- Submissions

Full Text
Researches in Arthritis & Bone Study
Rheumatoid Arthritis in the Cervical Spine
Tanaka M*, Fujiwara Y, Uotani K and Yamauchi T
Department of Orthopaedic Surgery, Okayama Rosai Hospital, Japan
*Corresponding author:Tanaka M, Department of Orthopaedic Surgery, Okayama Rosai Hospital, Japan
Submission: June 27, 2019;Published: July 05, 2019
Volume1 Issue4 July 2019
Abstract
1. Abstract
Rheumatoid Arthritis (RA) is a chronic, systematic, and progressive autoimmune disorder. More than two-thirds of all RA patients show symptomatic cervical spine lesions. RA in the cervical spine is categorized into three types: Atlantoaxial Subluxation (AAS), Vertical Subluxation (VS), and Sub axial Subluxation (SS). For the diagnosis of RA, plain radiographs are the basis of radiographic evaluation. Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) are important for the further examination. The significantly better results can be achieved with surgical treatment than with conservative treatment. However, the Indications for transoral decompression are limited. For most of the condition, the posterior atlantoaxial fixation can achieve a good result.
2. Keywords: Rheumatoid Arthritis; cervical spine; radiographs; surgical treatment
Introduction
Rheumatoid Arthritis (RA) is a chronic, systematic, and progressive autoimmune disorder, with an incidence of 1-3% [1]. This condition can occur at any age, especially during the fourth or fifth decade of life. The most common sites are the metacarpophalangeal and metatarsophalangeal joints (Figure 1). More than two-thirds of all RA patients show symptomatic cervical spine lesions [2,3], but the lumbar spine is rarely involved. The inflammation in RA causes synovitis, then loosening of the ligaments and capsules, and finally bony erosion, vertebral collapse, and subluxation.
Figure 1:

Clinical presentation
RA in the cervical spine is categorized into three types: atlantoaxial subluxation (AAS), Vertical Subluxation (VS), and Sub axial Subluxation (SS).
Atlantoaxial subluxation (AAS)
Rheumatoid synovitis at the atlantoaxial joints and around the stabilizing transverse, alar and apical ligaments leads to atlantoaxial instability. Disintegration of the transverse ligament causes anterior AAS. The reported prevalence of anterior AAS was 10-55% [4,5]. Compression of the cervical cord is usually from posteriorly, leading to demyelination of the posterior fascicle. Posterior AAS is less frequent (less than 1%) due to odontoid destruction or fracture [6].
Vertical subluxation
Destruction of the lateral atlantoaxial joint leads to joint depression and upward movement of the axis. Pathologically, this destruction spreads to the occipitoaxial joint [7].
Sub axial subluxation
Destruction of the sub axial joints and dysfunction of the posterior ligaments leads to SS. Common sites are C4/5 and C5/6. The prevalence of SAS is 13% among all RA patients [8]. This condition is associated with AAS and onset is usually late.
Plain radiography
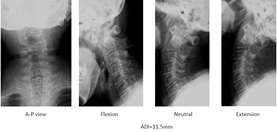
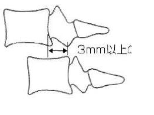
Plain radiographs are the basis of radiographic evaluation for RA in routine screening of the wider population. Anterior AAS may be assessed on a lateral cervical spine radiograph by measuring the Anterior Atlantoaxial Interval (AADI) from the middorsal margin of the anterior ring of C1 to the ventral surface of the odontoid (Figure 2). AADI more than 3mm in an adult or 4mm in a child is considered abnormal [9] (Figure 3). The interval is accentuated on a flexion view if the AAS is present. Posterior AAS may be assessed by measuring the Posterior Atlantoaxial Interval (PADI) from the dorsal aspect of the odontoid to the ventral margin of the C1 lamina.
Figure 2:Atlantoaxial subluxation (AAS).

Figure 3:Radiologic evaluation (Anterior subluxation).

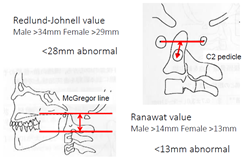
VS can be measured by McRae’s line, Chamberlin’s line or McGregor’s line (Figure 4). McRae’s line connects the front and back of the foramen magnum. If the odontoid process exceeds this line, this condition is regarded as VS. Chamberlin’s line connects the dorsal margin of the hard palate to the dorsal margin of the foramen magnum. If the tip of the odontoid projects more than 6mm, this condition is also regarded as VS. On the other hand, McGregor’s line is easier to use, as it is drawn from the posterior margin of the hard palate to the most caudal point of the occiput. The tip of the odontoid should not project more than 4.5mm.
Figure 4:76 Women, RA, Anterior atlantoaxial subluxation.
The tip of the odontoid is sometimes difficult to identify because of erosion. In such situations, the Redlund-Johnnell [10] method and Ranawat [11] method are very useful to diagnose VS. The Redlund-Johnnell [10] value is measured as the distance between McGregor’s line and the vertebral body of the axis (Figure 4). A value less than 34mm in men and less than 29mm in women is defined as VS. Ranawat value is measured as the distance between McGregor’s line and the center of the C2 pedicle. A value less than 15mm in men and less than 13mm in women is defined as VS (Figure 5 & 6).
Figure 5:Redlund Johnell method.
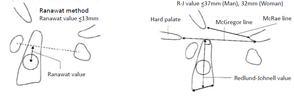
Figure 6:Radiologic evaluation (Vertical subluxation).
SAS is defined as a slip of more than 3mm in the sub axial vertebra (Figure 7). For RA patients, the lack of osteophyte formation represents a unique feature compared with OA patients (Figure 8). The Space Available for the Cord (SAC) is related to the onset of myelopathy and surgical results [12]. RA patients need to hyper-flex the neck during meals because of ROM (Range of Motion) disturbance of the upper extremities (Figure 9).
Figure 7:79 Women, RA, Vertical subluxation.

Figure 8:79 Women, RA, Vertical subluxation, CT.
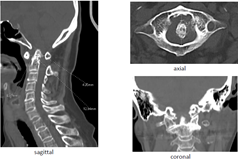
Figure 9:Sub axial Subluxation (SAS).
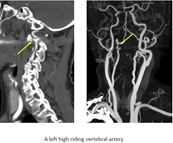
Computed tomography (CT)
CT is preferred for evaluating bony destruction and ruling out anatomical anomalies. Multiplanar Reconstruction (MPR) provides a three-dimensional evaluation of the cervical spine. Sagittal reconstruction images allow clear visualization of AADI, odontoid erosion, and high-riding vertebral artery (Figures 10-13).
Figure 10:71 Women, RA, Sub axial subluxation.
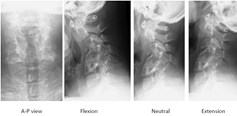
Figure 11:67 Women, RA, Subaxial subluxation.

Figure 12:76 Women, RA.
Figure 13:74 Women, RA.

Magnetic resonance imaging (MRI)
As plain radiograms cannot evaluate soft tissues, MRI is very important to assess pannus, cord compression, myelomalacia, and soft tissue (Figures 14-17). MRI in flexion is used to check compression of the spinal cord in AAAS patients [13]. MRI can be used to evaluate the corticomedullary angle. An angle less than 135° is correlated with neurological compression of the medulla [14]. Magnetic resonance angiography reveals a vertebral artery abnormality in 34% of RA patients [15].
Figure 14:Acetabular
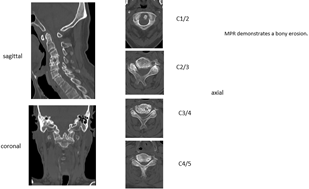
Figure 15:75 Woman, RA.
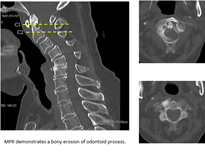
Figure 16:75 Woman, RA.

Figure 17:75 Woman, RA.

Natural history
The prevalence of cervical subluxation in RA patients is 43-86% [16]. The most common form of subluxation is AAAS. Fujiwara et al. identified AAAS in 31% of RA patients, and reducible AAAS progresses to irreducible AAAS, then to VS (Figure 18) [14]. Approximately 20% of subluxations in RA patients involve VS. Neurological deficits are reported in only 7-58% of RA patients [17,18]. Once paralysis develops, the natural history seems to be one of progressive neurological deterioration. Sudden death occurs in as many as 10% of RA patients due to medullary compression [16].
Figure 18:79 Women, RA.

Symptoms
Local symptoms: Neck pain from RA is very common and is caused by inflammation present in the joint when the disease is active. Pain at rest indicates inflammation, but pain during motion indicates instability of the joint.
3.9.2. Neurological deficit: Neurological examinations may be difficult to interpret in RA patients, as subtle neurological changes may be masked. Manual muscle testing is difficult to perform in patients with multiple joint destruction. Peripheral nerve entrapment syndrome modifies the neurological status. Deep tendon reflex is relatively useful to evaluate myelopathy, even in patients with multiple joint destruction. VS patients may show symptoms of medullary compression or lower cranial nerve symptoms.
Vertebral Artery (VA) insufficiency syndrome: VA insufficiency syndrome may occur in patients with AAAS, especially rotatory subluxation. These patients complain of vertigo, tinnitus, nausea, vomiting, and faintness during neck motion. Approximately 20% of RA patients experience occlusion of a VA [19].
3.9.4. General symptoms: RA patients typically complain of fatigue before other symptoms become obvious. Morning stiffness is often an early sign of RA, followed by joint pain, joint swelling, and loss of joint range of motion. When accompanied by other symptoms, low-grade fever can also be a symptom of RA.
Non-surgical treatment: Marks reported significantly better results can be achieved with surgical treatment than with conservative treatment [20]. Among RA patients with myelopathy who refuse surgical treatment, 76% become bedridden within 3 years, and mean survival is 2.3 years [21]. Mainstay nonsurgical treatments for PA patients are physical therapy, patient education, and medication. Non-steroidal anti-inflammatory drugs, steroids, and new immune-modulatory biologic medications are the cornerstones of pharmacotherapy for RA.
Initial pharmacological therapy typically includes methotrexate at 7.5-15mg/week. Corticosteroids are powerful drugs useful for achieving rapid relief from pain. A soft or hard collar can be used to limit anterior subluxation and improve discomfort.
Surgical treatment: Surgery is indicated for RA patients with intractable pain or progressive neurological deficits. The goals of surgery include pain relief, neurological decompression, and prevention of further neurological deterioration. Some patients require awake intubation because of severe cervical cord compression. Preoperative skeletal traction with a halo ring or halo jacket should be considered for patients with severe myelopathy (Figure 19). Somatosensory and motor-evoked potentials are important for monitoring spinal cord function during positioning and surgery.
Figure 19:67 Woman, RA.
Transoral odontoidectomy: Indications for this technique are limited, because RA patients can experience difficulty opening the mouth completely due to temporomandibular joint disturbances. A distance of at least 25mm between the front teeth is needed for this procedure. As RA patients already have some degree of immunodeficiency, surgical-site infection may be another problem associated with this procedure [22] (Figure 20).
Figure 20:79 Women, RA.

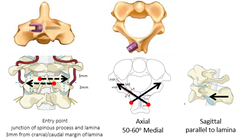
Posterior atlantoaxial fixation: In AAS patients, an AADI of 9mm or more, a SAC of less than 14 mm, or vertebral artery insufficiency are candidates for atlantoaxial arthrodesis surgery [23]. In the historical background, this technique was described Gallie [24] and Brooks & Jenkins [25] (Figures 21 & 22). C2 laminar screw and C1 lateral mass screw fixation, regarded as the Wright technique, is also a safer than Magerl [26] method (Figures 23 & 24). Three famous methods are available to put screws into the C1 lateral mass; Goel, Tan, and Notch methods (Figures 25 & 26). A disadvantage of these techniques is a high rate of nonunion due to reduced stability [27]. Magerl [28] reported trans-articular screw fixation, as the strongest anchor for the upper cervical spine (Figures 27 & 28). However, this procedure has a potential for VA injury in the presence of a high-riding VA [29,30] (Figure 29). Goel reported safer, more rigid fixation using a C1 lateral mass screw and C2 pedicle screw [31] (Figures 30-32). The most important advantage of this technique is that after placement of four screws, AAS can be reduced using screws and rods.
Figure 21:60 Men, RA.
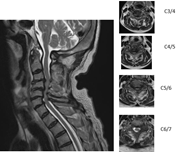
Figure 22:76 Woman, RA.

Figure 23:67 Woman, RA.
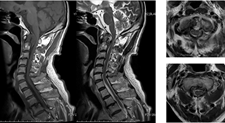
Figure 24:

Figure 25:

Figure 26:Transoral adenoidectomy.
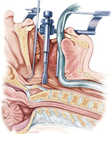
Figure 27:Gallie fusion.
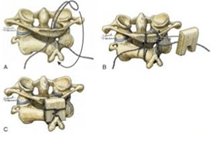
Figure 28:Brooks-Jenkins Fusion.
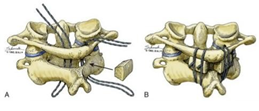
Figure 29: C2 laminar screw (Wright 2004).
Posterior occiput cervical fusion: This technique is mainly indicated for patients with irreducible AAAS and VS. For VS patients, odontoid migration cranial to McGregor’s line of at least 5mm or an abnormal Redlund-Johnnell [10] or Ranawat [11] value are indications for occipitoaxial (OC2) fusion surgery [32]. A major complication for this procedure is dysphagia (Figures 33-36), so OC2 angle should be considered before surgery. An angle of approximately 20° is ideal for OC2 fusion [33]. The navigation is very useful for identifying the thickest part of the occiput and screwing pedicle screws into the cervical spine [34] (Figures 37-44).
Figure 30:52 Men, RA, AAAS, Wright method.
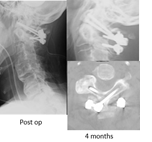
Figure 31:Three methods of C1 LMS placement.

Figure 32:C1 LMS technique.
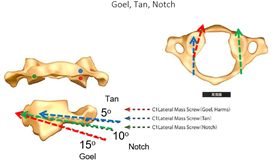
Figure 33:C1/2 transarticular screw (Magerl 1987).

Figure 34:62 Woman, RA, AAAS, Magerl fixation.
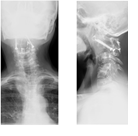
Figure 35:Iatrogenic VA Injury with Magerl Fixation.
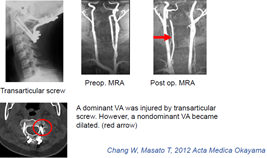
Figure 36:Goel method (C1 LMS & C2 Pedicle screw).
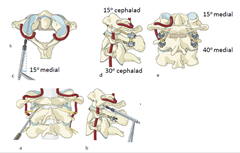
Figure 37:73 Woman, RA, AAAS, Goel fixation.

Figure 38:C2 pedicle screw
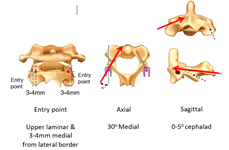
Figure 39:C2 pars screw (Judet 1962).

Figure 40:Dysphagia after OC2 Fusion.
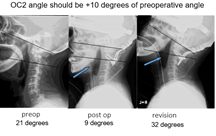
Figure 41:75 Woman, RA, AAAS.
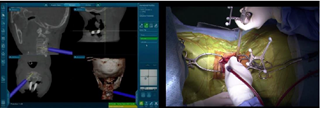
Figure 42:75 Woman, RA, AAAS.
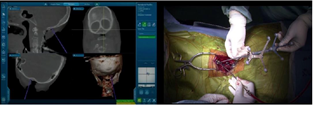
Figure 43:75 Woman, RA, AAAS.
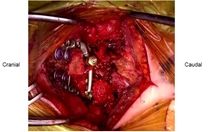
Figure 44:75 Woman, RA, AAAS.

Conclusion
The goal in management of RA cervical spine lesion is to prevent severe neurological deficit. The early diagnosis is very important because myelopathy is masked with peripheral joint problems. Among several imaging, the lateral flexion radiogram and MRI are very useful to diagnose cervical subluxation. For the surgery, the posterior fixation with instrumentation is the standard treatment. However, the surgeon should be reminded several severe complications. When the solid bony fusion is obtained, the pain relief and neurological recovery of the RA patient are expected.
References
20. Marks JS, Sharp J (1981) Rheumatoid cervical myelopathy. Q J Med 50(199): 307-319.
24. Gallie WE (1939) Fractures and dislocations of cervical spine. Amj Surg 46(3): 495-499.
26. Wright NM, Lauryssen C (1998) Techniques of posterior C1-C2 stabilization. Tech in Neurosurg 4: 286-297.
28. Grob D, Magerl F (1987) Surgical stabilization of C1 and C2 fractures. Orthopade 16(1): 46-54.
© 2019 Tanaka M. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






