- Submissions

Full Text
Perceptions in Reproductive Medicine
Birth Weight and Neurodevelopment Outcome in Singleton Babies: A Comparison between Assisted Reproductive Techniques and Control Group
Mahbod kaveh1, Zahra Kaveh2, Tanha FD3*, Roya hamrahi4, Mahboubeh shirazi5, Maryam veisizadeh4, Mamak shariat4 and Zahra shahraki6
1Department of neonatology, Bahrami hospital, Tehran university of medical sciences, Tehran, Iran
2Research center of Yas hospital, Tehran university of medical sciences, Tehran, Iran
3Department of obstetrics and gynecology, Yas hospital, Tehran university of medical sciences, Tehran, Iran
4Maternal, fetal and neonatal research center, Valiasr Hospital, Iran
5Maternal fetal and neonatal research center, Tehran university of medical sciences, Tehran
6Department of obstetrics and gynecology, Zabel university of medical sciences, Iran
*Corresponding author: Tanha FD, Department of obstetrics and gynecology, Yas hospital, University of medical sciences, Tehran, Iran
Submission: January 27, 2023;Published: February 17, 2023

ISSN: 2640-9666Volume5 Issue4
Abstract
Objective: This study examined the birth weight of singleton babies born after assisted reproductive
techniques and their neurodevelopment outcome until the sixth month of birth in comparison with the
singleton babies born without infertility treatment.
Study design: Prospective case-control study
Setting: University-based hospitals. four hundred patients were enrolled in the study. Two hundred were
in control group without infertility and two hundred with infertility treatment as case group
Main outcome measure(s): mean weights at birth, at the third and the sixth month and developing.
Examination results: The mean Birth Weights (BW) of infants of the case group and those infants of the
control group were 2998.97g±305.93 and 3245.82 g±414.58 respectively. The difference between groups
was statistically significant (p=0.001). Neurodevelopment delay occurred in infertility group, like the
ability to recognize bottle and breast at the third month and the ability to reach the mouth by the leg and
roll and sit alone at the sixth month. It seems that lower birth weight is associated with some retardation
in neurodevelopment function of infertility group’s infants.
Conclusion: Singleton pregnancy infants who were born after assisted reproductive techniques had lower
birth weight than those without background of infertility treatment. This difference may have some effects
on their neurodevelopmental ability.
Keywords: Birth weight; Neurodevelopment outcome
Introduction
Infertility is defined as the failure to have pregnancy after one year of regular Intercourse without contraception [1]. Poor obstetrics outcomes are common in babies born after assisted reproductive technologies. Infertility or treatment for poor pregnancy outcome is not clear. Babies who were born with low- or very low- birth weights had a higher risk of neonatal mortality [2]. Infants born after In Vitro Fertilization (IVF) are lighter than those born after frozen-embryo transfer [3]. Actually, these neonates are large at gestational age in comparison to naturally conceived babies. All types of reproductive methods increase the risk of still birth [4] preterm labor and low birth weight was seen in Infertile couples who conceive a baby after one year [5-15]. Authors concluded that babies born after Intra-Cytoplasmic Sperm Injection (ICSI) with extracted or ejaculated testicular sperm with extreme Oligoasthenospermia show no sign of developmental problems and their clinical outcome is the same [10]. This study examined the birth weight of singleton babies born after assisted reproductive technologies and their neurodevelopment outcome until the sixth month of birth in comparison with the singleton babies born without infertility treatment.
Methods and Materials
This is a prospective case-control study. Infertile and fertile women were enrolled in the study since March 2011 until February 2014 from two university-based hospitals. The study was approved by the ethical committee of Tehran University of Medical Sciences and all participants signed the informed consent before entering the study. Inclusion criteria for the case group included ages 18- 40, first singleton pregnancy, gestation age of below thirty-five weeks, no background of underlying disease or diabetes and preeclampsia, a background of one year or more of infertility for those who had pregnancy with assisted reproductive techniques. The control group had the same criteria except infertility. Four hundred patients were enrolled in the study. Two hundred were in the control group without infertility and two hundred with infertility treatment as case group. The following factors were taken in consideration in this article: age and Body Mass Index (BMI) of mothers, background of miscarriage, duration of infertility, type of assisted reproductive techniques, background of polycystic ovarian syndrome, endometriosis, male factor infertility, type of pregnancy termination, gestational age, infant gender, birth weight and height, APGAR score, days of Neonatal Intensive Care Unit (NICU) admission, head circumference at birth and three and six months after that and evaluation of neurodevelopment by Developmental Diagnosis-Normal and Abnormal Child Development-Clinical Methods and Pediatric Applications (Gesell and Amatruda1941). The qualitative variables were analyzed using Chi 2 and student’s T-test was used to analyze the quantitative data. (CI=95%; P<0.05) The data were analyzed using SPSS18.
Result
The mean Birth Weights (BW) of infants in the case and control groups were 2998.97g±305.93 and 3245.82 g±414.58 respectively. The difference between groups was statistically significant (p=0.001). The mean Birth Heights (BH) of infants in the case group and those in the control group were 48.47cm±2.38 and 49.61cm±2.31 respectively. The difference between groups was statistically significant (P=0.001) The mean weights of infants three months after birth were 5689.11g ±880.34 and 6107.82 g±896.47 in case and control groups respectively (p=0.003). The mean head circumferences at birth in the case and the control group were 34.87cm±1.6 and 34.8cm±1.51 respectively. Three and six months after birth, the mean head circumferences in the case group were 40.39cm±2.28 and 44.02cm ±2.55 respectively; and in the control group, the mean head circumferences at the third and the sixth month of birth were 40.48±1.94 and43.71±2.37 respectively. The differences between head circumferences at birth, at the third and the sixth month were not statistically significant between groups (p=0.672).
Table 1: Results of the weight, height and head circumference at birth and three and six months after birth.
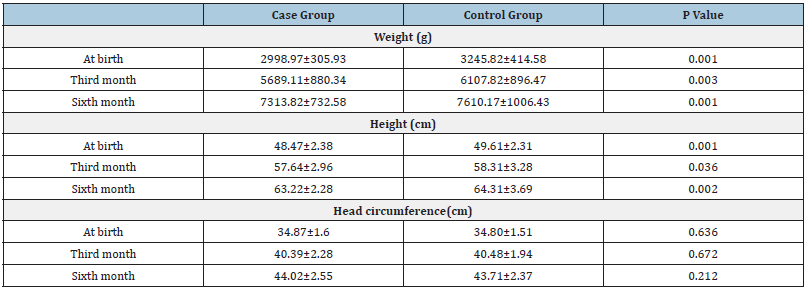
Case Group: infertile group; Control Group: fertile group
Table 2: Third month neurodevelopment outcome.
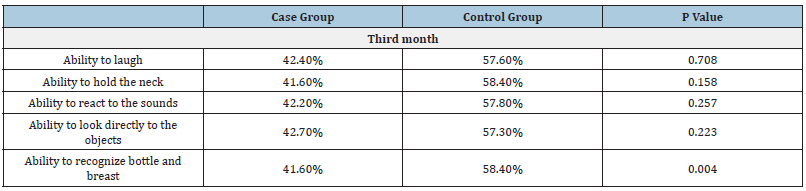
Case Group: infertile group; Control group: fertile group
The results are reported as frequency (percentage); P<0/05 is statistically significant
Table 3: Sixth month neurodevelopment outcome.
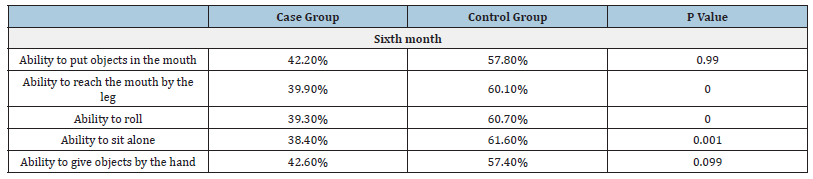
Case Group: infertile group; Control group: fertile group The results are reported as frequency (percentage); P<0/05 is statistically significant
Table 1 shows the result of the weight, height and head circumference at birth and three and six months after birth. The ability to laugh and hold the neck (p=0.158) and react to the sounds (p=0.162) and look directly to the objects (p=0.223) at the third month was the same in both groups. The ability to recognize bottle and breast (p=0.004) was different at the third month in the two groups. But after six months, both groups’ babies acted similarly in to recognize bottle and breast. The ability to put objects in the mouth at the sixth month was the same in the two groups. However, at the sixth month, the ability to reach the mouth by the leg and roll and sit alone had retarded in the infertility group compared to the control group (p=0.001), but the ability to give objects by the hand was the same in both groups (p=0.09). Table 2 & 3 show neurodevelopment outcome The head circumferences at birth in Intrauterine Insemination (IUI) and ICSI groups were 35.26±1.29cm and34.5±1.68cm respectively; the difference was statistically significant (p=0.001).
The mean birth heights in IUI and ICSI groups were 48.22±1.87cm and 48.69±2.92cm respectively. (p=0.178) The birth weights in IUI and ICSI groups were 3019.75±275.76g and 3003.5±363.8g respectively. (p=0.716) The mean birth heights in IUI and ICSI groups at the third month were 57.09±2.59cm and 57.93±3.5cm respectively (p=0.055). The mean head circumferences at the third month were 40.63±1.76cm and 40.21±2.68cm respectively. (p=0.198) The mean weights at the third month in IUI and ICSI groups were 5864.5±811.88g and 5489±933.37g respectively (p=0.003). The mean heights at the sixth month in IUI and ICSI groups were 62.57±2.59cm and 63.93±3.29cm (p=0.001). The mean head circumference at the sixth month in IUI and ICSI groups were 44.25±2.38cm and44.01±2.12cm respectively (p=0.542). The mean weights at the sixth month in IUI and ICSI groups were 7397.5±590.68g and 7236.5±907.54g respectively (p=0.139).
Discussion
Some neurodevelopment delay occurred in infertility group, like the ability to recognize bottle and breast at the third month and the ability to reach the mouth by the leg and roll and sit alone at the sixth month. Several studies have been carried out on the birth weights of singleton pregnancy infants after infertility treatment. Authors (2011US) did researches on 1264 women without and 461 women with background of infertility and singleton pregnancy and reported that infants of the infertility group were lighter than the others, but there were no Information infants’ heights or head circumferences or neurodevelopment [11].
It seems that lower birth weight is associated with some retardation in neurodevelopment function of infertility group’s infants. In this study, birth weight and developing examination of mothers with singleton pregnancy after infertility treatment and those without infertility treatment had been developed. There were four hundred infants divided into two groups. The mean birth weight and those of the third and the sixth months in the case group were lower than those in the control group and the differences were statistically significant.
In study on 16748 infertile women, 920 cases were under assisted reproductive techniques treatment; 904 cases underwent medical treatment and 14673 cases received no treatment. Infants of the ART group were reported to be at a higher risk of poor obstetric outcomes like low-and very low birth weight [12]. In a study, on low birth weight and preterm labor in 144018 mothers (in vitro fertilization cycles) it was demonstrated the risks of low birth weight and preterm labor were higher in women who used donated cycles [13]. In our study, it was demonstrated that mean birth height and those of the third and the sixth months in the case group were lower than those in the control group and the differences were statistically significant. However, the head circumferences were similar at birth and at the third and the sixth months. In our study, it was demonstrated that examination of birth heights and weights of the infants of both groups showed that the height and weight growths of infertile mothers’ infants were lower than the ones of the other group’s infants at birth, at the third and at the sixth month.
On the other hand, the quality of movements in three-monthold infants born of mothers with background of infertility is lower than those of fertile mothers [16]. Stromberg’s research examined 5,680 babies born by IVF and 11,360 babies conceived naturally and reported that the risk of neurological disability requiring rehabilitation was higher in the ART group [17] in one study, 81 babies born by the ART methods with 85 babies born by naturally conceived pregnancies and found that the minor neurological dysfunction is more likely in the ART group [18]. Everything that disturbs the growth of the neonate, causes weight loss and if continues, results in short stature, and at the end, affects the head circumference. At this study, the infertility group’s infants had lower weights and the differences at the statures were significant. Revealed growth retardation, preterm birth, cerebral palsy in one year in infants attributed to the ART induced pregnancies [19] and also, IVF babies got lower scores on a test of moving quality than the natural group babies [20]. Kelly-Vance L et al. [21] reported lower psychomotor development in children born by ART than in naturally conceived children [21]. Some studies reported that IVF risk of neurological and behavioral development problems in the first year of life [22,23] the treatment of this condition causes is not clear, but regarding the etiology, retardation effect can be happened until sixth month.
Conclusion
However, the difference between head circumference growth was not significant. Neurodevelopmental abilities like grasping, recognizing bottle and breast, reaching the mouth by the leg, putting objects in the mouth and reacting to sounds had significant differences in the two groups, whereas other abilities did not differ significantly. However, the ability to sit alone was different at the sixth month and needed to be examined at the ninth month. Singleton pregnancy infants who are born after assisted reproductive techniques are lighter at birth than those without background of infertility treatment. This difference may have some effects on their neurodevelopmental ability. We recommend a large study with longer follow-up duration for examining this aspect of infant development for babies who are born after assisted reproductive techniques. Conflict of interest: There is no conflict of interest in this study. All authors have contributed significantly.
Acknowledgement
This study was sponsored by deputy research of Tehran University of Medical Sciences
We have financial support of Tehran University of Medical Sciences (tums).
References
- Practice Committee of American Society for Reproductive Medicine (2008) Definitions of infertility and recurrent pregnancy loss. Fertil Steril 90(5): S60.
- Jackson RA, Gibson KA, Wu YW, Croughan MS (2004) Perinatal outcomes in singletons following in vitro fertilization: A meta-analysis. Obstet Gynecol 103(3): 551-563.
- Barnhart KT (2013) Assisted reproductive technologies and perinatal morbidity: Interrogating the association. Fertil Steril 99(2): 299-302.
- Wisborg K, Ingerslev HJ, Henriksen TB (2010) IVF and stillbirth: A prospective follow-up study. Hum Reprod 25(5): 1312-1316.
- Jaques AM, Amor DJ, Baker HW, Healy DL, Ukoumunne OC, et al. (2010) Adverse obstetric and perinatal outcomes in sub fertile women conceiving without assisted reproductive technologies. Fertil Steril 94(7): 2674-2679.
- Marino JL, Moore VM, Willson KJ, Whitrow MJ, Giles LC, et al. (2014) Perinatal outcomes by mode of assisted conception and sub-fertility in an Australian data linkage cohort. PLoS One 9(1): e80398.
- Wisborg K, Ingerslev HJ, Henriksen TB (2010) In vitro fertilization and preterm delivery, low birth weight and admission to the neonatal intensive care unit: A prospective follow-up study. Fertil Steril 94(6): 2102-2106.
- De Geyter C, De Geyter M, Steimann S, Zhang H, Holzgreve W (2006) Comparative birth weights of singletons born after assisted reproduction and natural conception in previously infertile women. Hum Reprod 21(3): 705-712.
- Davies MJ, Moore VM, Willson KJ, Van Essen P, Priest K, et al. (2012) Reproductive technologies and the risk of birth defects. N Engl J Med 366(19): 1803-1813.
- Tsai CC, Huang FJ, Wang LJ, Lin YJ, Kung FT, et al. (2011) Clinical outcomes and development of children born after Intra Cytoplasmic Sperm Injection (ICSI) using extracted testicular sperm or ejaculated extreme severe oligo-astheno-teratozoospermia sperm: A comparative study. Fertil Steril 96(3): 567-571.
- Cooper AR, O Neil KE, Allsworth JE, Jungheim ES, Odibo AO, et al. (2011) Smaller fetal size in singletons after infertility therapies: The influence of technology and the underlying infertility. Fertil Steril 96(5): 1100-1106.
- D Angelo DV, Whitehead N, Helms K, Barfield W, Ahluwalia IB (2011) Birth outcomes of intended pregnancies among women who used assisted reproductive technology, ovulation stimulation or no treatment . Fertil Steril 96(2): 314-320.
- Nelson SM, Lawlor DA (2011) Predicting live birth, preterm delivery and low birth weight in infants born from in vitro fertilization: A prospective study of 144,018 treatment cycle. PLoS Med 8(1): e1000386.
- Pelinck MJ, Keizer MH, Hoek A, Simons AH, Schelling K, et al. (2010) Perinatal outcome in singletons after modified natural cycle IVF and standard IVF with ovarian stimulation. Eur J Obstet Gynecol Reprod Biol 148(1): 56-61.
- Allen C, Bowdin S, Harrison RF, Sutcliffe AG, Brueton L, et al. (2008) Pregnancy and perinatal outcomes after assisted reproduction: A comparative study Ir J Med Sci 177(3): 233-241.
- Middelburg KJ, Haadsma ML, Heineman MJ, Bos AF, Hadders-Algra M (2010) Ovarian hyperstimulation and the in vitro fertilization procedure do not influence early neuromotor development; a history of subfertility does. Fertil Steril 93(2): 544-553.
- Strömberg B, Dahlquist G, Ericson A, Finnström O, Köster M, et al. (2002) Neurological sequelae in children born after in-vitro fertilization: A population based study. Lancet 359(9305): 461-465.
- Knoester M, Vandenbroucke JP, Helmerhorst FM, van der Westerlaken LA, Walther FJ, et al. (2007) Matched follow-up study of 5-8 year old ICSI singletons: Comparison of their neuromotor development to IVF and naturally conceived singletons. Hum Reprod 22(6): 1638-1646.
- Wadhawan R, Oh W, Perritt RL, McDonald SA, Das A, et al. (2009) Twin gestation and neurodevelopmental outcome in extremely low birth weight infants. Pediatrics 123(2): e220-e227.
- La Sala GB, Gallinelli A, Fagandini P, Bevolo P, Landini A, et al. (2004) Developmental outcomes at one and two years of children conceived by intra cytoplasmic sperm injection. Int J Fertil Women’s Med 49(3): 113-119.
- Kelly-Vance L, Anthis KS, Needelman H (2004) Assisted reproduction versus spontaneous conception: A comparison of the developmental outcomes in twins. J Genet Psychol 165(2): 157-167.
- Ludwig AK, Sutcliffe AG, Diedrich K, Ludwig M (2006) Post-neonatal health and development of children born after assisted reproduction: A systematic review of controlled studies. Eur J Obstet Gynecol Reprod Bio 127(1): 3-25.
- Wagenaar K, Huisman J, Cohen-Kettenis PT, de Waal HA (2008) Overview of studies on early development, cognition, and psychosocial well-being in children born after in vitro J Dev Behav Pediatr 29(3): 219-230.
© 2023 Tanha FD. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






