- Submissions

Full Text
Perceptions in Reproductive Medicine
Every Child Comes with his or her Own Blessings: The Perceptions and Belief Systems of Indigenous Bakiga Men Regarding LARCs Use by their Rural Women
Kibonire RA* and Mphuthi DD
School of Social Sciences, College of Human Sciences, Department of Health Studies, University of South Africa, South Africa
*Corresponding author:Ronald Arineitwe Kibonire, School of Social Sciences, College of Human Sciences, Department of Health Studies, University of South Africa
Submission: November 20, 2023;Published: December 22, 2023

ISSN: 2640-9666Volume6 Issue1
Abstract
Worldwide complications associated with pregnancy, labour, and the postpartum period claim the lives of many women. Contraception, especially the use of Long-Acting Reversible Methods (LARCs), is one of the most effective interventions for reducing maternal mortality. LARCs aid in the postponement of pregnancy and allow for longer intervals between deliveries. However, the use of LARCs remains minimal globally and in Uganda due to male partners’ lack of acceptability. This qualitative study aimed to investigate the perceptions and belief systems of rural indigenous Bakiga Ugandan men regarding their rural women’s use of LARCs. The study was conducted in the districts of Rubanda, Uganda. Using purposeful sampling, the researcher selected 45 married males aged 20 to 49 for focus group interviews and 15 for individual interviews, for a total of 60 participants. For both individual and focus group interviews, the researcher employed semi-structured questions. Transcribing the interviews, organising the field notes, sorting and saving the data, listening to recordings, looking through the interviews and field notes, coding and categorising the data, and finally finding the emergent themes from the phenomena were all used to analyse the data.
According to these research findings, rural indigenous Bakiga Ugandan men’s perceptions, and belief systems regarding the use of LARCs by their rural wives served as obstacles to the method’s acceptance. Among the perceptions were low libido, effects on body organs, infertility, arm paralysis, adultery, difficulties with the removal and management of side effects, difficulties in feature deliveries, excessive weight gain, conceiving while on a method, the desire for balanced sex, and having the desired number of children. The research also found religious and cultural views as belief systems the men had. The study recommends creating an environment conducive to the provision of LARC services, policymakers and the ministry of education and sports should train pre-service and in-service healthcare personnel to provide LARC services. Other recommendations include enhancing social and behavioural change communication, improving service delivery for LARCs, and instituting robust monitoring and evaluation systems for LARCs
Keywords:Long-acting reversible contraceptive methods (LARCs); Beliefs; Perceptions; Indigenous Ugandan men; Rural
Abbreviations:LARC: Long Term Reversible Contraceptives; SSA: Sub-Saharan Africa; US: United States; IUDs: Intra-Uterine Devices; UNISA: University of South Africa; RDC: Resident District Commissioner; FGD: Focus Group discussion; I: Mean Individual Interviews; R: Refers to Participants from Rubanda District, Nyamweru Sub-County; RM: Means Participant from Rubanda District, Muko Sub-County; K: Refers to Participants from Kiboga District, Bukomero Sub-County; KD: Means Participant from Iboga District, Dwanilo Sub-Countys
Background
According to global estimates, 295,000 women died in childbirth in 2017 [1]. 86% of all recorded maternal fatalities occurred in Sub-Saharan Africa (SSA), where Uganda is located, and in southern Asia. SSA represented almost 66 percent of all maternal deaths [1]. In comparison, the United States had a maternal mortality rate of 17.9 per 100,000 women [2].
Worldwide, pregnancy and childbirth-related problems accounted for up to 75% of all maternal fatalities. These issues are brought on by extreme bleeding, usually after birth, infections, pre-eclampsia and eclampsia during pregnancy and delivery, and unsafe abortions [1]. Uganda has one of the highest rates of maternal death in sub- Saharan Africa, with 336 per 100,000 live births [3]. The maternal mortality rate in the Rubanda district, which is located in the Kigezi area of South-Western Uganda, is about 541 per 100,000 live births, which places it second only to the Karamoja region, where the rate is 580 per 100,000 live births [4]. To reduce maternal death rates, unwanted pregnancy prevention is essential. By making modern contraceptives, especially LARCs, more widely available, this approach reduces the unmet need for family planning [5].
The situation in Uganda
According to estimates, LARCs account for 21.4% of all family planning methods used in Uganda. while implants make up 17.3% and IUDs barely make up 4.0% [6]. This is because a significant percentage of rural Ugandan men disregard the use of LARCs [7] and [8]. According to reports, a lady in western Uganda was allegedly killed by her husband for using a LARC [9]. This occurrence mostly shows the undesirable beliefs and perceptions that exist towards LARCs in most parts of Uganda. The health of women and children born into large households is impacted by low LARC adoption. Uganda is a developing nation with few resources. Large families put pressure on the nation’s capacity to provide social services like health and education, lowering the quality of services the Ugandan government could offer to the general population. In order to come up with ways to boost LARC usage, this research attempted to provide a thorough knowledge of the belief systems of rural indigenous Ugandan males in relation to the use of LARCs.
Methodology
Design
The researcher collected constructive phenomenological qualitative data using a cross-sectional study methodology. An approach called phenomenology aims to comprehend people’s lived experiences and the meanings they take from those experiences [10].
The setting of the study
The rural districts of Rubanda and Kiboga, which are situated in the Kigezi, served as the study’s locations. These research sites were selected due to their remote locations, high fertility rates, and high rates of maternal death. The Rubanda district is found in the Kigezi area, which has a maternal death rate of 541/100,000 live births, a rural total fertility rate of 4.8%, and a LARC adoption rate of 14%. In comparison to the national average of 336 deaths per 100,000 live births, the maternal mortality rate in Kigezi is higher. LARC usage is lower than the expected national rate of 21.4% in Kigezi [6]. The focus group and individual interviews were conducted in both locations in order to find out the perceptions and belief systems of indigenous Ugandan men regarding LARCs.
Study participants
Indigenous married men from the Ugandan district of Rubanda, aged 20 to 49, made up the sample population [11]. The age range of 20 to 49 years was chosen because most men in Kigezi marry around the age of 20 and because most men in Uganda are very sexually active up to around the age of 49.
Sampling procedure
Purposive sampling was used to determine the sample size in this study [12]. For a total of 60 participants for individual and focus group interviews, the study’s sample included 60 individuals from the Rubanda district. data saturation determined the study’s sample size.
Data collection method
For face-to-face, in-depth individual and focus group interviews, data collection methods were utilised using open-ended interview guides with semi-structured questions. The researcher asked participants open-ended questions in order to extract an enormous amount of information [13]. The collection of data occurred in a natural environment, especially in open spaces at trade centre’s set up by the individual village leaders. Rukiga, the native language of the Rubanda people, was used to translate the interview questions. Interviews were taped and then transcribed.
Development of data collection tools
Instruments were developed before data was collected. These contained consent information sheets, informed consent forms, and open-ended focus group and individual interview guidelines [14]. Participants were permitted to speak freely on any subjects they felt important, using their own words and articulating their experiences in depth by utilising narratives, illustrations, and stories [10,15]. The Uganda National Council of Science and Technology gave final clearance after the AIDS Support Organisation, a local institutional review board in Uganda, and the University of South Africa’s ethical committee had all accepted the use of the questionnaires’ English and translated versions.
Selection of individuals
The researcher submitted permission requests to the Resident District Commissioners (RDCs) of Rubanda. The leaders facilitated the researcher’s efforts to secure venues for individual and focus group interviews as well as select participants based on inclusion criteria.
Interview process
Local indigenous leaders from two sub-counties recruited participants from the district of Rubanda. Concerns about ethics were reiterated in the Rukiga leaflets. Participants who gave written consent to participate in the study were interviewed individually and in focus groups. The saturation of the data determined the sample size, and the total number of participants in Rubanda district was 60. The data collection exercise lasted for 14 days. The researcher conducted interviews in Rukiga, the language spoken in the Rubanda district. The researcher asked perceptive questions to keep the conversation flowing and elicit topicspecific information [16]. The insightful questions elucidated the phenomenon of contraceptives, perceptions, and beliefs regarding LARCs. The researcher requested additional information from participants regarding the issue at hand [17]. After confirming that the participants had not provided any additional information, the researcher thanked them for their cooperation and concluded the interviews. Both the individual and focus group interviews were audio-recorded after obtaining participant consent. In addition, the researcher assured the participants that he would share the study’s findings with them once it was complete.
Data Analysis
The recordings of individual and focus group interviews were transcribed into text by listening intently and repeatedly in a calm, uncluttered atmosphere. The researcher carefully transcribed the interview recordings [18]. The researcher then used memoing, a method for recording what had been learned from the data, after transcription [16]. This was performed in order to guide the development of codes and sub-codes in order to follow the concepts and their relationships within the data. After memorization, the researcher manually categorised the data, checking for themes, concepts, and categories before marking segments of text that were comparable to one another [17,18]. Co-coding was also done with a researcher from one of the institutions doing research in Uganda. The three emergent themes were created by the researcher, and the consensus was then used to create categories and subcategories for each of the three themes. Structure, themes, and subthemes were provided by the Theories of Planned Behaviour (TPB) and Reasoned Action (TRA) to direct data analysis.
Result
Prolonged vaginal bleeding (Refer to Table 1)
Men stated that LARCs induce continuous vaginal haemorrhaging in women who use them, which was one of the reasons they did not support their partners’ use of the same contraceptive methods. In the citations that follow, participants provide their responses. “When our women use an implant or a capsule (IUD), they make them bleed non-stop. As a man, you can imagine what we feel spending a long time without touching your wife. I cannot allow my wife to use family planning method” (FGD R 7). I have heard that women who use capsules bleed nonstop and this can make them become very weak and unable to do work at home and in the garden (I RM 39). “A woman using a family planning method does not see the monthly periods and when they finally come, she will bleed for all the months she missed. This kind of bleeding can kill her and therefore I cannot allow my wife to use a LARC method (I K15)”.
Table 1:Summary of themes emerging from both focus group and individual interviews for Rubanda and Kiboga Districts.
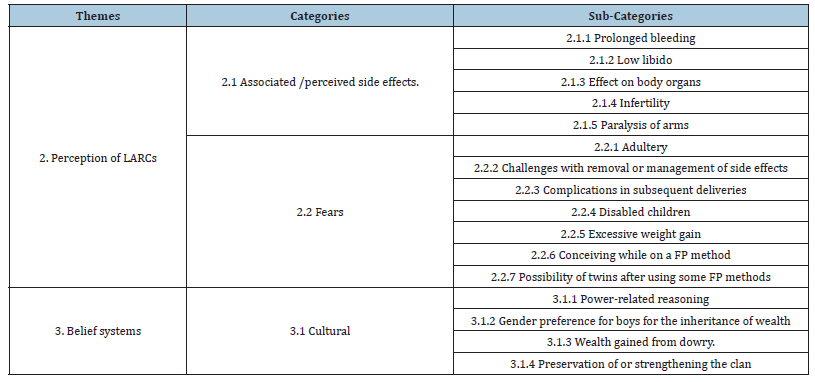
These findings are consistent with a study conducted in China by Luo et al. [19,20], which identified irregular vaginal bleeding as a significant barrier to LARCs adoption as it leaves men without intercourse for an extended period of time. The vast majority of men believed this and cited it as the reason why they did not recommend LARCs to their spouses. Approximately 20% of implant users experience amenorrhea, while up to 50% experience intermittent, regular, or protracted vaginal haemorrhage [21]. Users of Implanon are more likely to experience infrequent or no menstruation than irregular menstruation [22]. Users of IUDs may also experience protracted and excessive monthly bleeding or bleeding that occurs intermittently [23] (Table 1). Although protracted vaginal bleeding is a known adverse effect of LARCs, it can be effectively managed by service providers if the affected women visit a health care facility [22]. However, when males view LARCs as a method that will deprive them of sexual satisfaction, the majority of them cannot tolerate their wives using such a method. This may be the reason for the minimal use of LARCs in the two regions used as study contexts.
Source of labour for the family
According to indigenous bakiga men in Rubanda district, if the family has adequate land, the more children they have, the more labour they offer to the family for food production. As a result, several participants reported that they are opposed to their wives utilising LARCs since they take a long time, and they are unsure whether their ladies would produce again. They also said that this may lower their chances of having as many children as possible to supply labour for food production and income generation in the family. The following are some.
Quotes from participants: “If a family has many children and they go to cultivate, they dig a very big area for food production, and you will find such a family had enough food and money from selling excess food” (FGD R2). Families in Africa value having a large number of children as a source of labour, according to research conducted in Nigeria [24], which found that families wanted to have a large number of children to offer labour. This conclusion is supported by separate research conducted in Ethiopia, where several children were favoured as a source of labour for the family [25].
Expanding and strengthening the clan
In this subcategory (refer to Table 1 above), participants cited the need to expand and strengthen their lineages as the reason why they oppose their wives’ use of LARCs. Some participants from Rubanda claimed that a man’s greatness depends on how many children and spouses he has. The following quotations illustrate the perspectives of males from both the Rubanda and Kiboga districts. “I am from the Bahimba clan and in this area, we are only one family so men and my brothers need to produce many children to expand our clan so that when [we] are at the bar we are not overlooked and beaten. Therefore, we cannot allow our women to use long-acting family planning” (I R11) “I also have to be seen as contributing to expanding my clan and therefore it is not in order for my wife to use long-acting family planning. I will be considered a man when I have many boys to enlarge our clan” (FGD RM 22).
These assertions from indigenous men Rubanda District are supported by a study conducted in Ethiopia by [26], which found that cultural leaders opposed the use of family planning in favour of large family sizes to deal with inter-clan competition and other dynamics. The primary reason for not permitting their spouses to use LARCs is to increase the size of their clan. This is also supported by research conducted in Tanzania and South Africa, in which women reported that men do not want them to use modern contraceptives because they feel obligated to increase the size of their clan through procreation [27,28].
Paralysis of arm
The Bakiga indegenous men in Rubanda District cited arm paralysis as one of their concerns, causing them to oppose the use of LARCs by their women. Following are the statements of selected participants. “Like capsules when administered on the arm, some women complain of paralysis on several occasions” (FGD RM 3). “We have heard about women who used family planning of inserting in the arm and they [have] since failed to use the arm properly” (I RM 44). The fear of arm paralysis by men relates to the findings of a study conducted in Ethiopia [29], which revealed that some clients believed that LARCs could induce arm paralysis where the device is inserted. In a study conducted in Ethiopia [30], participants were also misinformed about paralysis; however, only women participated in this study, not men. In a separate study conducted in Papua New Guinea, Gupta et al. [31] found that men had heard rumours and false beliefs that women who use implants become extremely weak and unable to move their arms even after the implant is removed.
Expectation of wealth from dowries
Some people in the Rubanda District indicated that they didn’t want their wives to use LARCs because they needed dowries from their children. A number of the participants who took part said that when a family has a lot of girls and they all marry, the family gets a lot of cows in form of dowries and other things that add to their wealth. So, letting women use LARCs takes away the chance for families to have a lot of girls, which means less dowry in the future and less wealth for the family. “When I have many children especially girls and I am lucky they get married, I get cows and that is wealth in the family. So, if I allow my wife to use family planning, you cannot get enough girls and that means few cows” (FGD R9). “You know every child comes with his or her own blessing, there is therefore no need of limiting children and this also denies the family of wealth from cows if for example the girls get married”( I-R11). “If you produce many girls in the family and they become old, they will get married, and the family will get many cows and goats which are a source of wealth to the family. If the woman uses family planning, she will produce very few children and few cows” (I R 15).
A study by Harrington et al. [32] demonstrated that bride price obligations require women to have children and that using modern contraceptives is against social and cultural norms. This supports the idea that having a lot of girl children is a source of wealth. A South African study [28] found that some people in the Rubanda District thought that women should have a lot of children, both male and female, so that the gift could be paid back by marrying off the girl children.
Adultery
The indigenous Bakiga men believe that if their spouses use LARCs, they will not become impregnated as a result of extramarital sexual encounters, according to the findings of the current study. Therefore, participants from Rubanda District believed that LARCs could result in infidelity among women. The same assertion holds true for men who believe that, once their partners begin using LARCs, their diminished libido will cause them to seek satisfaction from other seductive women. According to the participants, this has led to both men and women contracting sexually transmitted infections, including HIV/AIDS. Below are some of the expressions of indigenous bakiga men. “Because the woman knows that she cannot be impregnated by another man when she goes out while using a long-term family planning method, this encourages her to continue cheating” (FGD R4). “Women who are using a long-acting family planning method, tend to be cheaters because they are not worried of being impregnated by other men. So, family planning encourages cheating, and I do not support it”(FGD RM 35).
This study’s findings regarding indigenous men’s fear of adultery are similar to those of a study conducted in Kenya by Obare et al. [33], in which participants disliked using contraceptives because they believed their partners were likely to accuse them of infidelity. In the same study, women feared that using contraceptives would encourage their male companions to engage in extramarital relations. Mwaisaka et al. [20] identified the fear of infidelity as well. Therefore, participants in the current study were hesitant to permit their wives to use LARCs to prevent infidelity and deception in their households. This finding from the Rubanda District is corroborated by a study by Bekele et al. [26], which found that permitting women to use contraceptives would make them healthier, more attractive, and more desirable to males. Due to this belief, men in the districts of Rubanda cannot permit their spouses to use LARCs.
Challenges with removal or management of side effects
Given that LARCs get inserted free of charge at health facilities, the participants in this study were concerned about their spouses using them. However, they are not assisted at the same health facilities when they experience complications while using the same techniques. They confirmed that healthcare providers at health facilities instruct LARC clients to wait for the individuals (organisations) who administer them. This is also true for women who desire LARC removal. As a consequence, males reported spending a significant amount of money to manage adverse effects and remove the devices from their partners. Participants, as a result, discouraged their spouses from using LARCs. “I cannot accept that my wife uses a capsule in the arm because when time for removing them comes, the health workers at the health centre cannot help as they want money” (I-RM 49). “Usually, women who get family planning services get them for free from Marie Stopes but when women get problems and they want to remove them, they cannot be helped by the health workers at the health centres. We end up spending a lot to remove them from private clinics” (FGD-RM 5).
It can be concluded that this practise leads to low adoption of LARCs if health care providers in health facilities are not adequately trained in the same contraceptive method. In South Africa, Adeagbo et al. [34] revealed that nurses lacked expertise in Implanon NXT removals, resulting in low adoption of the same method, which is similar to the finding presented above. In a study conducted in Kenya, women also confirmed that the lack of LARC removal services was an obstacle to the use of those contraceptive methods [35]. This could imply that women share the same concerns as their male partners, which all contribute to the low adoption of LARCs.
Excessive weight leads to less productivity
The Bakiga indigenous men in Rubanda district expressed caution that women who use LARCs will gain weight, develop mobility issues, and become incapacitated to perform household and gardening tasks. Men consequently believed that their women’s use of LARCs would lead to a lack of food at home and no one to do the tasks that women typically carry out. Men believe that the use of LARCs could increase their burden because their wives are less productive than they would be without these contraceptive methods. The majority of indigenous Bakiga men prefer their partners to use either short-term or natural contraceptives out of fear of extra responsibility. “Women who use long-acting family planning (LARCs) get excessive weight which leads to less productivity in doing chores and this makes men suffer with no one to do work of the woman at home” (FGD-RM 28). “When women use LARCs, they tend to be overweight leading to laziness at doing work at home” (FGD-RM 14) “I also here that family planning brings a lot of bleeding, and excessive weight gain making a woman unable to go and dig” (FGD R2).
Some studies indicate that some LARC users claim weight gain, whereas others indicate that there is no scientific link between LARC use and weight gain. According to some research, there is no causal relationship between the use of implants and IUDs and weight gain [21]. Romano & Braun-Courville [36] demonstrated in a similar study that the ENG Long-Acting Implant does not induce weight gain. Nonetheless, a study [37-39] found that ENG implant and hormonal IUD recipients gained weight, but Cupper IUD users did not. The perceived reason for weight gain among women using LARCs may be a supposition based on the fact that women are at ease knowing they will not have unintended pregnancies.
Conceiving while using a LARC
The indigenous Bakiga men in the Rubanda District were also concerned about the alleged ineffectiveness of LARCs, citing the fact that women continue to become pregnant despite their use. Furthermore, participants stated that the methods are ineffective and have adverse health effects on the body, including on expectant babies. Men believed that infants conceived while their mothers were using LARCs might be born with malformations and disabilities. As a consequence, the indigenous Bakiga men and their spouses choose short-term contraceptive methods, such as three-month injectables, tablets, and natural methods, rather than LARCs. Below are some quotes from the participants. “Some women produce twins after using some long-acting family planning methods yet there is no history of twins in the family” (FGD-RM 17). “Men as a man, I cannot support my wife to use a long-term family planning method because she might produce many children at ago’’ (I-RM 44).
In accordance with WHO/RHR & CCP [22], LARCs are the most efficient contraceptive methods, with a failure rate of 0.0005% (5 pregnancies per 10,000) for implants compared to fewer than one pregnancy per 100 women using an IUD (6 to 8 pregnancies per 1,000 women). Due to drug interactions, a number of implant failures have been reported in women taking Rifampicin for tuberculosis and antiretroviral medications like efavirenz for the treatment of HIV/AIDS [40-42]. Similar failure rates were discovered in other studies, as reported by participants. In a study conducted in the United States, the rate of failure for LARCs was determined to be 0.2% [43], whereas the failure rate for implants in Ghana was 0.5% [44]. Implants and IUDs are not linked to birth defects, according to the scientific literature [22]. According to the WHO’s failure rate estimates, the failure rate among LARC consumers is negligible. Therefore, it is possible that what the participants said was inaccurate.
Power-relations between men and women
Power relations are defined as the capacity to influence the behaviour of another individual [45]. The indigenous Bakiga men in Rubanda District believed that a man is the leader of the household and has the final say on whether or not his spouse ought to utilise LARCs. Since men have their own concerns and beliefs about the use of LARCs, they often prevent their spouses from using the methods to demonstrate their authority in the household. Some men indicated that if women obtain LARCs without first getting permission from them, they must return the women to the health facilities to be removed because they did not give permission for the women to obtain these contraceptive methods. Below are some excerpts from the participants’ opinions.
“As a man, I am the head of the family, and I am supposed to be the one to allow my wife to use or not use a contraceptive method” (FGD-R 5). “You see women escape and go to put that family planning thing without telling us, men. So, to avoid problems that come with the use of those family planning methods I have to take mine back to the facility to remove it. I should be in the know before she uses any family planning method” (FGD RM 46). The results of this study, based on the submissions, are comparable to those of Augustine and Godwin [46], who revealed that due to the dominance of men, women often have no say in the use of contraceptives. Studies conducted in Papua New Guinea, South Africa, and Nigeria [24,28,31] found that women are obligated by culture to seek consent from their spouses before utilising implants. In some instances, men damage LARCs to render them ineffective or even forcibly remove them from their companions [28]. All the above demonstrates the dominance of males over their spouses, particularly in rural settings like Rubanda district.
Summary of the Findings
Based on the findings of this study, it can be concluded that indigenous Bakiga men from Rubanda district have perceptions and belief systems about the use of LARCs by their rural women. These perceptions act as barriers to acceptability and support for LARCs by indigenous Bakiga men. The perceptions and belief systems include prolonged vaginal bleeding, children as a source of labour for the family, paralysis of the arm as a result of LARCs use, and the expectation of acquiring wealth from Dowries. More to that, the indigenous Bakiga men fear adultery as a result of their wife’s use of LARCs, challenges with the removal or management of side effects, and excessive weight gain that leads to less productivity among women. In addition, some men feared that their women could still conceive even when they were using LARC. Male dominance in decision-making in the home was also cited as one of the perceptions hindering indigenous Bakiga men’s acceptance of LARCs use by their rural women [47].
Recommendations
The study recommends that there should be efforts to increase knowledge of family planning and LARCs, among the indigenous Bakiga men in Rubanda district. This should be done using satisfied men users, trained cultural and religious leaders, and radio programmes, both the community and conventional ones. In addition, there is a need for capacity building of health workers on LARC insertions, removals, and management of side effects, right from the health centre IIs to the hospital level, to improve access to those services. Once the indigenous Bakiga men have adequate knowledge about LARCs, their negative perceptions and belief systems are likely to change to more positive ones. This could lead to increased support for LARC use among rural women. In addition, the improvement in the provision of LARC services, especially at the lower health facilities, could make them more attractive, especially if health workers are able to offer LARC insertion and removal services as well as manage the related side effects.
Conclusion
To address the perceptions and belief systems of indigenous rural Bakiga men, the implementation of recommendations should be adopted. The researcher assumes that once men and the entire community have correct information about LARCs and quality LARC services available and offered within reach of rural women, the support of indigenous Bakiga men towards LARC use will increase. This will most likely result in increased use by their rural women.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with relevant guidelines and regulations as provided for in the Declaration of Helsinki. The study was approved by the Department of Health Studies at the University of South Africa, the Ugandan Institutional Review Board (IRB), the AIDS Support Organisation Uganda (TASO) and then from the Uganda National Council for Science and Technology (UNCST) for the final clearance for data collection. Informed consent was obtained from all the participants.
Consent for publication
The researchers obtained written consent to use quotes from participants in publications.
Availability of data and materials
The primary study document contains all the necessary detailed information and data set used and analyzed during this study. It is available upon an appropriate request from the corresponding author.
Funding
This work was supported by University of South Africa through Masters and Doctoral Bursary awarded to the researcher.
Authors’ Contributions
Ronald Arineitwe Kibonire
Developed the study concept, the study design, data collection, analysis and interpretation, prepared the manuscript, and read the paper. He is the principal investigator for the study.
David ditaba mphuthi
As the supervisor for the researcher and provided guidance at every stage during the conception of the study, study design, data collection and analysis and reviewed the manuscript and provided feedback for refining. He was the co-investigator on this study.
Availability of data and materials
The primary study document contains all the necessary detailed information and data set used and analyzed during this study. It is available upon an appropriate request from the corresponding author.
Acknowledgement
The authors thank Rubanda who participated in the study. We also thank the Office of Resident district commissioners through the District Health Officers in Rubanda that granted permission to conduct the research in the district. Special thanks go to the staff of the District Health Office that helped in coordinating and mobilizing the participants for the study.
Ethics approval numbers
UNISA: NHRE REG NO: Rec-240816-052 TASO: TASO-2021-56 UNCST: REF- HS2152ES.
References
- (2019) Trends in maternal mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United, Geneva: World Health Organization.
- Hawkins SS, Ghiani M, Harper S, Baum CF, Kaufman JS (2020) Impact of state-level changes on maternal mortality: A population-based, quasi-experimental study. Am J Prev Med 58(2): 165-174.
- Uganda Bureau of Statistics (UBOS) and ICF, (2018) Uganda demographic and health survey 2016, Kampala, Uganda and Rockville, Maryland, USA: UBOS and ICF.
- Uganda Bureau of Statistics (2017) the national population and housing census 2014-health status and associated factors. Thematic Report Series, Kampala Uganda: UBOS.
- World Health Organization (2015) Strategies toward ending preventable maternal mortality (EPMM) World Health Organisation, Geneva, Switzerland.
- FP2020 (2020) Core Indicator Summary Sheet: 2019-2020 Annual progress report.
- UNFPA (2020) Population Matters (2021) The Journey towards achieving zero unmet need for modern family planning: Re-evaluating Uganda’s efforts, Kampala: UNFPA, p. 4.
- Monitor (2021) Implants in untold places: Gulu’s family planning dilemma.
- Muhimba S (2022) Nile post, Uganda.
- Leavy P (2017) Research design: Quantitative, qualitative, mixed methods, arts-based, and community-based participatory research approaches. (1st edn). The Guilford Press, New York, USA.
- The World Bank (2022) Indigenous peoples overview.
- Pope C, Mays N (2020) Qualitative Research in Health Care, (3rd edn). John Wiley & Sons Ltd, Oxford, UK.
- Williman N (2018) Research Methods: The Basics, (2nd edn). Routledge, New York, USA.
- Sekaran U, Bougie R (2016) Research methods for business: A skill-building approach. (7th edn). John Wiley & Sons Ltd, West Sussex, USA.
- Cohen L, Manion L, Morrison K (2018) Research methods in education, (8th edn). Routledge, New York, USA.
- Biber SNH (2017) The Practice of Qualitative Research. (3rd edn). SAGE Publications, Inc, California, USA.
- Nieswiadomy RM, Bailey C (2018) Foundations of Nursing Research. (7th edn). Pearson Education, Inc, Boston, USA.
- Edmonds WA, Kennedy TD (2017) An applied guide to research designs: Quantitative, qualitative, and mixed methods. (2nd edn). SAGE Publications, Inc, California, USA.
- Luo Z, Gao L, Anguzu R, Zhao J (2018) Long-acting reversible contraceptive use in the post-abortion period among women seeking abortion in mainland China: Intentions and barriers. Reproductive Health 15(85): 1-9.
- Mwaisaka J, Gonsalves L, Thiongo M, Waithaka M, Sidha H, et al. (2020) Exploring contraception myths and misconceptions among young men and women in Kwale County, Kenya. BMC Public Health 20(1694): 1-10.
- Melville C (2015) Sexual and Reproductive Health at a Glance. (1st edn). John Wiley & Sons Ltd, Chichester, USA.
- WHO/RHR & CCP (2018) Family Planning: A Global Handbook for Providers, Baltimore and Geneva: CCP and WHO, Switzerland.
- Casanova R, Chuang A, Goepfert AR, Hueppchen NA, Weiss PM (2019) Beckmann and Ling's Obstetrics and Gynaecology. (8th edn). Wolters Kluwer, Chennai, India.
- Akamike IC, Madubueze UC, Alex INO, Anyigor CJ, Azuogu BN, et al. (2020) Perception, pattern of use, partner support and determinants of uptake of family planning methods among women in rural communities in Southeast Nigeria. Contraception and Reproductive Medicine 5(14): 1-8.
- Endriyas M, Eshete A, Mekonnen E, Misganaw T, Shiferaw M (2018) Where we should focus? Myths and misconceptions of long-acting contraceptives in Southern Nations, nationalities and people's region, Ethiopia: Qualitative study. BMC Pregnancy and Childbirth 18(98): 1-6.
- Bekele D, Surur F, Nigatu B, Teklu A, Getinet T, et al. (2021) Contraceptive prevalence rate and associated factors among reproductive age women in four emerging regions of Ethiopia: A mixed method study. Contraception and Reproductive Medicine 6(18): 1-13.
- Kassim M, Ndumbaro F (2022) Factors affecting family planning literacy among women of childbearing age in the rural Lake zone, Tanzania. BMC Public Health 22(646): 1-11.
- Kriel Y, Milford C, Cordero J, Suleman F, Beksinska M, et al. (2019) Male partner influence on family planning and contraceptive use: Perspectives from community members and healthcare providers in KwaZulu-Natal, South Africa. Reproductive Health 16(89): 1-15.
- Tebeje B, Workneh D (2017) Prevalence, perceptions and factors contributing to long-acting reversible contraception use among family planning clients, jimma town, oromiya region, South-West Ethiopia. Women's Health Care 6(1): 1-10.
- Obsa MS, Takiso KT, Ayele TT, Koyra HC, Hidoto KT, et al. (2021) Lived experience of women who underwent early removal of long-acting family planning methods in bedesa town, wolaita zone, Southern Ethiopia: A Phenomenological Study. International Journal of Women’s Health 13: 645-652.
- Gupta S, Bernays S, Black KI, Ramsay P, Bolnga J, et al. (2020) Community attitudes and gendered influences on decision making around contraceptive implant use in rural Papua New Guinea. Reproductive Health 17(136): 1-13.
- Harrington R, MacLaren RM, Harvey N, Puia M, et al. (2020) Barriers and enablers to using contraceptives for family planning at Atoifi Hospital, East Kwaio, Solomon Islands. Pacific Journal of Reproductive Health 1(10): 586-597.
- Obare F, Odwea G, Cleland J (2020) Men’s needs and women’s fears: Gender-related power dynamics in contraceptive use and coping with consequences in a rural setting in Kenya. Culture, Health & Sexuality 23(12): 1748-1762.
- Adeagbo O, Mullick S, Pillay D, Chersich M, Morroni C, et al. (2017) Uptake and early removals of implanon NXT in South Africa: perceptions and attitudes of healthcare workers. S Afr Med J 107(10): 822-826.
- Britton LE, Williams CR, Onyango D, Wambua D, Tumlinson K (2021) When it comes to time of removal, nothing is straightforward: A qualitative study of experiences with barriers to removal of long-acting reversible contraception in Western Kenya. Contraception X 3(100063): 1-11.
- Romano ME, Courville DKB (2019) Assessing weight status in adolescent and young adult users of the etonogestrel contraceptive implant. Journal of Pediatric and Adolescent Gynecology 32(4): 409-414.
- Lazorwitz A, Dindinger E, Harrison M, Aquilante CL, Sheeder J, et al. (2019) Influence of genetic variants on weight gain among etonogestrel contraceptive implant users. Fertility and Sterility 112(3): e9-e10.
- Edwards AJ, DiVasta AD, Pitts S (2020) Long-acting reversible contraception side effect management. Current Opinion in Paediatrics 32(4): 461-470.
- Beksinska M, Issema R, Beesham I, Lalbahadur T, Thomas K, et al. (2021) Weight change among women using intramuscular depot medroxyprogesterone acetate, a copper intrauterine device, or a levonorgestrel implant for contraception: Findings from a randomised, multicentre, open-label trial. E Clinical Medicine 34(100800): 1-9.
- Surya R, Kusnawara Y (2020) Alert in contraceptive implant failure: A Case Report. Obstetrics and Gynecology Case Report Jakarta, Indonesia.
- Kreitchmann R, Stek A, Best BM, Capparelli E, Wang J, et al. (2022) Interactions between etonogestrel-releasing contraceptive implant and 3 antiretroviral regimens. Journal of Contraception 105: 67-74.
- Pfitzer A, Wille J, Wambua J, Stender SC, Strachan M et al. (2020) Contraceptive implant failures among women using antiretroviral therapy in western Kenya: A retrospective cohort study. Gates Open Research 3(1482): 1-25.
- Moray KV, Chaurasia H, Sachin O, Joshi B (2021) A systematic review on clinical effectiveness, side-effect profile and meta-analysis on continuation rate of etonogestrel contraceptive implant. Reproductive Health 18(4): 1-24.
- Bawah AA, Sato R, Asuming P, Henry EG, Agula C, et al. (2021) Contraceptive method use, discontinuation and failure rates among women aged 15-49 years: Evidence from selected low-income settings in Kumasi, Ghana. Contraception and Reproductive Medicine 6(9): 1-10.
- Lindsey LL (2016) Gender Roles: A sociological perspective. (6th edn). Routledge, New York, USA.
- Augustine AO, Godwin OG (2018) Gender inequality on contraceptive use among young married couples in Benin City, Nigeria. FULafia Journal of Social Sciences 1(4): 1-11.
- Uganda Bureau of Statistics, (2017) The national population and housing census 2014-health status and associated factors. Thematic Report Series, Kampala Uganda: UBOS.
© 2023 Ronald Arineitwe Kibonire. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






