- Submissions

Full Text
Researches in Arthritis & Bone Study
C-Arm Free Technique for Anterior Correction of Adolescent Idiopathic Scoliosis: A Technical Note
Tanaka M*, Mehta R, Fujiwara Y, Uotani K and Yamauchi T
Department of Orthopaedic Surgery, Okayama Rosai Hospital, Japan
*Corresponding author:Tanaka M, Department of Orthopaedic Surgery, Okayama Rosai Hospital, Japan
Submission: September 27, 2018;Published: October 24, 2018
Volume1 Issue3 October 2018
Abstract
Purpose: Computer-assisted spinal surgery is getting popular, however there is no technical report which describes the technique of anterior correction for adolescent idiopathic scoliosis without C-arm fluoroscopy in the lateral position.
Methods: The authors report the result of 1-year follow-up of a 14-year-old girl scoliosis patient with anterior correction. The patient has 40 degrees lumbar scoliosis and low back pain for more than 6 months. The authors performed C-arm free anterior correction with dual rod fixation in a lateral position.
Results: The patient was successfully treated with surgery and spinal alignment was preserved correctly. She had neither neurological deficits nor low back pain at 1 year of final follow-up.
Conclusion: The C-arm free anterior correction is useful technique, especially in that the surgeons and OR staff have no risk of adverse event of radiation.
Keywords:AIS; Navigation surgery; O-arm; C-arm free
Introduction
Adolescent idiopathic scoliosis (AIS) is the most common type of spinal deformity [1]. Scoliosis is defined as a lateral curvature of spinal column greater than 10 degrees and it associate with rotation [2]. Treatment of AIS is aimed at achieving a solid fusion and a balanced spine following correction of the deformity. Thoracolumbar curve or lumbar curves are among the most commonly observed AIS patients [3]. Anterior spinal instrumentation and fusion has been the treatment of choice for this curve. The anterior approach allows best control of the coronal and axial deformity with a smaller incision [4]. Many authors reported excellent results of anterior correction and fusion for AIS [5,6]. For this technique the C-arm is necessary to check the screw length and direction. This causes long OR time and radiation exposure to all operating room staff. However, there is no reports which indicated utility of navigation and O arm for anterior correction for AIS safely. So, the authors hereby report a technique of Navigation +O arm -assisted anterior correction for lumbar scoliosis thus avoiding C-arm fluoroscopy in a lateral decubitus position.
Operation procedure
Preoperative planning and radiograms: Preoperative planning and radiograms are important to evaluate scoliosis curve. Not only the standing posteroanterior and lateral views but also lateral bending and traction films are necessary to check the curve flexibility. MRI and CT with 3D reconstruction are must to rule out any cord anomaly or structural bony deformity.
Patient positioning: The patient is positioned in the right lateral decubitus position on a breaking Jackson frame to enable to get CT scan by O-arm. Axillary roll is placed to protect the neurovascular structure in the axilla. The patient position should be on the center in the true lateral position. The legs of the patient should be slightly flexed to relax the psoas and the lumbar nerve plexus. The patient is secured to the Jackson table with tape. Somatosensory evoked potentials (SEP) and motor evoked potentials (MEP) are used for deformity correction.
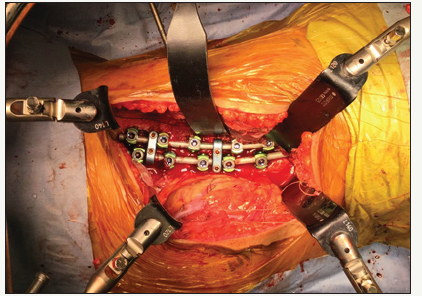
Thoracotomy: The approximate 20cm left oblique skin incision is made along the left 11th rib for this approach. The subcutaneous fat layers are dissected until the abdominal musculature is reached. The external, internal and transverse abdominal muscles are splitted along the direction of their fibers. To avoid iliohypogastric and ilioinguinal nerve injury a Bipolar cautery should be used carefully. The 11 rib is exposed and resected with a rib cutter. Bone wax is applied at the cut ends to control bleeding. Once inside the chest cavity, the diaphragm is cut in a circumferential way as in a traditional anterior approach. The self-retaining retractor blades are then applied resting on the anterior border of psoas muscle. Use of a hand-held retractor placed between peritoneal contents and the probe will minimize risk of injury to ureters and vascular structures anteriorly. The reference frame is attach to L1 spinous process, which is the center from T11-L3 and take a CAT scan (Figure 1).
Figure 1:The reference frame attached to the L1 spinous process and the self-retaining retractors in place.
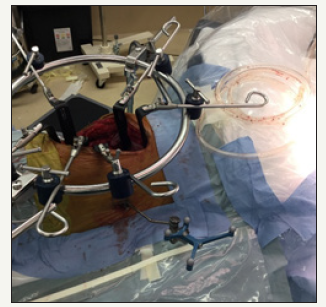
Figure 2A:The navigated pedicle probe is used (a) for penetrating the opposite side of the cortex.
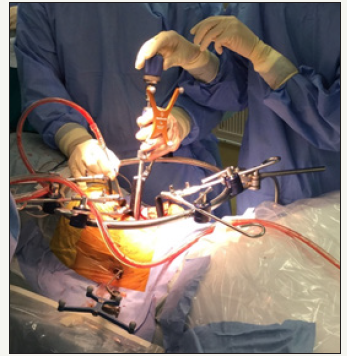
Figure 2B:Measuring the length of the screw.
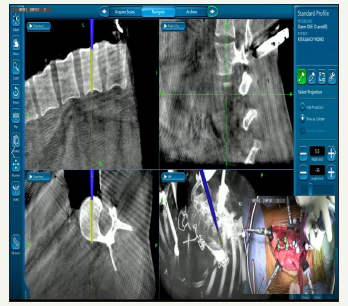
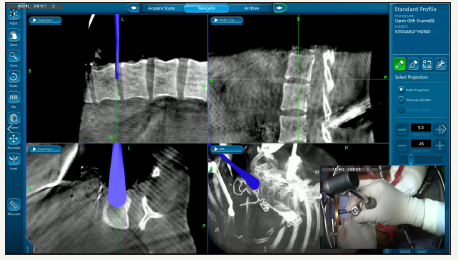
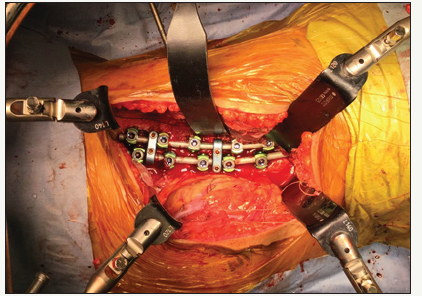
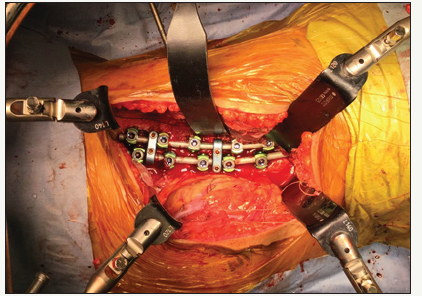
Screw insertion: Once the self-retractor blades are attached to the ring, O-arm scan is performed to use a navigation. A dual staple is placed on the lateral vertebral body for screw placement. After making the screw hole with the navigated high speed bar, the navigated pedicle probe is used for penetrating the opposite side of the cortex and measuring the length of the screw (Figure 2a & 2b). The posterior screw is inserted first and then anterior screw using navigation (Figure 3). Screw placement should usually proceed sequentially more anterior as the upper and lower instrumented vertebrae are approached (Figure 4).
Figure 3:Screw insertion under navigation.
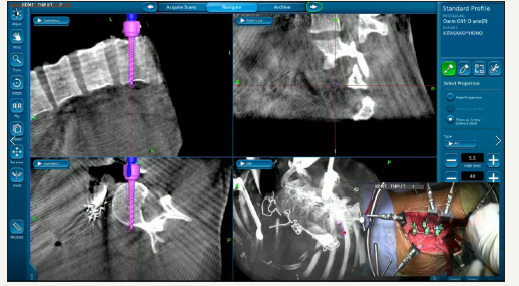
Figure 4:Sequentially placed screws.

Figure 5:Disc space preparation with navigated shaver.
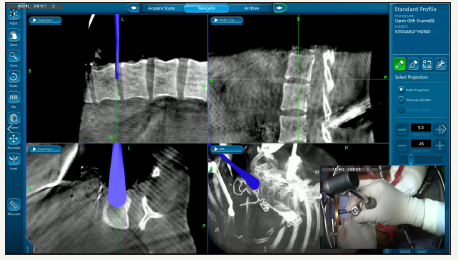
Disc space preparation: The annulus is incised using a knife and an annulotomy is performed. A thorough discectomy is performed using Kerrison roungers, navigated ring curettes, navigated shaver (Figure 5), and pituitaries. The navigated Cobbs is passed along both end plates to contralateral annulus with a mallet (Figure 6).
Figure 6:The navigated Cobbs is passed along both end plates to contralateral annulus.
Rod insertion and derotation: Rods are cut to the measured length and are bended to adjust the scoliosis curve (Figure 7). Then the anterior rod is inserted first (Figure 8a) and is rotated 90 degrees to make lordosis (Figure 8b). Most of the correction is to be achieved during this step. After putting the posterior rod, the only way of achieving correction is the in-situ rod bending. The resected rib is used as auto graft into the intervertebral disc space and the crosslink is inserted between two rods (Figure 9).
Figure 7:Rod contouring according to the degree of scoliosis
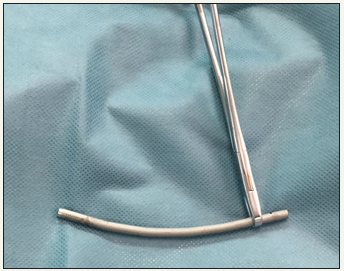
Figure 8A:The anterior rod is inserted first
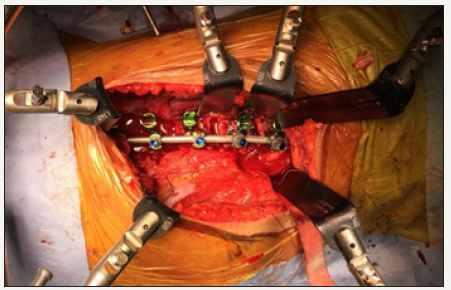
Figure 8B:Is rotated 90 degrees to make lordosis.

Figure 9:Cross link inserted between two rods.
Case Presentation
Patient history
A 14-year-old female presented with gradually progressing deformity over 3 years in spite of bracing. scoliosis. She started with minimal low back pain since 6 months. She had no neurological deficit.
Physical examination
On examination, her head was central, shoulders were balanced. There was left sided lumbar convexity with lumbar hump, asymmetry of the waist line, right side flank crease. There was no leg length discrepancy. There were no signs of upper motor neuron lesion. The range of her spine motion was limited.
Preoperative imaging
Figure 10A:Pre-operative radiographs.
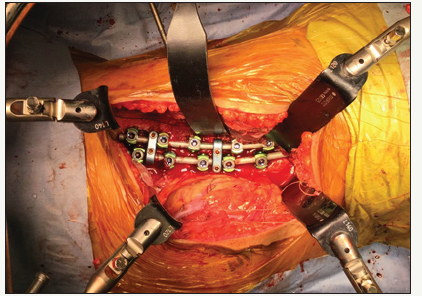
Figure 10B:CT with 3d reconstruction.
The Cobb angle on erect films measured as follows: left Thoraco/Lumbar 40 correcting to 25 degree on bending film, right main thoracic curve 20 degree correcting to measurement of her thoracic region is 20 degrees correcting to 7 degree on bending film. (Figure 10a). CT and MRI showed no abnormality (Figure 10b).
Surgery
Operative time was 3 hours 35 minutes and intra operative blood loss was 350 ml. There was no perioperative adverse event.
Follow-up
We followed up the patient at 1, 6 and 12 months. By one month, she was back to nearly full activity. The immediate postoperative and follow up radiograms and CT demonstrated good correction of curve and maintain an appropriate sagittal alignment (Figure 11). At one year follow up there was 3-degree loss of correction (Figure 12).
Figure 11:Accurately placed screw with bicortical purchase.
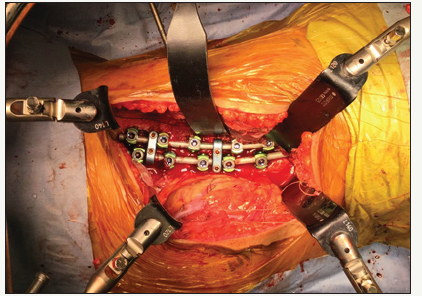
Figure 12:Erect radiographs at final follow up.
Discussion
The goal of spinal correction for AIS is maximize the degree of curve correction and preserve as many motion segments as possible [7]. Historically, the anterior approach was considered the preferred approach because of its good coronal and rotatory correction [8]. Recently several authors reported the long-term good outcomes of anterior instrumented fusion for thoracolumbar AIS [5,6]. The surgeons using a posterior approach include more levels in the instrumentation for comparable curves [8]. Also, anterior correction avoids the crankshaft phenomenon in skeletally immature patients and hence allows saving distal fusion levels [9]. However, for the anterior approach, there are some disadvantages are reported, including trunk scarring, pseudoarthrosis [10] and pulmonary impairment [11]. Advantages and disadvantages of anterior procedure are summarized in table1. Computer-assisted spinal surgery is the trend for putting pedicle screws, nowadays three-dimensional (3D) image guidance technology is available for posterior scoliosis surgery [12]. Among them, the O-arm and Stealth system (Medtronic Inc, Minneapolis, MN) is one of the most beneficial systems because of its excellent accuracy and automated registration [13]. Many reports [13,14] provide the facts that the O-arm based navigation technique showed a higher accuracy rate compared to the preoperative CT-based navigation or fluoroscopic techniques [15]. As we can see the axial and 3D image intraoperatively, there is almost no risk of screw misplacement. Another advantage is its potential to reduce radiation exposure for the surgeon and the operating room staff at centers performing large numbers of spine procedures. Currently the radiation problem is the main concern for scoliosis surgeons because for screw insertion technique it requires a greater intraoperative radiation exposure. There are reports documenting the harmful effects of radiation exposure to the surgeons and the operative team [16]. There are attempts of not using C-arm for posterior lumbar interbody fusion (PLIF) [17] and oblique lumbar interbody fusion (OLIF) in literature [18].
Table 1:

Also, in our experience, with this technique there has been no case of surgical site infection (SSI) which indicates that probably the repeated use of c arm in the conventional anterior technique is a contributing factor for SSI. Thus, this novel technique of C-arm free anterior correction may offer several important advantages over conventional anterior technique. This report is only for the introduction of a novel anterior method. Further studies are required to collect more data regarding the utility, advantages and drawbacks of this technique before its utility spreads.
Conclusion
C-arm free anterior correction for lumbar scoliosis with O-arm and navigation is a safe and effective technique. This technique avoids any radiation exposure for the surgeon and staff compared with conventional fluoroscopic techniques.
References
- Lonstein JE (1995) Idiopathic scoliosis. In: Lonstein JE, Bradford DS, Winter RB, Ogilvie J (Eds.), Moe’s textbook of scoliosis and other spinal deformities. (3rd edn), WB Saunders, Philadelphia, USA, pp. 219-256.
- Brian V, Slasky JB (2001) Adolescent idiopathic scoliosis: Review and current concepts. Am Fam Physician 64(1): 111-116.
- Lenke LG, Betz RR, Clements D, Merola A, Haher T, et al. (2002) Curve prevalence of a new classification of operative adolescent idiopathic scoliosis: does classification correlate with treatment? Spine (Phila Pa 1976) 27(6): 604-611.
- Kelly DM, McCarthy RE, McCullough FL, Kelly HR (2010) Longterm outcomes of anterior spinal fusion with instrumentation for thoracolumbar and lumbar curves in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 35(2): 194-198.
- Delfino R, Pizones J, Ruiz Juretschke C, Sánchez MF, Zúñiga L (2017) Selective anterior thoracolumbar fusion in adolescent idiopathic scoliosis: long-term results after 17-year follow-up. Spine (Phila Pa 1976) 42(13): E788-E794.
- Sudo H, Kaneda K, Shono Y, Iwasaki N (2016) Short fusion strategy for thoracolumbar and lumbar adolescent idiopathic scoliosis using anterior dual-rod instrumentation. Bone Joint J 98-B(3): 402-409.
- Wang T, Zeng B, Xu J, Chen H, Zhang T, et al. (2008) Radiographic evaluation of selective anterior thoracolumbar or lumbar fusion for adolescent idiopathic scoliosis. Eur Spine J 17(8): 1012-1018.
- Abel MF, Singla A, Feger MA, Sauer LD, Novicoff W (2016) Surgical treatment of Lenke 5 adolescent idiopathic scoliosis: Comparison of anterior vs posterior approach. World J Orthop 7(9): 553-560.
- Shufflebarger HL, Clark CE (1991) Prevention of the crankshaft phenomenon. Spine (Phila Pa 1976) 16(8 Suppl): S409-S411.
- Gitelman Y, Lenke LG, Bridwell KH, Auerbach JD, Sides BA (2011) Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure: a 10-year follow-up analysis. Spine (Phila Pa 1976) 36(20): 1665-1672.
- Kim YJ, Lenke LG, Bridwell KH, Cheh G, Sides B, et al. (2008) Prospective pulmonary function comparison of anterior spinal fusion in adolescent idiopathic scoliosis: thoracotomy versus thoracoabdominal approach. Spine (Phila Pa 1976) 33(10): 1055-1060.
- Zhang W, Takigawa T, Wu Y, Sugimoto Y, Tanaka M, et al. (2017) Accuracy of pedicle screw insertion in posterior scoliosis surgery: a comparison between intraoperative navigation and preoperative navigation techniques. Eur Spine J 26(6): 1756-1764.
- Houten JK, Nasser R, Baxi N (2012) Clinical assessment of percutaneous lumbar pedicle screw placement using the O-arm multidimensional surgical imaging system. Neurosurgery 70(4): 990-995.
- Kim TT, Drazin D, Shweikeh F, Pashman R, Johnson JP (2014) Clinical and radiographic outcomes of minimally invasive percutaneous pedicle screw placement with intraoperative CT (O-arm) image guidance navigation. Neurosurg Focus 36(3): E1.
- Oertel MF, Hobart J, Stein M, Schreiber V, Scharbrodt W (2011) Clinical and methodological precision of spinal navigation assisted by 3D intraoperative O-arm radiographic imaging. J Neurosurg Spine (Phila Pa 1976) 14(4): 532-536.
- Baaj AA, Beckman J, Smith DA (2013) O-Arm-based image guidance in minimally invasive spine surgery: Technical note. Clin Neurol Neurosurg 115(3): 342- 345.
- Tanaka M, Sugimoto Y, Arataki S, Takigawa T, Ozaki T (2016) Computerassisted minimally invasive posterior lumbar interbody fusion without c-arm fluoroscopy. Acta Med Okayama 70(1): 51-55.
- Tanaka M, Blattert TR, Sugimoto Y, Takigawa T, Ozaki T (2018) C-Arm Free oblique lumbar interbody fusion (olif) and lateral percutaneous pedicle screw fixation (lateral pps): Technical note. Researches in Arthritis & Bone Study 1(2): 2018.
© 2018 Tanaka M. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






