- Submissions
Full Text
Researches in Arthritis & Bone Study
C-Arm Free Oblique Lumbar Interbody Fusion (OLIF) and Lateral Percutaneous Pedicle Screw Fixation (Lateral PPS): Technical Note
Tanaka M1, Blattert TR2, Sugimoto Y1, Takigawa T1 and Ozaki T1
1Department of Orthopaedic Surgery, Okayama University Hospital, Japan
2Department for Spine Surgery and Traumatology, Schwarzach Orthopaedic Clinic, Germany
*Corresponding author: Tanaka M, Department of Orthopaedic Surgery, Okayama University Hospital, Japan
Submission: May 23, 2018; Published: August 03, 2018
Volume 1 Issue 2 August 2018
Abstract:
Purpose: Computer-assisted spinal surgery is getting popular, however there is no technical report which describes the technique of oblique lumbar interbody fusion (OLIF) and percutaneous pedicle screw fixation (PPS) without C-arm fluoroscopy in the lateral position.
Methods:The authors report the result of 2-year follow-up of a 69-year-old female patient with L4 degenerative spondylolisthesis. The patient has suffered low back pain and intermittent claudication for more than 4 years. The authors performed C-arm free OLIF and PPS in a single lateral position.
Results:The patient was successfully treated with surgery and lumbar alignment was preserved correctly. She had neither neurological deficits nor low back pain at 2 year of final follow-up.
Conclusion:The C-arm free OLIF and lateral PPS is useful technique, especially in that the surgeons and OR staff have no risk of adverse event of radiation.
Keywords:Lumbar spine; Navigation surgery; Lateral lumbar interbody fusion; O-arm; Percutaneous pedicle screw; C-Arm Free
Introduction
Minimally invasive spine surgery (MISS) has been popular in spinal fusion compared with conventional open technique because MISS ensures better results for postoperative pain and wound cosmetics [1,2]. Lateral lumbar interbody fusion is also getting popular for various spinal disease including spinal deformity, trauma, infection and degenerative disease [3,4]. For this procedure, the patient position should be changed from lateral position to prone position. This causes long OR time and another dressing for the patient. Computer-assisted spinal surgery is also the trend for putting pedicle screws, nowadays three-dimensional (3D) image guidance technology is available for MISS [5-9]. Among them, the O-arm and Stealth system (Medtronic Inc, Minneapolis, MN) is one of the most beneficial systems because of its excellent accuracy and automated registration [10]. However, there are few reports which indicated its utility for spinal instrumentation safely [5-9]. Currently the radiation problem is the main concern for MISS surgeons because for MISS technique it requires a long-time intraoperative radiation exposure [11]. To solve this problem, the authors hereby report a new technique of computer-assisted OLIF without C-arm fluoroscopy (C-arm free OLIF) and lateral PPS in a single lateral decubitus position.
Operation Procedure
Preoperative planning
Preoperative planning is important to check the location of the iliac crest and lower rib, position of the psoas, anterior vasculature, posterior lumbar nerve plexus and the kidney via axial MRI. Severe adhesion due to previous abdominal surgery is contraindication for OLIF [12].
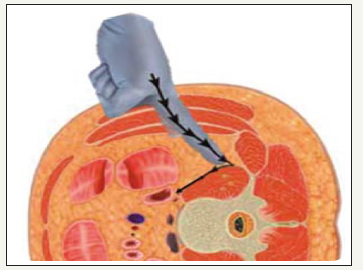
Patient positioning for C-arm free PPS
The patient is positioned in the right lateral decubitus position on a Jackson frame to enable to get CT scan by O-arm (Figure 1). Axillary roll is placed to protect the neurovascular structure in the axilla. The patient position should be on the center but on one third to the back end of the table and 20 degrees tilted toward the face from the true lateral position (Figure 2), which enable to perform lateral PPS easily. The clearance of pedicle screw insertion (red arrow) should be confirmed before surgery. The legs of the patient should be slightly flexed to loosen the psoas and the lumbar nerve plexus. The patient is secured to the Jackson table with tape (Figure 3).
figure 1: Patient positioning: The patient is positioned in the right lateral decubitus position on a Jackson frame.

figure 2:Semi-decubitus lateral position the true lateral decubitus position. In this position,
a. PPS is difficult to insert due to the table. Red arrow shows PPS direction.
b. Home position the patient position should be on the center but on one third to the back end of the table and 20 degrees tilted toward the face from the true lateral position. There is clearance of PPS direction.
c. OLIF position the table is 20 degrees tilted toward back, however the patient is the true lateral position.
d. PPS position the table is 20 degrees tilted toward face.
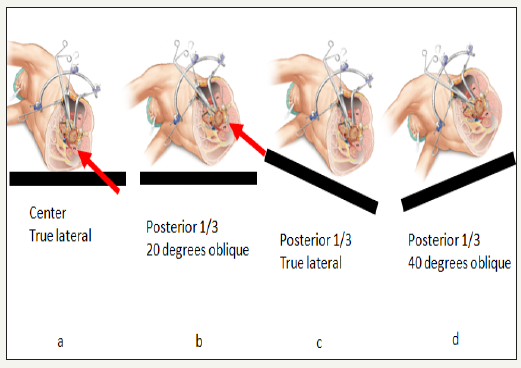
figure 3: Skin taping: The patient is secured to the Jackson table with tape.

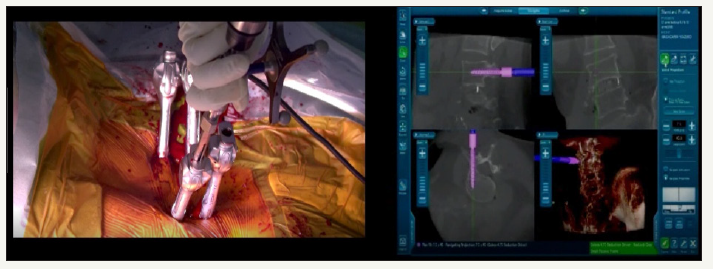
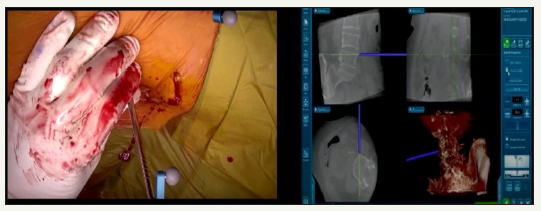
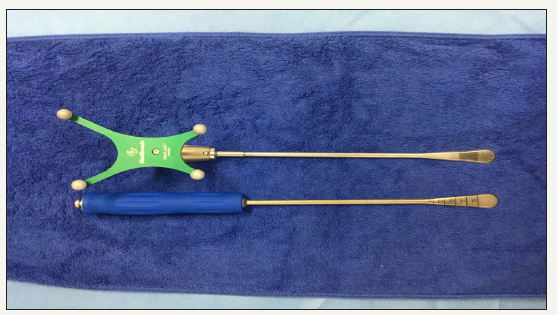
Lateral PPS
The percutaneous reference frame pin is anchored into the posterior superior iliac spine. The O-Arm is then positioned and the 3D reconstructed images are obtained and transmitted to the Stealth station navigation system Spine 7R (Medtronic, Memphis, USA). For OLIF, the nueromonitouring is not necessary, however we routinely use neuromonitouring to prevent neurological complication during lateral PPS and OLIF. The Jackson table should be rotated 20 degrees ventral side (Figure 4). After verifying every navigated instrument, PPSs are inserted in the lateral position (Figure 5). With the Solera Sextant percutaneous pedicle system, it is easy and accurate to measure the rod length and also the C-arm is not necessary to insert the rod correctly (Figure 6).
figure 4: PPS position: There is a space for right side PPS.
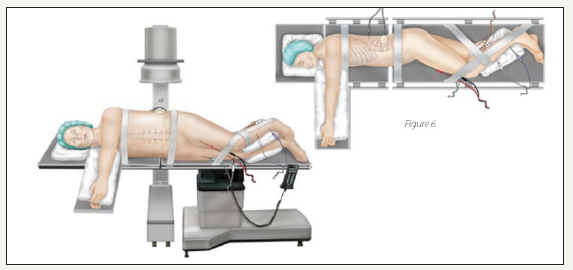
figure 5: PPS insertion: Under a navigation guidance, four PPSs were inserted without C-arm.

figure 6: Rod insertion: With the Solera percutaneous pedicle system it is easy and accurate to measure the rod length and also the C-arm is not necessary to insert the rod correctly.
Patient repositioning for C-arm free OLIF
For OLIF, the table should be rotated 20 degrees to the back and get the true lateral position, which enable to perform OLIF easily.
Dissection
The 4 cm left oblique skin incision is made for OLIF using the navigated pin point probe. This skin incision usually locates two finger breadth laterals from the anterior disc margin. The subcutaneous fat layers are dissected until the abdominal musculature is reached. The external, internal and transverse abdominal muscles are divided along muscle fibers, not to cut the muscle fibers. To avoid iliohypogastric and ilioinguinal nerve injury, the monopolar should not be used. Once inside the retroperitoneal space, the both index fingers are used to follow the internal abdominal wall posteriorly down to the psoas muscle, which can be visualized (Figure 7).
figure 7: Anterior psoas approach: The external, internal and transverse abdominal muscles are divided along muscle fibers. Once inside the retroperitoneal space, the both index fingers are used to follow the internal abdominal wall posteriorly down to the psoas muscle.
Anterior psoas approach
The navigated first Direct Lateral Dilator is resting on the anterior border of psoas muscle at the disc level (Figure 7). Use of a hand-held retractor placed between peritoneal contents and the probe will minimize risk of injury to ureters and vascular structures anteriorly. The use of neuromonitouring is recommended not to injure the nerve. After the first probe has safely passed in front of the anterior portion of the psoas, the dilator is impacted into the annulus for firm fixation, sequential dilation is used to a diameter of 22mm. Measure the depth from the skin to the disc space and the retractor is placed in the correct position. The retractor assembly is attached to the flexible arm and then stability pins are inserted to fix the retractor.
Disc preparation
The MAST Quadrant illumination system is attached to the retractor blades. The annulus is then incised and an Annulotomy is created using the bayoneted knife under microscopy. A though discectomy is performed using Kerrison rongeurs, ring curettes, and pituitaries. Our original navigated Cobbs is passed along both end plates to contralateral annulus with a mallet (Figure 8).
figure 8: The navigated first direct lateral dilator: The navigated first direct lateral dilator is resting on the anterior border of psoas muscle at the disc level.
Trialing
The disc space is distracted with navigated trials until adequate disc space height is obtained. The important point is that the disc space in the navigation image doesn’t open even though the proper height of the trial. The tightness during the impaction of the trail and preoperative measuring of the disc height are the key to choose the correct cage height (Figure 9).
figure 9: Disc preparation (original navigated Cobb): Our original navigated Cobbs is passed along both end plates to contralateral annulus with a mallet.
Cage placement
figure 10: Trialing: The tightness during the impaction of the trail and preoperative measuring of the disc height are the key to choose the correct cage height.

Once trialing is complete, a mallet is then used to gently insert the OLIF cage while monitoring placement under navigation guidance (Figure 10). Iliac bone is inserted into cage hole, hydroxyapatite is also a good option for bone graft. After the implant is positioned in the center of the disc space, the inserter is unthreaded from the implant and removed.
Case Presentation
Patient history
A 69-year-old woman was referred to our orthopedic department on December of 2014 for low back pain and intermittent claudication. She had described low back pain and intermittent claudication for more than 2 years. She also had numbness and muscle weakness of her left leg.
Physical examination
On examination, she could walk only 200 meters duo to left leg pain. There was no hyperreflexia of her legs, no abnormal abdominal reflex, but there was a severe pain in her left leg and the range of her spine motion was limited.
Preoperative imaging
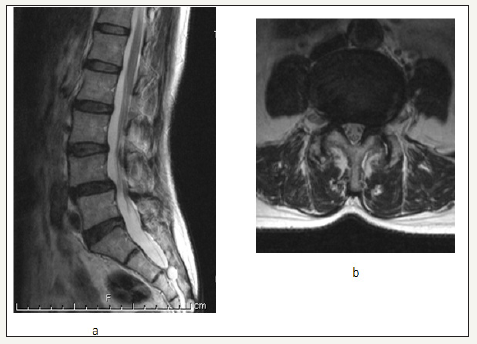
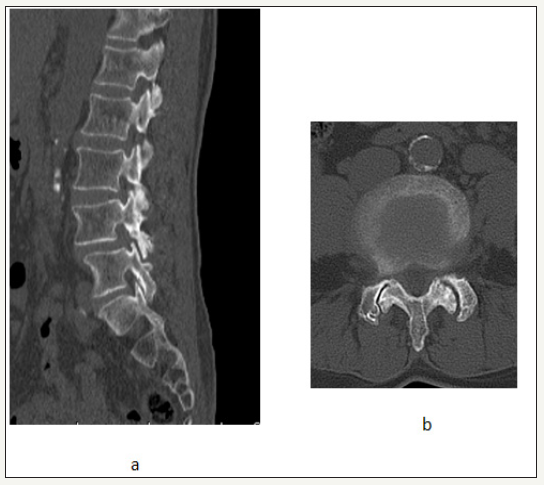
Radiograms at initial visit demonstrated grade 1 degenerative spondylolisthesis and moderate instability at L4/5 level (Figure 11). Preoperative MRI revealed mild L4/5-disc degeneration and L4 slip. The dural sac stenosis was also observed at that level (Figure 12). CT also shows L4 anterior slip and L4/5 facet osteoarthritis and opening (Figure 13).
figure 11: Cage placement: Once trialing is complete, a mallet is then used to gently insert the OLIF cage while monitoring placement under navigation guidance.
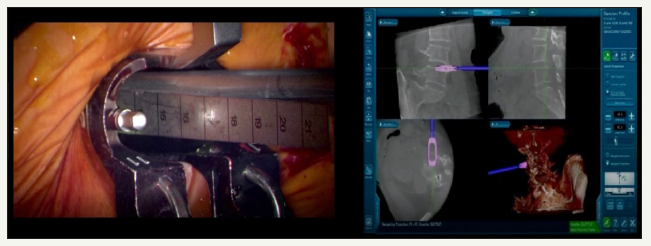
figure 12: Preoperative lumbar radiograms
a: anteroposterior view
b: lateral neutral position: There was grade I spondylolisthesis at L4 level.
c: lateral flexion view: There was an intermediate instability at L4/5 revel.
d: lateral extension view
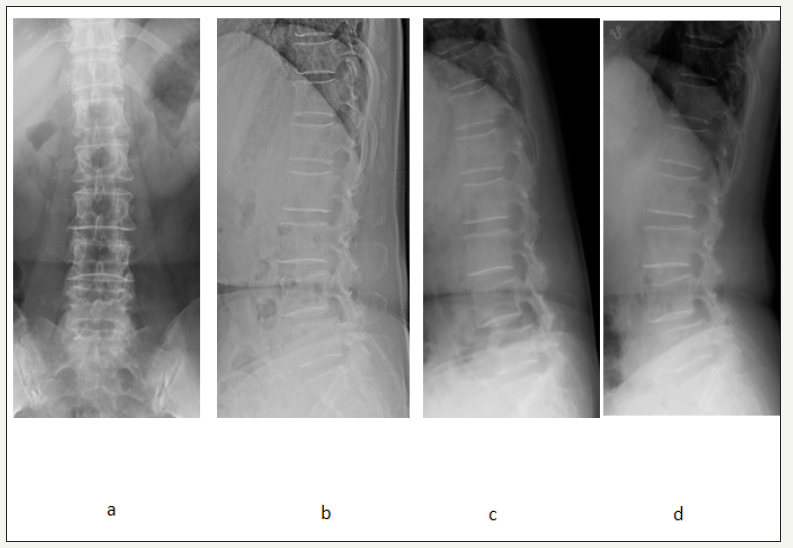
figure 13: Preoperative MRI.
a: T2 weighted midsagittal image: L4/5 stenosis was observed.
b: T2 weighted axial image: there was an intermediate dural stenosis at L4/5 level.
Surgery
Operative time was 2 hours 35 minutes and estimated blood loss was 10ml. There have been no postoperative complications, and no neurological compromise.
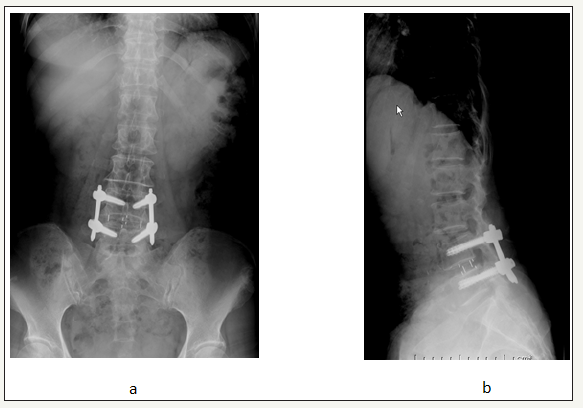
Follow-up imaging
figure 14: Preoperative CT
a: Sagittal image: There was disc narrowing at L4/5 level.
b: axial image: The facet osteoarthritis and opening was observed at L4/5 level.
By 2 months, she was back to nearly full activity. The post operative CTs demonstrated good correction of curve and maintain an appropriate sagittal alignment (Figure 14). She has been good spinal balance and no neurological deficit for more than one year (Figure 15,16).
figure 15: Post operative CT
a: sagittal reconstruction image: A solid bony fusion is obtained.
b: axial image et L4: L4 PPSs were inserted correctly.
c: axial image at L4/5: OLIF cage was located in the center of the disc space.
d: axial image at L5: L5 PPSs were also inserted correctly.
e: 3-D anteroposterior image: The rod length and position were correct.
f: 3-D lateral image: The spondylolisthesis was reduced.
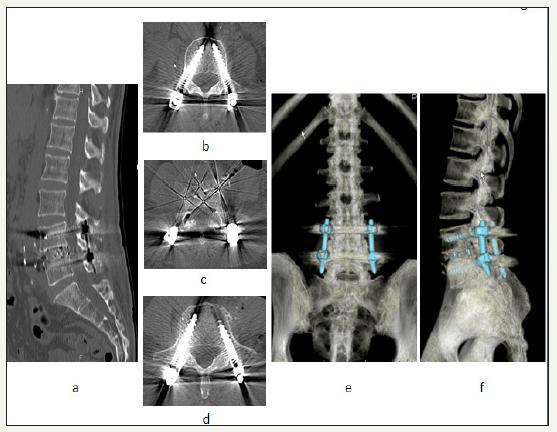
figure 16: Final follow up lumbar radiograms
a: anteroposterior view:
b: lateral neutral position: there is mild spondylolisthesis at L4 level.
Discussion
Table 1:
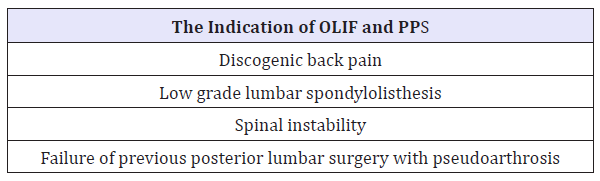
Table 2:
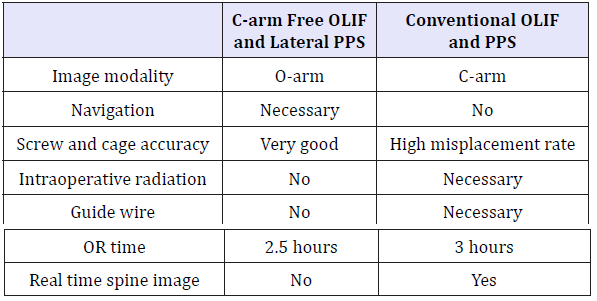
Since Pimenta first performed retroperitoneal transpsoas minimally invasive LLIF (XLIFR) [13], many reports have been described [14,15]. Table 1 shows the indication of LLIF and PPS. LLIF has a lot of advantages over TLIF/PLIF, including large cage, preservation of posterior muscle, minimal blood loss [16]. However, LLIF has some disadvantages, which are psoas muscle weakness and lumbar nerve plexus paralysis [17]. Thus, to reduce such complications, OLIF has been getting popular. For OLIF procedure, approach site to the disc is not the middle of the psoas but the anterior aspect of the psoas. That is the reason that this procedure can reduce the lumbar nerve plexus paralysis. To perform LLIF and PPS, we need a lot of radiation exposure [11]. So there is some attempt not to use any C-arm during lumbar interbody fusion surgery [10]. For conventional PPS, the patient position should be prone position. However, recently Hill is reported a combined approach for LLIF and PPS in the same lateral decubitus position [18]. This procedure reduces OR time and medical cost. In our data, the OR time of this technique reduced approximately 30 minutes than that of two stage conventional OLIF and PPS. The C-arm free OLIF and Lateral PPS may offer several important advantages over conventional OLIF and PPS [5,6] (Table 2). The first advantage is the accuracy rate for percutaneous pedicle screw insertion. Many reports [5-9] provide the facts that the O-arm based navigation technique showed a higher accuracy rate compared to the preoperative CT-based navigation or fluoroscopic techniques [6,8,19]. The pedicle screw perforation rate of O-arm was from 1% to 4% [5-7,19]. On the other hand, those of preoperative CT-based navigation and fluoroscopy techniques were 3% to 10% [20-22] and 13% to 30% [9,23,24], respectively. With PPS method, this accuracy rate is more important because the sounding technique to check the perforation is not available for this technique. The second advantage is its potential to reduce radiation exposure for the surgeon and the operating room stuffs at centers performing large numbers of MIS procedures. A lot of reports have documented the harmful effects of radiation exposure to the surgeons and the operative team [25-27]. Advanced imaging, O-arm navigation, may be most valuable in reducing radiation time for pedicle screw insertion [5,10]. Regretfully, most O-arm reports recommended to use additional C-arm fluoroscopy for cages or rod insertion or didn’t mention about it [5-9]. Our new technique doesn’t require any C-arm fluoroscopy for cage, or screw insertion. And also Solera Sextant system isn’t not necessary for image guidance during rod insertion. Most importantly, radiation exposure to the patient also needs to be considered. Each O-arm 3D scan is equal to 60% of an ordinary CT scan according to the radiation measurement carried by the manufactured company (Medtronic, USA) [7].
The third advantage is that there is no risk of guide wire problem [28,29]. If the anterior cortex is perforated by guide wire, conventional percutaneous method became very dangerous to perpetrate advanced into the abdominal cavity. Chung et al. [30] reported the case with MIS-TLIF who postoperatively developed paraplegia due to subdural hematoma as a rare complication of a guide wire. If the guide wire is used for O-arm technique, one of the risks is the inability to track the real time location of the guide wire [5]. However, our technique doesn’t require the guide wire, so there is no risk for guide wire related problem. The pedicle shadows of overweighed or osteoporotic patient are sometime difficult to figure out in C-arm fluoroscopy [31]. This report is only for the introduction of the novel method. In addition to clinical accumulation of experience and accuracy examination should be performed until the use of this technique spreads.
Conclusion
C-arm free OLIF and lateral PPS with O-arm and navigation is a safe and effective technique. This technique provides no radiation exposure for the surgeon and may reduce its exposure compared with conventional fluoroscopic techniques.
References
- Dasenbrock HH, Juraschek SP, Schultz LR, Witham TF, Sciubba DM, et al. (2012) The efficacy of minimally invasive discectomy compared with open discectomy: a meta analysis of prospective randomized controlled trials. J Neurosurg Spine 16(5): 452-462.
- Wu RH, Fraser JF, Hartl R (2010) Minimal access versus open transforaminal lumbar interbody fusion: meta-analysis of fusion rates. Spine (Phila Pa 1976) 35(26): 2273-2281.
- Kaiser MG, Eck JC, Groff MW, Watters WC, Dailey AT, et al. (2014) Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 1: introduction and methodology. J Neurosurg Spine 21(1): 2-6.
- Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1(1): 2-18.
- Kim TT, Drazin D, Shweikeh F, Pashman R, Johnson JP (2014) Clinical and radiographic outcomes of minimally invasive percutaneous pedicle screw placement with intraoperative CT (O-arm) image guidance navigation. Neurosurg Focus 36(3): E1.
- Oertel MF, Hobart J, Stein M, Schreiber V, Scharbrodt W (2011) Clinical and methodological precision of spinal navigation assisted by 3D intraoperative O-arm radiographic imaging. J Neurosurg Spine 14(4): 532-536.
- Silbermann J, Riese F, Allam Y, Reichert T, Koeppert H, et al. (2011) Computer tomography assessment of pedicle screw placement in lumbar and sacral spine: comparison between free-hand and O-arm based navigation techniques. Eur Spine J 20(6): 875-881.
- Baaj AA, Beckman J, Smith DA (2013) O-Arm-based image guidance in minimally invasive spine surgery: Technical note. Clin Neurol Neurosurg 115(3): 342- 345.
- Houten JK, Nasser R, Baxi N (2012) Clinical assessment of percutaneous lumbar pedicle screw placement using the O-arm multidimensional surgical imaging system. Neurosurgery 70(4): 990-995.
- Tanaka M, Sugimoto Y, Arataki S, Takigawa T, Ozaki T (2016) Computerassisted minimally invasive posterior lumbar interbody fusion without c-arm fluoroscopy. Acta Med Okayama 70(1): 51-55.
- Funao H, Ishiin K, Momoshima S, Iwanami A, Hosogane N, et al. (2014) Surgeons’ exposure to radiation in single- and multi-level minimally invasive transforaminal lumbar interbody fusion; a prospective study. PLoS One 9(4): e95233.
- Ozgur BM, Agarwal V, Nail E, Pimenta L (2010) Two-year clinical and radiographic success of minimally invasive lateral transpsoas approach for the treatment of degenerative lumbar conditions. SAS J 4(2): 41-46.
- Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6(4): 435-443.
- Ahmadian A, Verma S, Mundis GM, Oskouian RJ, Smith DA, et al. (2013) Minimally invasive lateral retroperitoneal transpsoas interbody fusion for L4-5 spondylolisthesis: clinical outcomes. J Neurosurg Spine 19(3): 314-320.
- Castro C, Oliveira L, Amaral R, Marchi L, Pimenta L (2014) Is the lateral transpsoas approach feasible for the treatment of adult degenerative scoliosis? Clin Orthop Relat Res 472(6): 1776-1783.
- Ha KY, Kim YH, Seo JY, Bae SH (2013) Percutaneous posterior instrumentation followed by direct lateral interbody fusion for lumbar infectious spondylitis. J Spinal Disord Tech 26(3): E95-E100.
- Ahmadian A, Deukmedjian AR, Abel N, Dakwar E, Uribe JS (2013) Analysis of lumbar plexopathies and nerve injury after lateral retroperitonealtranspsoas approach: diagnostic standardization. J Neurosurg Spine 18(3): 289-297.
- Hilis A, Roldan L, Fernandez D, Laez R, Agueros JA, et al. (2016) “One- Shot” CT image navigated circumferential fusion in a single lateral decubitus position: surgical technique. J Neurosurg Sci 61(4): 429-437
- Zhang W, Takigawa T, Wu Y, Sugimoto Y, Tanaka M, et al. (2016) Accuracy of pedicle screw insertion in posterior scoliosis surgery: a comparison between intraoperative navigation and preoperative navigation techniques. Eur Spine J 26(6): 1756-1764.
- Francesco C, Andrea C, Ortolina A, Fabio G, Alberto Z, et al. (2011) Spinal Navigation: standard pre-operative versus intra-operative computed tomography data set acquisition for computer-guidance system: Radiological and clinical study in 100 consecutive patients. Spine 36(24): 2094-2098.
- Kosmopoulos V, Schizas C (2007) Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 32(3): E111-E120.
- Wang HC, Yang YL, Lin WC, Chen WF, Yang TM, et al. (2008) Computerassisted pedicle screw placement for thoracolumbar spine fracture with separate spinal reference clamp placement and registration. Surg Neurol 69(6): 597-601.
- Fraser J, Gebhard H, Irie D, Parikh K, Hartl R (2010) Iso-C/3-dimensional neuro navigation versus conventional fluoroscopy for minimally invasive pedicle screw placement in lumbar fusion. Minim Invasive Neurosurg 53(4): 184-190.
- Ringel F, Stoffel M, Stuer C, Meyer B (2006) Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery 59(4 Suppl 2): ONS361-ONS366.
- Lee K, Lee KM, Park MS, Lee B, Kwon DG, et al. (2012) Measurements of surgeons’ exposure to ionizing radiation dose during intraoperative use of C-arm fluoroscopy. Spine (Phila Pa 1976) 37(14): 1240-1244.
- Jones DP, Robertson PA, Lunt B, Jackson SA (2000) Radiation exposure during fluoroscopically assisted pedicle screw insertion in the lumbar spine. Spine (Phila Pa 1976) 25(12): 1538-1541.
- Theocharopoulos N, Perisinakis K, Damilakis J, Papadokostakis G, Hadjipavlou A, et al. (2003) Occupational exposure from common fuluoroscopic projection used in orthopaedic surgery. J Bone Joint Surg Am 85-A(9): 1698-1703.
- (2009) Medtronic navigation: O-Arm imaging system version 3.1 dosimetry report. MA: Medtronic, Colorado, USA.
- Ul Haque M, Shufflebarger HL, O Brien M, Macagno A (2006) Radiation exposure during pedicle screw placement in adolescent idiopathic scoliosis: is fluoroscopy safe? Spine (Phila Pa 1976) 31(21): 2516-2520.
- Chung T, Thien C, Wang YY (2014) A rare cause of postoperative paraplegia in minimally invasive spine surgery. Spine (Phila Pa 1976) 39(3): E228-E230.
- Kakarla UK, Little AS, Chang SW, Sonntag VK, Theodore N (2010) Placement of percutaneous thoracic pedicle screws using neuronavigation. World Neurosurg 74(6): 606-610.
© 2018 Tanaka M. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






