- Submissions

Full Text
Researches in Arthritis & Bone Study
Evaluation of Leg Length Discrepancy (LLD) after Unilateral Total Knee Arthroplasty (TKA) Done for Varus Knee Deformity
Abanoub Nagaty Gendy1, Ahmed Khalifa A1,2*, Hatem Bakr M1, Yaser Khalifa E1 and Ahmed Abdelaal M1
1Orthopaedic and traumatology department, Assuit University Hospital, Egypt
2Orthopaedic Department, South Valley University, Egypt
*Corresponding author:Ahmed Khalifa A, Orthopaedic Department, South Valley University, Egypt
Submission: November 29, 2019;Published: December 17, 2019
Volume1 Issue5 December 2019
Abstract
Leg Length Discrepancy (LLD) is a major concern in patients undergoing lower limb total joint arthroplasty, it is commonly studied in Total Hip Arthroplasty (THA) literature, however, few studies evaluated this issue in Total Knee Arthroplasty (TKA) patients. In this mini-review, we will mention in brief how to evaluate the LLD associated with LLD as well as reviewing what had been reported about its incidence and the possible effect on clinical outcomes.
Introduction
Varus deformity associated with knee osteoarthritis considered to be the most commonly encountered deformity in patients undergoing Total Knee Arthroplasty (TKA), which is usually associated with varying degrees of medial soft tissue structures contractures, laxity of the lateral soft tissue structures, flexion deformity and medial knee compartment bone erosions [1]. The challenges in performing TKA in a varus arthritic knee include the restoration of mechanical limb alignment after balancing the medial and lateral soft tissue tension by equalizing the flexion and extension gaps [2]. Limb Length Discrepancy (LLD) less than 2cm is usually not noticeable and does not require treatment, however, if the LLD is over 2cm, it is usually noticed by the patients with a tendency to perform a self-compensation mechanism such as walking on the ball of the foot (toe down) or by tilting the pelvis and curving the spine, which eventually may lead to lower back pain, gait abnormalities and even can lead to hip arthritis [3-5]. LLD and its effects on patient function have been discussed in depth in the Total Hip Arthroplasty (THA) literature, although it had been reported with TKA, however, few studies handled this issue with its effects on the clinical outcomes [6,7].
How to assess LLD associated with TKA
Clinically: Apparent or functional leg length (which can be affected due to other causes rather than the TKA such as pelvis or spine problems) can be measured using measuring tape from a fixed point (usually the umbilicus) to a point represented bilaterally in both limb (usually the medial malleolus) [5,8,9], while the true or the anatomical leg length (which represents the actual bony length of the lower limb) can be measured from a separate points on each limb independently (which usually the anterior superior iliac spine “ASIS” proximally and the medial malleolus distally)
Radiologically: Using a full-length (hip to ankle) standing anteroposterior (AP) radiographs of the bilateral lower extremities as a routine during pre- and postoperative evaluation of TKA patients [10-12]. A marker is used to digitally scale the radiograph and the functional length is performed by measuring the distance from the center of the head to a point located at the center of the tibial plafond (Figure 1A) for both sides, while to determine the anatomical length of the limb, the femur and the tibia are measured separately. Anatomical length of the femur is determined by the length of a line connecting the center of the femoral head to the center of the roof of the intercondylar notch (Figure 1B), while the anatomical length of the tibia is determined by the length of a line connecting the center of the tibial plateau to the base of the tibial plafond (Figure 1C). Obtaining these measurements can guide the surgeon to detect if there is a pre- or post TKA LLD, and if present, it will determine its source (Figure 2).
Figure 1:Preoperative radiological measurement
of leg length of both lower limbs on long film AP
radiograph.
A. Functional length of both limbs.
B. Anatomical length of the femur.
C. Anatomical length of the tibia.
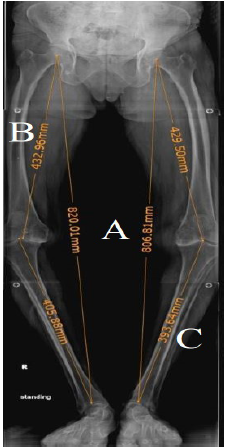
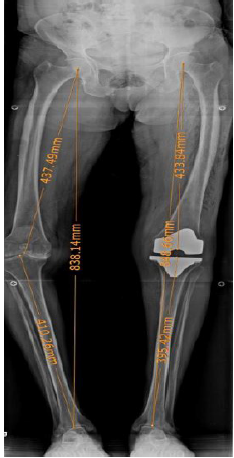
Figure 2:Postoperative long film AP radiograph showing the LLD between the operated and nonoperated limb after TKA.
Will the LLD after TKA affect the clinical outcomes
As we mentioned earlier that the data regarding the effect of
LLD on patients having THA is huge but deficient regarding its
incidence and secondary effect in the case of patients having TKA,
however, few studies discussed this issue. Lang et al. [3] in their
study in 2010 on 102 knees performed over a period of seven
months, they found that 85 (83.3%) knees showed increase in the
limb length after TKA and the average lengthening was 6.3mm (SD:
6.85mm; range, -11.0 to 24.0mm), however, they didn’t correlate
this LLD with patients clinical outcomes. A study by Vaidya et al.
[13] who reported that LLD after unilateral, not bilateral TKA
done for varus knees with osteoarthritis significantly affected the
functional outcomes. However, they also noted that 83.3% of the
patients in the unilateral group and 46.6% in the bilateral group
had LLD. Another study by Tipton et al. [14] in 2015 including
203 patients underwent TKA, 59.1% of the patients included in
this study experienced an increase in limb length with an average
increase of 0.438cm.
The authors didn’t report on the clinical outcomes as well
as the previous study. A recent study by Kim et al. [15] including
148 patients reviewed retrospectively which was divided into two
groups with one group including Eighty-one knees having a <15mm
LLD, and the other group including 67 knees found to have more
than a 15mm LLD, they evaluated the radiographic outcomes,
clinical outcomes, patients satisfaction, and perception of LLD
were also evaluated. They found a significant difference in the Knee
Society function score and the score for the difficulty with ascending
the stairs in the Western Ontario and McMaster Universities score
between both groups, however, there was no difference in the
results of their satisfaction questionnaires. They concluded that the
functional outcomes of more than 15mm post-operative LLD after
TKA were lower than those of the <15mm LLD. Thus, the reduced
post-operative LLD should be considered to improve the functional
outcomes of primary TKA.
Conclusion
Although not much studied, LLD related to TKA can occur and surgeons should keep it into account while performing TKA. More studies should be performed to assess the incidence of LLD following TKA as well as its effect on clinical as well as radiological outcomes and if it has any impact on implant survival and rate of revision.
References
- Mihalko WM, Saleh KJ, Krackow KA, Whiteside LA (2009) Soft tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg 17(12): 766-774.
- Mullaji, Arun B, Shetty, Gautam (2014) Deformity correction in total knee arthroplasty. Asian Heart Institute and Research Center, India.
- Lang JE, Scott RD, Lonner JH, Bono JV, Hunter DJ, et al. (2012) Magnitude of limb lengthening after primary total knee arthroplasty. J Arthroplasty 27(3): 341-346.
- Khalifa AA (2017) Leg length discrepancy: Assessment and secondary effects. Ortho & Rheum Open Access 6(1): 001-005.
- Clark CR, Huddleston HD, Schoch EP, Thomas BJ (2006) Leg-length discrepancy after total hip arthroplasty. J Am Acad Orthop Surg 14(1): 38-45.
- Konyves A, Bannister G (2005) The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br 87(2): 155-157.
- Edeen J, Sharkey P, Alexander AH (1995) Clinical significance of leg-length inequality after total hip arthroplasty. Am J Orthop (Belle Mead NJ) 24(4): 347-351.
- McCaw S, Bates B (1991) Biomechanical implications of mild leg length inequality. Br J Sports Med 25(1): 10-13.
- Beard D, Andrew JG, Jeya P, John FN (2008) Incidence and effect of leg length discrepancy following total hip arthroplasty. Physiotherapy 94(2): 91-96.
- Murray KJ, Azari MF (2015) Leg length discrepancy and osteoarthritis in the knee, hip and lumbar spine. J Can Chiropr Assoc 59(3): 226-237.
- Sabharwal S, Kumar A (2008) Methods for assessing leg length discrepancy. Clin Orthop Relat Res 466(12): 2910-2922.
- Harvey WF, Yang M, Cooke TD, Segal NA, Lane N, et al. (2010) Association of leg-length inequality with knee osteoarthritis: A cohort study. Ann Intern Med 152(5): 287-295.
- Vaidya SV, Patel MR, Panghate AN, Rathod PA (2010) Total knee arthroplasty: Limb length discrepancy and functional outcome. Indian J Orthop 44(3): 300-307.
- Tipton S, Sutherland, Schwarzkopf R (2015) Change in limb length after total knee arthroplasty. Geriatr Orthop Surg Rehabil 6(3): 197-201.
- Kim SH, Rhee SM, Lim JW, Lee HJ (2016) The effect of leg length discrepancy on clinical outcome after TKA and identification of possible risk factors. Knee Surg Sports Traumatol Arthrosc 24(8): 2678-2685.
© 2019 Ahmed Khalifa A. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






