- Submissions

Full Text
Perceptions in Reproductive Medicine
Supernumerary Breast: About an Uncommon Case Report
Mariam M1*, Khaoula L1, Oumaima S1, Aziz S2, Najia Z1, Amina L1, Aicha K2 and Abdelaziz B1
1Department of Gynecology-Obstetrics and Endoscopy, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco
2Department of Gynecology-Obstetrics and Endocrinology, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco
*Corresponding author:Mariam M, Department of Gynecology-Obstetrics and Endoscopy, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco
Submission: January 13, 2023;Published: January 24, 2023

ISSN: 2640-9666Volume5 Issue4
Background
Supernumerary breasts or polymastia is a moderately common congenital condition of abnormal accessory breast tissue in addition to normal breast tissue. Between 1% and 5% of men and women have this condition. the most common site for accessory nipples is just below the normal breast, and the most common site for accessory breast tissue is the lower axilla. This condition reacts as normal breast tissue, and present the same diseases as a normal breast, need to be followed up for diseases, as in a normal breast. The diagnosis is often discovered incidentally and the management of these condition is essentially surgical and recommended at any age found. We present a rare case of bilateral axillary supernumerary breasts in a 26-year-old woman who had a chronic bilateral axillary lymphadenopathy developing since puberty and worsening with pregnancy and lactation, which strongly reinforces the diagnosis. Underwent excision surgery and the anatomopathological study confirmed the diagnosis of supernumerary breasts with absence tumor cells. Through this case report we will describe the pathological and management aspects of polymastia as rare diagnosis.
Keywords: Supernumerary breast; Adenopathies; Polymastia
Introduction
The development of the supernumerary breast (polymastia or hypermetria) and its modality constitutes an interesting chapter in clinical observation. Polymastia is found in 90% of the chest, 5% in the abdomen and 5% in the armpit [1]. If the diagnosis is easy in the presence of a nipple and a milky discharge, it becomes more difficult in their absence. Thus, confusion with all etiologies of axillary masses is possible, which is the case in this observation. Polymastia remains a rare malformation whose axillary localization can be confused with other causes of axillary masses, in particular lipomas and lymphadenopathy. Its clinical and sonographic diagnosis can be difficult. The anatomopathological study confirms the diagnosis. This supernumerary breast tissue is likely to be the site of the same diseases as the physiological breast tissue, which requires surgical removal to prevent complications. Our case report allows us to put the light on this diagnosis and request the necessary examinations considering the diagnostic delay in front of this case.
Case Report
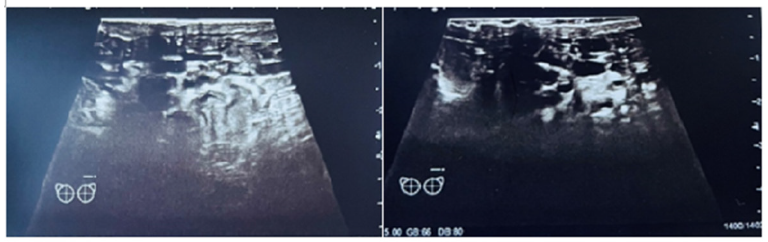
a young 26-year-old patient with no medical or surgical history, 2nd gesture and parity, breastfeeding for 1 month who consulted at the postnatal consultation for axillary pain accentuated at the level of axillary adenopathies evolving since puberty, for which the patient had consulted several times or 2 diagnoses were evoked lipomas and adenopathies of benign appearance. the axillary prolongment is bilaterally the site of a subcutaneous mass of 2cm*2cm with bumpy contours and a slightly painful mobile soft consistency without any discharge or skin irregularities (Figure 1). The gynecological examination and the rest of the clinical examination were without particularities. All evolving in a context of conservation of the general state. The ultrasound examination shows swollen and thickened bilateral axillary fatty tissue suggestive of supernumerary breasts with absence of axillary adenopathies (Figure 2). Laboratory tests including CA 15-3, were normal. A surgical exegesis was decided and the anatomopathological study confirmed the diagnosis by the presence of mature adipose tissue interspersed with breast tissue having lobular architecture. numerous ducts and acini were seen lined by ductular epithelial cells./p>
Figure 1:Bilateral axillary supernumerary breasts without areolas.
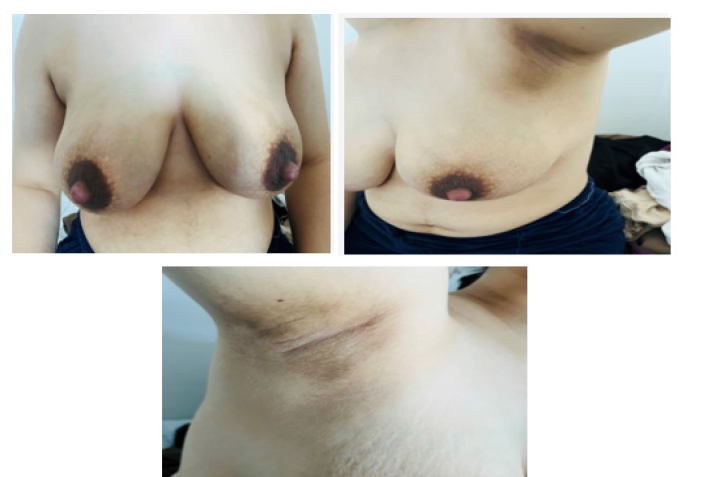
Figure 2:Ultrasound appearance of supernumeraries breasts.
Discussion
Any abnormality in the involution of the mammary Crete results in the persistence of glandular tissue anywhere along the lacteal line, from the axilla to the inguinal region, which can lead to the appearance of other buds whose persistence results in accessory or supernumerary breasts or polymastia [2]. Familial cases have been reported [3] and there is a hypothesis of autosomal dominant genetic transmission [4]. In our observation, no family antecedent had been found. Polymastia is present from birth but is rarely described in children same with our case, it is discovered during pregnancy or lactation due to hormonal impregnation that leads to an increase in its volume as well as the appearance of sensitivity even pain. This abnormality may pose diagnostic difficulties. Indeed, the absence of areola and the absence of engorgement during gestation and lactation explains why these tumors do not initially point to a supernumerary breast and can lead to a misdiagnosis of lipoma, axillary adenopathy, which was the case for our patient, or the diagnosis of benign axillary adenopathy for several years [4]. The bilateral and symmetrical nature of the axillary localization, the mobility and a transient increase in volume during pregnancy and lactation are the main clinical features that point to axillary accessory breasts.
Radiologically, the breast is composed ́ of conjunctivo-glandular tissue that appears hyperechogenic on ultrasound, and adipose tissue that is hypoechogenic (Figure 2). The predominance of adipose tissue in supernumerary breasts can often impose for a lipoma on ultrasound, in our case report, we did not have recourse to other examinations, only the ultrasound could raise the diagnosis. The predominance of adipose tissue in supernumerary breasts often suggests a lipoma on ultrasound, this also explains the absence of engorgement during gestation and lactation in our patient. The most important complication is malignant transformation even though the incidence of this cancerization is low [5]. This condition can reveal other malformations, especially of a urinary nature. Our patient has not been evaluated in this sense. As for therapeutic attitude; some authors recommend abstention in the absence of complications, others choose for a systematic exercise not only for the aesthetic and moral handicap that it entails, but also in order to prevent malignant degeneration [2,4]; for our patient we opted for a surgical procedure.
Conclusion
Polymastia remains a rare malformation, with aesthetic and moral prejudice whose axillary localization, which is rare, can lead to confusion with other causes of axillary masses, notably adenopathies and lipomas. Its diagnosis is suspected clinically and echo graphically, the anatomopathological examination allows to confirm the diagnosis. This condition may be the site of the same pathology as the physiological mammary gland, which requires surgical treatment to prevent complications.
References
- Velanovich V (1995) Ectopique Brest tissue, supernumerary breasts and supernumerary nippes. South Med J 88(9): 903-906.
- Abita T, Lachachi F, Durand Fontanier S, Maisonnette F, Valleix D, et al. (2004) Apropos of a case of bilateral axillary supernumerary breasts. Morphology 88(280): 39-40.
- Weinberg SK, Motulsky AG (1976) Aberrant axillary breast tissue: a report of family with six affected women in two generations. Clin Genet 10(6): 325-328.
- Anthony LT, Viera J (1999) Breast-feeding with ectopic axillary breast tissue. Mayo Clin Proc 74(10): 1021-1022.
- Giron GL, Friedman I, Feldman S (2004) Lobular carcinoma in ectopic axillary breast tissue. Am Surg 70(4): 312-315.
© 2023 Mariam M. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






