryotherapy on proprioception is still to be clearly ascertained [21].
Approaches to Measure Proprioception
James McKeen Cattell and Hugo Munsterberg founded pioneer assessment procedure of proprioception and termed it as a psychophysical method of assessing human movement in late 18th century. Afterwards, Charles Sherrington proposed the concept of proprioception, methods of assessing proprioception. Now there are three fundamental approaches or methods to measures proprioception: method of limits, method of adjustment and method of constant stimuli [22].
Method of limits
Describe as the determining the threshold for perception of movement as the level of stimulus (joint angle) is altered (increased and decreased) slowly. Both increasing and decreasing method usually used alternately and the thresholds are averaged [23]. The threshold to detection of passive motion (TTDPM) proprioception technique is one form of the method of limits, where participants are required to detect joint movement under different velocities (Lephart, 2002).
Method of adjustment
Also known as method of average error, evaluates the ability of subject to reproduce level of stimulus (joint angle) at the same level of reference stimulus (joint angle that had been placed before). The difference between the adjustable stimulus and the reference one is recorded as the subject’s error, then average errors is reported [24]. The joint position reproduction (JPR) proprioception test protocol is one form of the method of adjustment, where participants are usually asked to match or reproduce the previously experienced reference joint positions [25].
Method of constant stimuli
Describe as repetitions of different level of stimulus (joint angle) are presented in random order. Then the subject has to determine whether they are able to detect the stimulus (absolute threshold), or subject can make comparison between the constant stimuli at different levels (difference threshold) [21]. The subjects compare two movements, one which have clearly defined start and end positions and other determines which stimulus is greater. Waddington & Adams [25,26] developed the active movement extent discrimination assessment (AMEDA) to test participant`s ability to use proprioceptive information.
Proprioceptive Training
Like other physical fitness component such as endurance, strength and power training; proprioceptive training is also one of the main components. Primary objectives of proprioceptive training or retraining are to train afferent pathways (sensory inputs) to enhance joint movement sense. It works on neuromuscular control system. Various studies concluded that exercise supervised by physiotherapists seems to improve proprioceptive accuracy (both position and motion sense), pain and activity limitations. Positive results were noticed in the proprioceptive accuracy (joint position sense) while performing balance training or proprioceptive exercises in both weight bearing and non-weight bearing positions [27-29]. Other researcher found that weight bearing strengthening exercise resulted in significant improvement on position sense while non-weight bearing strengthening shows not much significant improvement in proprioception accuracy [29]. These types of exercises have positive effects on the muscular strength and endurance, thereby due to increase in the muscle spindle sensitivity [27] or stimulation of the articular mechanoreceptors [27]. Weight bearing exercise result in elevation of the intra-articular pressure; stimulates ruffini nerve endings and therefore improvement in the proprioceptive accuracy [29].
There are different ways to improve proprioception by challenging the individual in different way; they can be used separately or in combination as well. These challenging activities are used for the progression and functional based program [30- 32]. For example for old age population independent walking, stair climbing, walking on uneven surface is a primary function and for athletes running, jumping, agility become a primary function. So for the specific function altering the following challenging activity we are increasing the reliability on proprioceptors to provide functional stability. It can done by reducing the cues (conscious and subconscious), reducing the visual input (eye open to eye closed), reducing the auditory input (putting ear plugs), reducing the base of support (narrow standing, semi tandem position, tandem position, single leg standing), from stable to unstable surface (Foam pad, stability trainer, wobble board: unidirectional to multidirectional, bosu ball, air stability disc etc), altering the vestibular cue by changing the head position (Westlake, 2007).
Another important aspect of training process is fascial proprioception. Congruently, in the proposed fascia training a perceptual refinement of shear, gliding, and tensioning motions in superficial fascial membranes is encouraged [33,34]. In doing this, it is important to limit the filtering function of the reticular formation, as it can markedly restrict the cortical transfer of sensations from movements which are repetitive and which the cerebellum can predict via feed-forward anticipation. In addition to the slow and fast dynamic stretches, as well as utilizing elastic recoil properties, the inclusion of ‘fascial refinement’ elements are recommended, in which varying qualities of movement are experimented with, e.g., extreme slow motion and very quick micro-movements which may not even be visible to an observer, as well as large macro movements involving the whole body [35,36]. To this end, it may then be not uncommon to place the body into unfamiliar positions while working with the awareness of gravity, or possibly through exploring the weight of a training partner (Robert Schleip et al. 2012).
Like other training protocols, neuromuscular control system is also mediated by proprioception at three different levels: reflex at spinal level, brain stem level and motor cortex level.
2) Training involving balance and postural activities with or without visual input, works on brainstem level.
3) Training involving alteration in conscious and unconscious inputs, works on motor cortex level. Hence, any using these principles we can make proprioceptive exercises more challenging in stepwise manner to improve functional stability.
Conclusion
Proprioceptive sense plays a crucial role in education and is based on differences of individual characteristics and activity of daily living. Since proprioceptive re-education is a relatively new rehabilitation concept incorporating these exercises into joint rehabilitation clinics could be a step for clinical basic science work. Our paper summarizes few important aspects of proprioception such as its influencing factors, assessment principles and training guidelines. To the point precise answers of all queries regarding proprioception will help rehabilitation professionals to directly use or replicate them in their rehabilitation protocols. Thus, it could be used as a guide for all rehabilitation professionals in evaluation, assessment, gaining insight of proprioception factors influencing each individual, formulating training protocol and planning appropriate, effective strategies when managing issues related to position sense. Future research on the effect of proprioception training should try to compare more specific samples and clearly define the framework of training.
References
- Sherrington C (1910) The integrative action of the nervous system. CUP Archive.
- Swanik CB, Lephart SM, Rubash HE (2004) Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am 86-A(2): 328-334.
- Knoop J, Steultjens MP, Van der Leeden M, Van der Esch M, Thorstensson CA, et al. (2011) Proprioception in knee osteoarthritis: a narrative review. Osteoarthritis and Cartilage 19(4): 381-388.
- Cigdem Oksuz (2015) Proprioception: The Forgotten Sixth Sense Chapter: Hand and Wrist Problems and Proprioception. OMICS Group eBooks 1-8.
- Era P, Schroll M, Ytting H, Gause-Nilsson I, Heikkinen E, et al. (1996) Postural balance and its sensory motor correlates in 75-year-old men and women: A cross-national comparative study. J Gerontol A Biol Sci Med Sci 51(2): M53 -M63.
- Barrack RL, Skinner HB, Cook SD, Haddad RJ (1983) Effect of articular disease and total knee arthroplasty on knee joint position sense. J Neurophysiol 50(3): 684-687.
- Hassan BS, Mockett S, Doherty M (2001) Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Ann Rheum Dis 60(6): 612-618.
- Koralewicz LM, Engh GA (2000) Comparison of proprioception in arthritic and age-matched normal knees. J Bone Joint Surg Am 82-A(11): 1582-1588.
- Freeman MAR, Dean MRE, Hanham IWF (1965) The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br 47(4): 678-685.
- Glencross D, Thornton L (1981) Position sense following joint injury. J Sports Med Phys Fitness 21(1): 23-27.
- Friden T, Roberts D, Ageberg E, Walden M, Zatterstrom R (2001) Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture. J Orthop Sports Phys Ther 31(10): 567-576.
- Jerosch J, Prymka M (1997) Proprioceptive deficits of the knee joint after rupture of the medial meniscus. Unfallchirurg 100(6): 444-448.
- Felson DT, Gross KD, Nevitt MC, Yang M, Lane NE, et al. (2009) The effects of impaired joint position sense on the development and progression of pain and structural damage in knee osteoarthritis. Arthritis Rheum 61(8): 1070-1076.
- Shakoor N, Furmanov S, Nelson DE, Li Y, Block JA (2008) Pain and its relationship with muscle strength and proprioception in knee OA: results of an 8-week home exercise pilot study. J Musculoskelet Neuronal Interact 8(1): 35-42.
- Bennell KL, Hinman RS, Metcalf BR, Crossley KM, Buchbinder R, et al. (2003) Relationship of knee joint proprioception to pain and disability in individuals with knee osteoarthritis. J Orthop Res 1(5): 792-797.
- Hortobagyi T, Garry J, Holbert D, DeVita P (2004) Aberrations in the control of quadriceps muscle force in patients with knee osteoarthritis. Arthritis Rheum 51(4): 562-569.
- Barrett DS, Cobb AG, Bentley G (1991) Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br 73(1): 53-56.
- Insall JN (1984) Total knee replacement. Surgery of the knee. Churchill Livingstone, New York, USA, 587-695.
- Barrack RL, Skinner HB, Brunet ME, Cook SD (1984) Joint kinesthesia in the highly trained knee. J Sports Med Phys Fitness 24: 18-20.
- Daneshjoo A, Mokhtar AH, Rahnama N, Yusof A (2012) The Effects of Comprehensive Warm-Up Programs on Proprioception, Static and Dynamic Balance on Male Soccer Players. PLoS ONE 7(12): e51568.
- Ribeiro F, Oliveira J (2011) Factors Influencing Proprioception: What do They Reveal? Biomechanics in Applications.
- Adams R, Lee KY, Wadddington G, Lee HJ (2012) The method of constant stimuli in the psychophysics of movement. Proceedings of Fechner Day 28(1): 18-23.
- Gescheider GA (2013) Psychophysics: the fundamentals. Psychology Press.
- Goble DJ (2010) Proprioceptive acuity assessment via joint position matching: from basic science to general practice. Phys Ther 90(8): 1176- 1184.
- Waddington G, Adams R (1999) Ability to discriminate movements at the ankle and knee is joint specific. Percept Mot Skills 89(3 Pt 1): 1037- 1041.
- Lin DH, Lin YF, Chai HM, Han YC, Jan MH (2007) Comparison of proprioceptive functions between computerized proprioception facilitation exercise and closed kinetic chain exercise in patients with knee osteoarthritis. Clin Rheumatol 26(4): 520-528.
- Diracoglu D, Aydin R, Baskent A, Celik A (2005) Effects of kinesthesia and balance exercises in knee osteoarthritis. J Clin Rheumatol 11(6): 303-310.
- Lin DH, Lin CH, Lin YF, Jan MH (2009) Efficacy of 2 non-weightbearing interventions, proprioception training versus strength training, for patients with knee osteoarthritis: a randomized clinical trial. J Orthop Sports Phys Ther 39(6): 450-457.
- Jan MH, Lin CH, Lin YF, Lin JJ, Lin DH (2009) Effects of weight-bearing versus nonweight-bearing exercise on function, walking speed, and position sense in participants with knee osteoarthritis: a randomized controlled trial. Arch Phys Med Rehabil 90(6): 897-904.
- Bastian HC (1887) The “muscular sense”; its nature and cortical localization. Brain 10(1): 1-89.
- Blackburn T, Guskiewicz KM, Petschauer MA, Prentice WE (2000) Balance and joint stability: the relative contributions of proprioception and muscular strength. J Sport Rehabil 9(4): 315-328.
- Ghez C (1991) The control of movement. Principles of Neural Science. (3rd edn), Elsevier Science, New York, USA, PP. 533–547.
- Han J, Waddington G, Adams R, Anson J, Liu, Y (2016) Assessing proprioception: a critical review of methods. Journal of Sport and Health Science 5(1): 80-90.
- Hasan Z, Stuart DG (1988) Animal solutions to problems of movement control: the role of proprioceptors. Annu Rev Neurosci 11: 199-223.
- McCaskey MA, Schuster-Amft C, Wirth B, Suica Z, de Bruin ED (2014) Effects of proprioceptive exercises on pain and function in chronic neckand low back pain rehabilitation: a systematic literature review. BMC Musculoskelet Disord 15: 382.
- Skinner HD, Barrack RL, Cook SD (1984) Age-related decline in proprioception. Clin Orthop 184: 208-211.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






