- Submissions

Full Text
Researches in Arthritis & Bone Study
Simultaneous Oblique Lumbar Interbody Fusion (OLIF) and Lateral Percutaneous Pedicle Screw Fixation (Lateral PPS): A Technical Note
Tanaka M*, Ruparel S, Fujiwara Y, Uotani K and Yamauchi T
Department of Orthopaedic Surgery, Japan
*Corresponding author: Tanaka M, Department of Orthopaedic Surgery, Japan
Submission: January 16, 2019;Published: February 04, 2019
Volume1 Issue4February,2019
Abstract
Purpose: Due to its distinct advantages, lateral approach to the lumbar spine with insertion of percutaneous pedicle screws is increasingly used to treat lumbar degenerative pathologies. We describe a novel technique of simultaneous Oblique Lumbar Interbody Fusion [OLIF] and Percutaneous Pedicle Screw [PPS] insertion in single lateral position with O-arm based navigation system. To the best of our knowledge, this technique has not yet been described in the literature.
Methods: The authors report clinical and radiological results of a 73-year-old lady treated for degenerative lumbar pathology. The authors performed C-arm free OLIF and PPS in single lateral decubitus position simultaneously and describe the technique in detail.
Result: The patient was successfully relieved of her pre-operative symptoms with no neurological sequelae. At 18 months follow up, she maintained good sagittal alignment and balance.
Conclusion: Simultaneous insertion of OLIF cage and PPS in lateral position is possible with O-arm based navigation technique. This significantly reduces operating time and radiation exposure without compromising the results.
Keywords: Navigation surgery; Lateral lumbar; Interbody fusion; O-arm; Percutaneous pedicle screw; C arm free
Introduction
Spinal fusions are usually done with conventional open posterior techniques. With the advent of Minimally Invasive Spine Surgery [MISS]; these are increasingly being used to serve the purpose [1,2]. Better understanding of spinal anatomy; excellent retraction devices and visualization of anatomical structures have made Lateral Lumbar Interbody Fusion [LLIF] technique increasingly popular [3]. This technique though has distinct advantages; needs intra-operative change of patient position from lateral to prone i.e. a two staged procedure. This significantly increases the operating time for the patient. Similarly; insertion of pedicle screws with percutaneous techniques has become possible with computer assisted spinal surgery. These systems have three dimensional [3D] guidance necessary in MISS [4-6].
Amongst these; O-arm and Stealth system [Medtronic Inc. Minneapolis; MN] is used at our centre for its excellent accuracy and automated registration [7]. Traditional C-arm based percutaneous insertion of pedicle screws have the disadvantage of radiation exposure to the operating surgeons. To overcome these shortfalls; the authors hereby report a new technique of simultaneous Oblique Lumbar Interbody Fusion [OLIF] without C-arm fluoroscopy [C-arm free OLIF] and lateral percutaneous pedicle screw [PPS] insertion in a single lateral decubitus position. We believe this technique greatly reduces the operating time and radiation exposure without losing its accuracy and efficacy [8].
Operative Technique
Preoperative planning
Preoperative planning is necessary to check the anatomy of lumbar spine and surrounding soft tissues like the position of psoas muscles; anterior vasculature anomalies; location of lumbar nerve plexus and kidneys on radiological imaging. Severe adhesions due to previous abdominal surgery is a contraindication for OLIF [9].
Patient positioning
The patient is positioned in right lateral decubitus position on a breaking Jackson’s frame. This enables intra operative imaging with O-arm (Figure 1). The table should break approximately with 20 degrees of convexity. An axillary roll is inserted to protect the neurovascular structures in the axilla and the arms are positioned away from the abdomen. The patient should be preferably positioned to the back end of the table; which allows for simultaneous insertion of percutaneous pedicle screws (Figure 2). This feasibility and space for insertion of pedicle screws should be checked pre-operatively. Legs are slightly flexed for relaxation of psoas muscles and lumbar nerve plexus. The patient is secured to the Jackson table with tapes.
Figure 1:Patient positioning, the patient is positioned in the right lateral decubitus position on a breaking Jackson frame.

Figure 2:True lateral decubitus position. The table should be break approximately 20 degrees in a convex way to make lumbar spine no scoliosis.
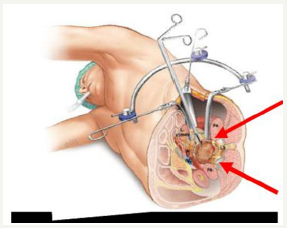
Simultaneous OLIF and lateral Percutaneous Pedicle Screws [PPS]
Step 1: Bone graft harvest: Bone graft is harvested from posterior iliac crest by the first assisting surgeon. After acquisition of adequate bone graft; percutaneous reference frame is anchored to the posterior superior iliac spine through the same incision. The O-arm is positioned, and 3D reconstructed images are obtained. These images are acquired by the Stealth station navigation system [Spine 7R Medtronic; Memphis; USA]. Though neuromonitoring is not necessary for OLIF surgery; we routinely use it in our practice to prevent neurological complications.
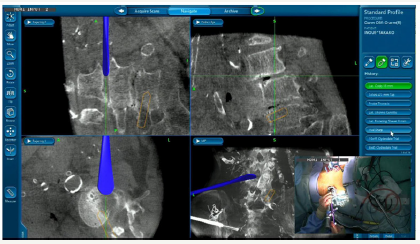
Step 2a: Cranial PPS: After verification of all navigated instruments; skin incision is localized with a navigated probe. Through a 2cm incision; PPS are inserted on either side into the cranial vertebra [L3] with the help of navigated instruments by the first assisting surgeon (Figure 3). These screws are inserted before the insertion of the intervertebral cage. This is because cage insertion changes the alignment of cranially located vertebra and reduces navigational accuracy.
Figure 3:Lateral PPS. PPSs are inserted in the lateral decubitus position using navigated instruments by the first assistant.

Step 2b: Cranial OLIF: The main surgeon simultaneously proceeds with OLIF cage insertion along with Step 2a. The navigated probe helps to centre the 4cm left oblique skin incision. The fibres of external oblique; internal oblique and transversus abdominis muscles are split during exposure (Figure 4). The navigated first Direct Lateral Dilator is placed anterior to psoas at the cranial disc space level [L3-4]. After safe passage of first dilator; sequential dilation is performed until a 22mm tubular retractor can be placed. The retractor assembly is attached to a table mounted flexible arm. Discectomy is then performed (Figure 5) using a bayoneted knife; navigated curette and a navigated Cobb’s retractor (Figure 6). The disc space is distracted with navigated trials. After attainment of adequate disc height; OLIF cage filled with bone graft [or Hydroxyapatite] is gently placed under navigation guidance.
Figure 4:Abdominal muscle dissection. The external, internal and transverse abdominal muscles are divided along muscle fibers by the main surgeon.
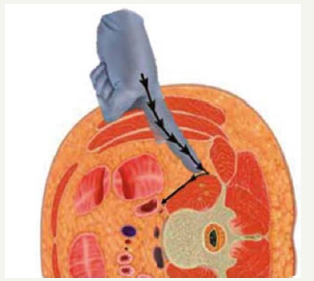
Figure 5:Simultaneous OLIF and lateral PPS. The retractor assembly is attached to the flexible arm and then a discectomy by the main surgeon and the PPS is continuing by the first assistant.
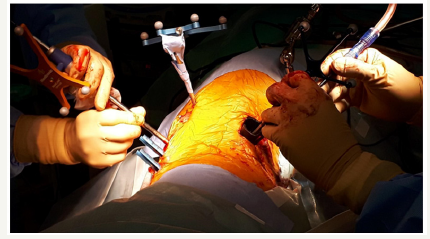
Figure 6:The navigated cobb. The navigated Cobbs is passed along both end plates to contralateral annulus with a mallet.
Step 3a: Intermediate PPS: After accurate placement of cranial OLIF cage [L3-4]; the first assistant surgeon proceeds with insertion of intermediate [L4] PPS in the same manner as the cranial PPS [L3] described above (Figure 7,8).
Figure 7:The navigated trial. The disc space is distracted with navigated trials until adequate disc space height is obtained.
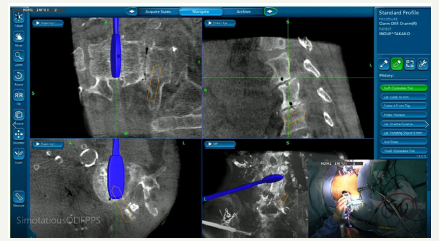
Figure 8:The OLIF cage. Once trialing is complete, a mallet is then used to gently insert the OLIF cage while monitoring placement under navigation guidance.

Step 3b: Caudal OLIF: Along with insertion of intermediate PPS; caudal OLIF cage [L4-5] is inserted by the primary surgeon under navigation guidance.
Step 4a: Caudal PPS: The caudal PPS [L5] are then inserted after placement of caudal OLIF cage (Figure 9,10).
Figure 9:The navigated pedicle probe. The navigated awl is used to make the screw pass way and measure the length and the diameter of screws.
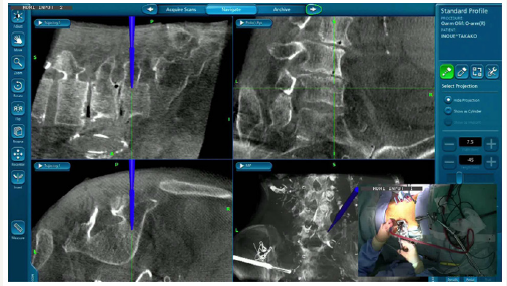
Figure 10:The navigated tap. The navigated tap is inserted into the previous pass way. After tapping, percutaneous pedicle screws are inserted without C-arm.
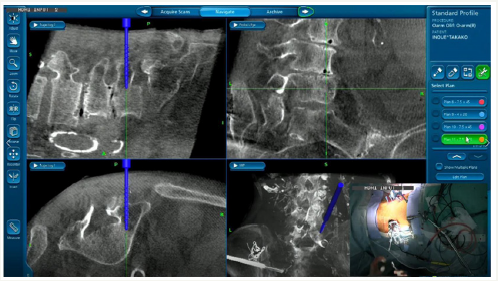
Step 4b: Skin closure: The main surgeon simultaneously closes the lateral skin incision while the caudal PPS are inserted.
Step 5: Insertion of rods: Insertion of percutaneous rods bilaterally is then performed in a standard fashion simultaneously by both surgeons without fluoroscopic guidance. After confirmation of rod position; compression force is applied to secure the bony fusion and generate good lumbar lordosis. Finally; all set screws are tightened to manufactured setting. The posterior skin incisions are closed after satisfactory placement of implants confirmed with radiograms.
Case Presentation
Patient history
A 73-year-old lady was referred to our Hospital with complaints of severe low back pain and intermittent claudication for 6 months. She also complained of numbness and weakness of both lower limbs.
Physical examination
Her claudication distance was 100 meters. Her spine range of motion was limited. Neurological examination was essentially normal.
Pre-operative imaging
Figure 11:Preoperative lumbar imaging. Anteroposterior view
A. Lateral neutral position: There was grade I spondylolisthesis at L3 and 4 level
B. T2 weighted midsagittal MRI: Preoperative MRI revealed severe destruction of both endplates

Radiographs revealed Grade 1 L3-4 degenerative spondylolisthesis with moderate instability at L3-4 and L4-5 levels. Magnetic Resonance Imaging showed canal stenosis at these levels with destruction of endplates (Figure 11).
Surgery
Operative time was 1 hour and 30 minutes. Estimated blood loss was 150 ml. The neurological status was intact post operatively with no known complications.
Follow up imaging
The patient returned to full activity at 1-month post op. The post-operative radiographs and Computed Tomography [CT] scans demonstrate good correction of sagittal alignment (Figure 12,13). At 18 months follow up; patient maintains good sagittal and coronal balance with no neurological sequelae or symptoms.
Figure 12:Final follow up radiograms
A. Anteroposterior view: The lumbar alignment is reduced
B. Lateral neutral position: The spondylolisthesis is reduced, and a good lumbar lordosis is obtained
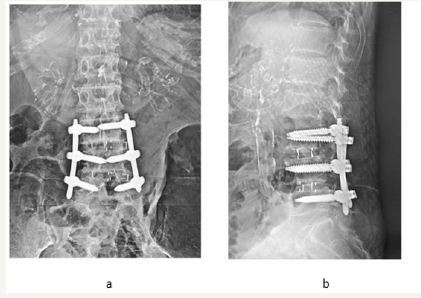
Figure 13:Final follow up CT.
A. Coronal image: Pedicle screws are inserted correctively
B. Sagittal image: A solid bony fusion is obtained
C. L3 axial image
D. L4 axial image
E. L5 axial image

Discussion
The trans-psoas minimally invasive LLIF [XLIFR] has become extremely popular due to its distinct advantages of decreased blood loss and post-operative pain [10-12]. However; this procedure may injure the psoas muscles and lumbar plexus within it; thus, requiring neuromonitoring [13]. With the aim to reduce these complications; OLIF procedure came into vogue [14]. Similarly; OLIF requires supplementation with pedicle screws. These screws are preferably inserted through percutaneous techniques. Thus; this procedure has two distinct disadvantages. First; change of patient position from lateral to prone greatly increases the operating time. Second is the radiation exposure [15]. To overcome these disadvantages; we came with a novel technique for simultaneous OLIF and PPS in lateral position with help of O-arm based navigation guidance system. Similar studies with simultaneous LLIF and PPS have been recently reported [16-18] in the literature with good results.
On comparing the accuracy of O-arm based navigation technique with pre-operative CT based navigation and fluoroscopic techniques for insertion of PPS; O-arm based techniques demonstrated better accuracy [4,5]. Accuracy is particularly important for insertion of PPS; since the pedicle breach cannot be confirmed by probe as in open techniques [6]. Similarly; with C-arm fluoroscopy the pedicle shadows of obese and osteoporotic patient are often difficult to visualize [19]. Thus, in addition to reducing the operating time; this C-arm free technique has numerous additional advantages than conventional OLIF and PPS. The first amongst these is better accuracy rate for PPS insertion. The second advantage is its potential to reduce radiation exposure to the surgeon and operating staff. This is particularly important at centres performing large number of MIS procedures. Numerous studies in the literature have documented harmful effects of radiation [20,21]. With C-arm based PPS insertion techniques; the surgeon is unable to confirm the bony landmarks. This is taken care of by the real time navigated instruments.
Radiation has been notorious in induction of cancers [8] and attempts to reduce radiation to the operating team must be taken into consideration. There have been studies in the literature [4,5] suggesting the use of C-arm fluoroscopy during cage and rod insertion steps in addition to O-arm. In the technique described above; C-arm is not required during these stages; thus, further reducing radiation. However; radiation exposure to the patient also needs to be considered. It has been suggested that each O-arm 3D scan has 60% radiation exposure of an ordinary CT scan. This is in accordance with the radiation measurement carried by the manufacturing company [22]. The third advantage is elimination of guide wire and its related complications during PPS insertion. It is well known; that it can be extremely dangerous if the guide wire penetrates the anterior cortex and enters the abdominal cavity [23].
Reported a rare complication wherein patient developed paraplegia due to subdural haematoma as a guide wire complication. With O-arm navigation; it is not possible to track real time location of guide wire [24]. Since the guide wire is not used in the technique described above; it eliminates the related complications altogether. There are few limitations. Like every new technique; it has a learning curve which is commensurate with the surgeon’s experience. There has been a controversy with regards to the amount of lumbar lordosis correction achieved in prone and lateral position. Yson suggested prone position is better however, did not find any significant difference [16,25]. Due to change in the navigational accuracy; we do not recommend this technique for more than three-disc levels. This report aims only for introduction of a novel technique. Additional multicentric studies with large sample size is necessary for validation of accuracy and efficacy of this technique.
Conclusion
OLIF cage and PPS insertion can be accomplished simultaneously in single lateral position without compromising its clinical and radiological benefits. This O-arm based navigationbased technique boasts the advantages of reducing operating time lost in repositioning of the patient and also decreasing the radiation exposure to the operating personnel.
References
- Oppenheimer JH, DeCastro I, McDonnell DE (2009) Minimally invasive spine technology and minimally invasive spine surgery. A Historical Review Neurosurgical Focus 27(3): E9.
- Mayer HM (1997) A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine 22(6): 691-699.
- Shen FH, Samartzis D, Khanna AJ, Anderson DG (2007) Minimally invasive techniques for lumbar interbody fusions. Orthop Clin North Am 38(3): 373-386.
- Kim TT, Drazin D, Shweikeh F, Pashman R, Johnson JP (2014) Clinical and radiographic outcomes of minimally invasive percutaneous pedicle screw placement with intraoperative CT (O-arm) image guidance navigation. Neurosurg Focus 36(3): E1-E7.
- Oertel MF, Hobart J, Stein M, Schreiber V, Scharbrodt W (2011) Clinical and methodological precision of spinal navigation assisted by 3D intraoperative O-arm radiographic imaging. Journal of Neurosurgery Spine 14(4): 532-536.
- Tanaka M, Blattert TR, Sugimoto Y, Takigawa T, Ozaki T (2018) C-Arm free oblique lumbar interbody fusion (OLIF) and lateral percutaneous pedicle screw fixation (lateral PPS): A technical note. Res Arthritis Bone Study 1(2): 1-9.
- Tanaka M, Sugimoto Y, Arataki S, Takigawa T, Ozaki T (2016) Computerassisted minimally invasive posterior lumbar interbody fusion without c-arm fluoroscopy. Acta Med Okayama 70(1): 51-55.
- Funao H, Ishii K, Momoshima S, Iwanami A, Hosogane N, et al. (2014) Surgeons’ exposure to radiation in single- and multi-level minimally invasive transforaminal lumbar interbody fusion; a prospective study. PLoS One 9(4): e95233.
- Ozgur BM, Agarwal V, Nail E (2010) Two-year clinical and radiographic success of minimally invasive lateral transpsoas approach for the treatment of degenerative lumbar conditions. SAS J 4(2): 41-46.
- Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme Lateral Interbody Fusion (XLIF): A novel surgical technique for anterior lumbar interbody fusion. Spine J 6(4): 435-443.
- Ahmadian A, Verma S, Mundis GM, Oskouian RJ, Smith DA, et al. (2013) Minimally invasive lateral retroperitoneal transpsoas interbody fusion for L4-5 spondylolisthesis: clinical outcomes. J Neuro Surg Spine 19(3): 314-320.
- Castro C, Oliveira L, Amaral R, Marchi L, Pimenta L (2014) Is the lateral transpsoas approach feasible for the treatment of adult degenerative scoliosis? Clin Orthop Relat Re 472(6): 1776-1783.
- Ahmadian A, Deukmedjian AR, Abel N, Dakwar E, Uribe JS (2013) Analysis of lumbar plexopathies and nerve injury after lateral retroperitonealtranspsoas approach: diagnostic standardization. J Neurosurg Spine 18(3): 289-297.
- Fujibayashi S, Kawakami N, Asazuma T, Ito M, Mizutani J, et al. (2017) complications associated with lateral interbody fusion: nationwide survey of 2998 cases during the first 2 years of its use in Japan. Spine 42(19): 1478-1484.
- Sellin JN, Mayer RR, Hoffman M, Ropper AE (2018) Simultaneous lateral interbody fusion and pedicle screws (SLIPS) with CT-guided navigation. Clin Neurol Neurosurg 175: 91-97.
- Drazin D, Kim TT, Johnson JP (2015) Simultaneous lateral interbody fusion and posterior percutaneous instrumentation: early experience and technical considerations. Biomed Res Int: 1-8.
- Blizzard DJ, Thomas JA (2018) MIS single-position lateral and oblique lateral lumbar interbody fusion and bilateral pedicle screw fixation: feasibility and perioperative results. Spine 43(6): 440- 446.
- Hilis A, Roldán L, Suarez D, Láez R, Agüeros JÁ, et al. (2017) One-shot CT image navigated circumferential fusion in a single lateral decubitus position: surgical technique. J Neurosurg Sci 61(4): 429-437.
- Wang HC, Yang YL, Lin WC (2008) Computer-assisted pedicle screw placement for thoracolumbar spine fracture with separate spinal reference clamp placement and registration. Surg Neurol 69(6): 597- 601.
- Lee K, Lee KM, Park MS, Lee B, Kwon DG, et al. (2012) Measurements of surgeons’ exposure to ionizing radiation dose during intraoperative use of C-arm fluoroscopy. Spine 37(14): 1240-1244.
- Jones DP, Robertson PA, Lunt B, Jackson SA (2000) Radiation exposure during fluoroscopically assisted pedicle screw insertion in the lumbar spine. Spine 25(12): 1538-1541.
- Silbermann J, Riese F, Allam Y, Reichert T, Koeppert H, et al. (2011) Computed tomography assessment of pedicle screw placement in lumbar and sacral spine: comparison between free-hand and O-arm based navigation techniques. Eur Spine J 20(6): 875-881.
- Chung T, Thien C, Wang YY (2014) A rare cause of postoperative paraplegia in minimally invasive spine surgery. Spine 39(3): E228-E230.
- Kakarla UK, Little AS, Chang SW, Sonntag VK, Theodore N (2010) Placement of percutaneous thoracic pedicle screws using neuronavigation. World Neurosurg 74(6): 606-610.
- Yson SC, Sembrano JN, Santos ER (2012) Does prone repositioning before posterior fixation produce greater lordosis in lateral lumbar interbody fusion (LLIF)? J Spinal Disord Tech 27(7): 364-369.
© 2019 Tanaka M. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






