- Submissions

Full Text
Perceptions in Reproductive Medicine
Idiopathic Granulomatous Mastitis Associated with Behcet’s Disease: Case Report
Mariam M1*, Oumaima S1, Khaoula L1, Aziz S2, Najia Z1, Amina L1, Aicha K2 and Abdelaziz B1
1Department of Gynecology-Obstetrics and Endoscopy, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco
2Department of Gynecology-Obstetrics and Endocrinology, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco
*Corresponding author: Mariam M, Department of Gynecology-Obstetrics and Endoscopy, Maternity Souissi, University Hospital Center IBN SINA, University Mohammed V, Rabat, Morocco
Submission: January 13, 2023;Published: January 20, 2023

ISSN: 2640-9666Volume5 Issue3
Summary
Idiopathic Granulomatous Mastitis (IGM) is a chronic inflammatory disease of the breast. Recent studies have shown an increase in its prevalence. The etiopathogenesis is still unknown; however, inflammation as the result of a reaction to trauma, metabolic or hormonal processes, autoimmunity, and an infection with Corynebacterium kroppenstedtii have all been implicated. The most common signs of the disease are palpable mass, pain, inflammation and erythema, abscess formation, single or multiple fistulas, nipple retraction, breast deformity and axillary adenopathy, Ultrasound, mammography, and magnetic resonance imaging are not specific; however, ultrasound and mammography should be done to exclude other pathologies. The definite diagnosis is only through histological evaluation. there is no consensus regarding the best therapy for patients affected by IGM. Numerous therapeutic options are available, including observation, antibiotics, surgery, or drug therapy (steroids and immunosuppressants).
Keywords: Granulomatous; Idiopathic; Mastitis; Beast; Behcet’s disease; Diagnosis; Treatment
Introduction
Idiopathic Granulomatous Mastitis (IGM) is a chronic benign disease of the breast with unknown etiology, which is mostly seen in young women with a history of pregnancy shortly after their last pregnancy. Even though most studies have reported IGM to be a rare disease, recently many studies have been published, which show an increase in their prevalence [1]. It is of unknown aetiology and primarily affects young women. Potential precipitating factors include pregnancy, lactation, oral contraceptive use, and hyper prolactinaemia. There is no well-established aetiology. It is characterized histologically by chronic granulomatous inflammation in the breast lobules without caseous necrosis. It should be differentiated from other causes of granulomatous breast disease such as plasma cell mastitis, granulomatosis with polyangiitis, sarcoidosis, foreign body reaction, tuberculosis, and fungal infections [2]. The most common signs of the disease are palpable mass, pain, inflammation and erythema, abscess formation, single or multiple fistulas, nipple retraction and breast deformity and sometimes axillary adenopathy (Figure 1). Regarding the imaging methods, in most cases it is classified as a differential diagnosis for breast cancer and the definite diagnosis is only through histological evaluation [3]. Although some studies recommend surgical excision or incision and drainage, others recommend medical treatments such as antibiotics, corticosteroids, immunosuppressives, anti-inflammatory medications and sometimes only observation of the patient without any treatment. Nevertheless, the most appropriate treatment protocol is yet to be identified [4]. We report a rare case of idiopathic granulomatous mastitis associated with Behcet’s disease, occurring in 65-year-old women.
Figure 1:A 65-year-old women breast with a mass in the upper quadrants of the left breast in combination with ulcers and or multiple fistulas.

Case Report
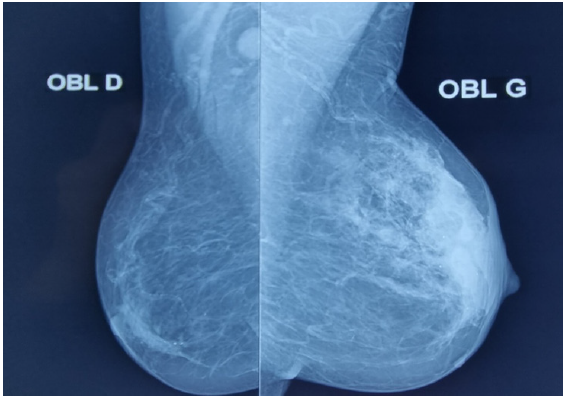
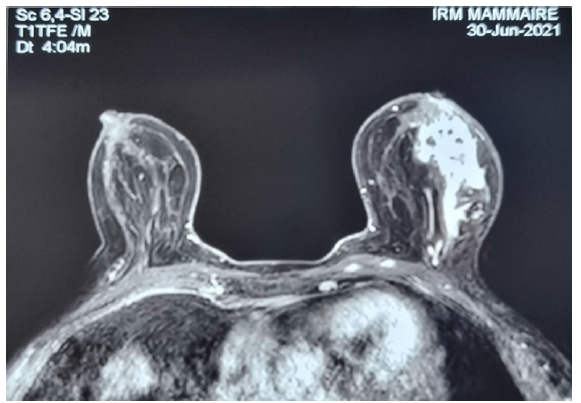
65-year-old patient, G2P2, followed Behcet’s disease for 15 years, with a history of painful lump, ulcers and or multiple fistulas in the left breast. There was no nipple discharge, she had not taken the contraceptive pill, or any other medication. On examination, the left breast contained a hard mass 40x30mm. There was no lymphadenopathy. Breast MRI demonstrates a mass centered by dilated ducts in the upper quadrant classified as BIRADS 5 (Figure 2). An ultrasound-guided breast biopsy was performed. The Histology showed formations with a localized infiltration of multi-nucleated giant cells, plasma cells, epithelioid histiocytes and lymphocytes with foci of micro abscess formation and nonnecrotizing granuloma. No organisms were seen on Gram, periodic acid-Schiff or Grocott stained sections. She had a normal hemoglobin and white cell count, a raised erythrocyte sedimentation rate (150mm/h). The biochemical profile was normal. Routine cultures were negative. The breast tissue for mycobacterium were negative. Tuberculin skin testing was negative. Our patient was treated medically with Corticosteroids (prednisone) and methotrexate. Thereafter, the lump gradually decreased to complete at 7 months.
Figure 2:Mammography of the left and right breasts demonstrates irregular mass in left breast.
Discussion
GM is a rare benign inflammatory breast disease which was first described in five case reports, by Kessler and Wolloch in 1972 [5]. IGM generally affects young women between 17 and 42 years of age [6]. However, IGM may be observed in advanced ages such as 65 or 83 years as well [7]. The pathophysiology of IGM is not clearly understood. However, the onset of some chemical reactions with oral contraceptive intake, infectious processes and autoimmunity are considered to be involved [8]. Although the possible etiological factors of IGM have not been certainly defined, some factors are believed to be effective, which include autoimmune diseases, undetected microorganisms, hyper prolactinaemia, diabetes and oral contraceptive use [9]. However, the exact factors have not been established yet. Symptoms in patients with IGM can include a palpable lump, localized or regional erythema, focal tenderness and peaud’orange [10,11]. Nipple involvement is infrequent, but can include discharge [12,2], scaling and retraction, with or without pain. Unilateral symptoms are most often reported; involvement of both breasts is less common [13,14]. The majority of patients are female, although cases have also been identified in males [10,15,16].
Histology is characterized by a non-caseating granulomatous inflammatory response of the breast lobules in the absence of specific underlying causes. Pathological evaluations demonstrate granulomas, multinucleated giant cells, lymphocytes, plasma cells and micro-abscesses [17]. Imaging demonstrates a varied appearance based on the timing of radiographic evaluation, extent of inflammation and possibility of prior intervention [12,18]. IGM is frequently aggressive and typically demonstrates features of infectious mastitis or inflammatory breast carcinoma (Figure 3). Diagnosis of IGM can be difficult and is frequently delayed. Malignancy and all other possible causes of mastitis must be excluded before a diagnosis of IGM can be considered [18]. there is no consensus regarding the best therapy. Numerous therapeutic options are available, including observation, antibiotics, surgery, or drug therapy (steroids and immunosuppressants). Nevertheless, the most appropriate treatment protocol is yet to be identified [4].
Figure 3:Breast magnetic resonance image: demonstrates an irregular mass cantered by dilated ducts in the upper outer quadrant classified as BIRADS 5.
Conclusion
IGM is a rapidly progressive rare inflammatory condition of the breast resulting in non-necrotizing granuloma formation. Clinical diagnosis is often one of exclusion, is delayed in the majority of cases, but should be facilitated by imaging. Contemporary breast imaging techniques are essential in documenting disease extent, providing guidance during percutaneous core needle biopsy and in helping to exclude malignancy. MR imaging can be useful in monitoring IGM behavior and clinical improvement, particularly in patients managed conservatively.
References
- Maione C, Palumbo VD, Maffongelli A, Damiano G, Buscemi S, et al. (2019) Diagnostic techniques and multidisciplinary approach in idiopathic granulomatous mastitis: A revision of the literature. Acta Biomed 90(1): 11-5.
- Larsen LJ, Peyvandi B, Klipfel N, Grant E, Iyengar G (2009) Granulomatous lobular mastitis: Imaging, diagnosis, and treatment. AJR Am J Roentgenol 193(2): 574-581.
- Thomas VM, Alexander SA, Bindal P, Vredenburgh J (2020) Idiopathic granulomatous mastitis-a mystery yet to be unraveled: A case series and review of literature. Cureus 12(2): e6895.
- Manogna P, Dev B, Joseph LD, Ramakrishnan R (2020) Idiopathic granulomatous mastitis-our experience. Egyptian Journal of Radiology and Nuclear Medicine 51(1): 15.
- Kessler E, Wolloch Y (1972) Granulomatous mastitis: A lesion clinically simulating carcinoma. AM J Clin Pathol 58(6): 642-646.
- Uysal E, Soran A, Sezgin E, Granulomatous Mastitis Study Group (2018) Factors related to recurrence of idiopathic granulomatous mastitis: What do we learn from a multicentre study? ANZ J Surg 88(6): 635-639.
- Lai EC, Chan WC, Ma TK, Tang AP, Poon CS, et al. (2005) The role of conservative treatment in idiopathic granulomatous mastitis. Breast J 11(6): 454-456.
- Bani-Hani KE, Yaghan RJ, Matalka II, Shatnawi NJ (2004) Idiopathic granulomatous mastitis: Time to avoid unnecessary mastectomies. Breast J 10(4): 318-322.
- Altintoprak F, Kivilcim T, Ozkan OV (2014) Aetiology of idiopathic granulomatous mastitis. World J Clin Cases 2(12): 852-858.
- Seo HRN, Na KY, Yim HE, Kim TH, Kang DK, et al. (2012) Differential diagnosis in idiopathic granulomatous mastitis and tuberculousmastitis. J Breast Cancer 15(1): 111-118.
- Patel RA, Strickland P, Sankara IR, Pinkston G, Many Jr, et al. (2010) Idiopathic granulomatous mastitis: Case reports and review of literature. J Gen Intern Med. 25(3): 270-273.
- Boufettal H, Essodegui F, Noun M, Hermas S, Samouh N (2012) Idiopathic granulomatous mastitis: A report of twenty cases. Diagn Interv Imaging 93(7-8): 586-596.
- Dursun M, Yilmaz S, Yahyayev A, Salmaslioglu A, Yavuz E, et al. (2012) Multimodality imaging features of idiopathic granulomatous mastitis: Outcome of 12 years of experience. Radiol Med 117(4): 529-538.
- Tse GMK, Poon CSP, Ramachandram K, Tony KF, Pang LM, et al. (2004) Granulomatous mastitis: A clinicopathological review of 26 cases. Pathology 36(3): 254-257.
- Reddy KM, Meyer CER, Nakdjevani A, Shrotria S (2005) Idiopathic granulomatous mastitis in the male breast. Breast J 11(1): 73.
- Andrade FEM, Heinzen RN, Pincerato KM, Oliveira FA, Docema MF, et al. (2017) Idiopathic granulomatous mastitis: Diagnosis and follow-up with magnetic resonance imaging. Mastology 27(3): 253-257.
- Gautier N, Lalonde L, Tran-Thanh D, Khoury ME, David J, et al. (2013) Chronic granulomatous mastitis: Imaging, pathology and management. Eur J Radiol 82(4): e165-e175.
- Fazzio RT, Shah SS, Sandhu NP, Glazebrook KN (2016) Idiopathic granulomatous mastitis imaging update and review. Insights into Imaging 7(4): 531-539.
© 2023 Mariam M. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






