- Submissions

Full Text
Perceptions in Reproductive Medicine
The Need for Redefining and Intensifying Pharmacovigilance in Reproductive Medicine
Kurt Kraetschmer*
Department of Reproductive Medicine, Austria
*Corresponding author: Kurt Kraetschmer, Department of Reproductive Medicine, Austria
Submission: April 13, 2022;Published: May 30, 2022

ISSN: 2640-9666Volume5 Issue2
Abstract
Background and aim: On the background of severe adverse events and even fatal sequelae of fertility treatments this research article aims at determining as to whether or not safety is sufficiently monitored in Medically Assisted Reproduction (MAR) and Artificial Reproductive Technology (ART).
Keywords:Safety; Adverse events; Bioethics; Health organizations; Fertility treatment
Method
The method implemented is a critical analysis which assesses pertinent documents issued by the most influential health authorities and agents of pharmacovigilance-namely World Health Organization (WHO), US Food and Drug Administration (FDA), Centers for Disease Control and Prevention (CDCP), and Australian Therapeutic Goods Administration (ATGA) with respect to accuracy, completeness, and reliability.
Result
The concepts pharmacovigilance, safety, and adverse event have not yet been defined in a cogent and comprehensive fashion. Clinical pursuits pertaining to safety in MAR and ART are not satisfactorily monitored by pharmacovigilance. Interventions by pharmacovigilance are frequently belated, inadequate, or insufficient to solve a safety problem. Numerous adverse events associated with medicines used in ART are still not adequately explored, especially those pertaining to drug interactions. In light of these deficits research on alternatives to artificial technologies are important for the clinical practice because an increasing number of women desire to avoid adverse events, risks, and complications. In this field of research exposure to conception plays a central role and finds support in endocrinological insights concerning the process of ovulation. In attempts to determine the crucial time of ovulation a new device may prove suitable for enhancing the chances of conception.
Conclusion and Implications
Given severe adverse events associated with artificial procedures in ART and MAR pharmacovigilance has to intensify its efforts to deal with new aspects of drug safety, including those engendered by a pandemic. In view of inadequate actions taken by proponents of pharmacovigilance in the past, the needs of women desiring “natural” forms of conception should be met. In accord with the principle of informed consent, all women should be informed about new avenues explored in various areas of research on ovulation, such as measurements of end-tidal pCO2. Besides safety, convenience and reliability should be part and parcel of future research projects dealing with the administration of medicines in ART and MAR.
Discussion
Pharmacovigilance as guarantor of safety according to definitions proposed by health authorities
According to commonly accepted definitions, the mission of Pharmacovigilance (PV) consists in ascertaining the safety of drugs available on the world market of therapeutic goods. Accordingly, PV has been defined as the “the science and activities relating to the detection, assessment, understanding and prevention of adverse effects or any other possible drug-related problem “[1]. Albeit widely accepted, this definition is not without blemish, especially regarding the identification of protagonists involved in the detection, assessment, and description of adverse events. In order to refer also to these protagonists, I propose the following definition: Pharmacovigilance represents the orchestrated efforts made by users and prescribers of drugs, healthcare providers, pharmacists, pharmacologists and researchers in order to identify, assess, and combat adverse events of drugs and foods and to propose measures suitable for alleviating/eliminating them. Among the leading authorities of PV is the World Health Organization (WHO), and this international institution has decidedly attempted to illuminate topical areas in reproductive medicine. One of the WHO’s primary targets is the standardization and harmonization of data collection, and for this purpose a set of definitions should be developed, which would be accepted by the international community: “The objective is to develop an internationally accepted and continually updated set of definitions, which would be utilized to standardize and harmonize international data collection, and to assist in monitoring the availability, efficacy, and safety of ART being practiced worldwide [2].
As can be seen from these agenda proposed by the WHO, the development of definitions should assist in monitoring not only the availability and efficacy but also the safety of ART worldwide. Whether this noble task can be accomplished is doubtful, however, because to date no clinically usable and ethically anchored definitions of safety can be found in the literature. Commonly safety is defined only vaguely with reference to death or a serious medical condition [3]. The crucial shortcoming of such a concept of safety is the absence of objective criteria that would allow to distinguish a serious medical condition from a condition which is not serious -- unless it would suffice to say that a serious condition is characterized by treatment in an intensive care unit. So far, however, this is not a generally accepted concept. In contrast to the stereotyped definitions commonly used primarily based on the risk-benefit ratio-I suggests a definition which takes into account the importance of the quality of life and the aspect of transience:
A drug is safe as long as it causes no more than a transient adverse event which entails a mild or moderate -but never severeimpact on the quality of life. In the popularizing medical literature an attempt has been made to define reproductive medicine in general terms. Unfortunately, authors have not succeeded in describing cogently and succinctly the multitude of intervention strategies characteristic of this discipline. Above all, the parameter safety is rarely an integral part of their definitions, as can be seen from the one proposed by a popular website: “Reproductive medicine is a branch of medicine concerning the male and female reproductive systems. It encompasses a variety of reproductive conditions, their prevention and assessment, as well as their subsequent treatment and prognosis. Reproductive medicine has allowed the development of artificial reproductive technique” [4]. Whether reproductive medicine has indeed allowed the development of “artificial reproductive technique” is doubtful because it is commonly assumed that the history of reproductive medicine properly speaking commenced with the technique of artificial insemination in 1884. “The first artificial insemination by donor (AID) procedure was performed in 1884.
A rich but infertile Philadelphia couple reasoned that there must be some way to ‘bypass’ infertility, and so they asked for the assistance of their friend, medical school professor Dr. William Pancoast” [5]. Regardless of the historical veracity, it is noteworthy that in our days artificial reproductive technology (ART) has been a focus also of leading health institutions such as the Centers for Disease Control and Prevention (CDCP). In a special website the CDC explains its aim of a “national ART surveillance” and underlines the importance of monitoring “the safety and effectiveness of ART procedures in the United States” [6].
Regrettably, the CDC does not explain what kind of measures have to be implemented for effectively monitoring safety and what type of safety problems should be addressed. Interestingly enough “safety” for the CDC seems to be restricted to the problem of multiple birth delivery: “While ART relieves the burden of infertility for many couples, it presents significant public health challenges due to the substantial risk for multiple birth delivery, which is associated with poor maternal and infant health outcomes. For this reason, it is important to monitor the safety and effectiveness of ART procedures in the United States” [6]. As can be seen, according to the CDC the reason for monitoring safety and effectiveness of ART procedures is the “risk of multiple birth delivery.” Clearly, an attempt to focus primarily on multiple birth delivery without paying heed to the plethora of safety problems in reproductive medicine is a serious ethical neglect. The disregard towards the parameter safety displayed by the CDC is typical for other publications on ART and MAR, be it research articles or popularizing medical literature. Given this negligence it is not surprising that serious adverse events and even fatal outcomes of ART go unnoticed not only by the press but also by the medical community. Thus in 2020 the problematicity of safety of ART has come to the forefront, when a fertility treatment for three women resulted in the death of one of them and in intensive care unit treatment for the two others. According to criminal investigations thus far, the cause for the fatal outcome was contaminated propofol [7]. Risks associated with the administration of propofol are no novelty. In an alert of 2007, the FDA reported severe adverse events in association with the administration of propofol and even solicited the cooperation of the CDC: “FDA is issuing this alert to inform healthcare professionals about several clusters of patients who have experienced chills, fever, and body aches shortly after receiving propofol for sedation or general anesthesia” [8]. According to the FDA, tests had been performed to find out whether or not contamination with bacteria or endotoxins had occurred. However, vials appeared to be uncontaminated: “. . . these tests have not identified any vials contaminated with bacteria or endotoxins” [8]. In contrast to the FDA’s finding, the treatment with a deadly outcome mentioned above was indeed associated with contaminated propofol. The fatal sequelae of this fertility treatment shed light on a problem that is frequently neglected in the clinical practice, namely the complexity of interventions. Fertility treatments are not a solo performance by one specialist but require the concerted efforts of several professionals, including anesthesiologists. In addition, the medicines administered must be carefully selected and assessed with respect to adverse events, risks, and complications for each individual patient, as proposed by precision medicine.
Adverse events of medicines used in fertility treatments
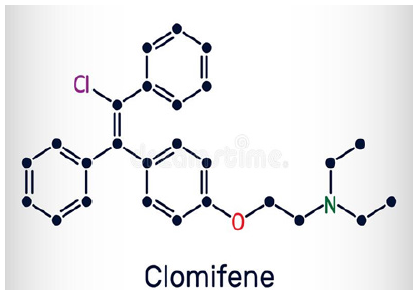
One of the most frequently used medicines in fertility treatments is clomifen citrat, an orally administered nonsteroidal stimulant of ovulation [9]. In pharmacology the following description of clomiphene is widely used: “Clomiphene Citrate Tablets, USP is an orally administered, nonsteroidal, ovulatory stimulant designated chemically as 2-[p-(2-chloro-1,2-diphenylvinyl) phenoxy] triethylamine citrate (1:1). It has the molecular formula of C26H28CINO•C6H8O7 and a molecular weight of 598.10” [10]. Its structural formula is shown in (Figure 1). It is worth noting that the FDA explicitly underlined the safety of the clomiphene citrate containing drug “clomid” when it referred to a Federal Register determination: “Federal Register determination that product was not discontinued or withdrawn for safety or effectiveness reasons” [11]. From an international perspective it is notable that in a publication of 2000 German authors considered Clomiphene as “well tolerated,” what apparently means that it is not causally related to any serious adverse events [12]. In contrast to this uncritical claim made by German researchers, the US Mayo Clinic presents a more thorough assessment and draws attention not only to allergies, breastfeeding, drug interactions, and other interactions (food, alcohol, and tobacco) but also to specific medical conditions which are considered hazardous. These conditions include the following: uncommon large ovary; cyst on an ovary; endometriosis; fibroid tumors of the uterus; inflammation of veins due to blood clots; history of liver disease; mental depression; and uncommon irregular vaginal bleeding [13]. Concerning the role of Clomiphene on the world market, it is worth noting that the Australian Therapeutic Goods Administration (ATGA) sent out an information about shortage of Clomiphene on Oct 8, 2018: “Consumers and health professionals are advised that the shortage of clomifene 50mg tablets (also known as clomiphene and marketed in Australia as Clomid) has been extended” [14].
Figure 1:Clomifene-structural formula.
To combat the shortage, an alternative drug from the Netherlands had been approved: “The TGA has granted a section 19A approval for the import and supply of an alternative product Clomid (clomifene citrate) 50 mg tablets marketed in the Netherlands” [14]. Earlier, on January 24, 2016, the TGA had allowed the import of an alternative drug manufactured in France. Strangely enough, adverse events associated with this French product apparently had not been sufficiently assessed so that the TGA had to encourage consumers to report any adverse events experienced: “Any adverse events involving the French product Clomid (clomifene citrate) 50mg tablets should be reported directly to Sanofi or to the TGA” [14].
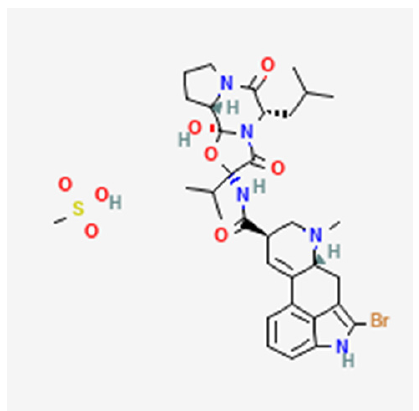
Besides Clomiphene as a stimulant of ovulation, reproductive medicine routinely uses a drug to combat the vexing problem of hyperlactinemia [15], namely bromocriptine. Bromocriptine mesylate is an ergot derivative with strong dopamine receptor agonist activity. The pharmacological description states: “Each Parlodel® (bromocriptine mesylate) SnapTabs® tablet for oral administration contains 2½mg and each capsule contains 5 mg bromocriptine (as the mesylate). Bromocriptine mesylate is chemically designated as Ergotaman-3′, 6′, 18-trione, 2-bromo-12′- hydroxy-2′- (1-methylethyl)-5′-(2-methylpropyl)-, (5′α)- monomethanesulfonate (salt)” [16]. The structural formula for bromocriptine is shown in Figure 2; [17].
Figure 2:Bromocriptine-structural formula.
The list of adverse events of bromocriptine is lengthy, and it includes bleeding from the stomach or bowel ulcers with potentially deadly outcomes [18]. Particular attention deserves the adverse events of post-marketing experience, namely psychiatric disorders (confusion, hallucination, libido increase, hypersexuality, etc,); nervous system disorders; eye disorders; ear and labyrinth disorders; cardiac disorders; vascular disorders; respiratory disorders; thoracic and mediastinal disorders; gastric disorders; skin and subcutaneous tissue disorders; musculoskeletal and connective tissue disorders [16]. Given the well-known plethora of adverse events of bromocriptine it is surprising that one of the foremost representatives of pharmacovigilance, ie, the European Medicines Agency (EMA), acted on bromocriptine only after concerns voiced by French authorities. “The review was triggered by concerns in France over increased reports of rare but potentially serious or fatal side effects, particularly cardiovascular side effects (such as heart attack and stroke), neurological side effects such as seizures (fits) and psychiatric side effects (such as hallucinations and manic episodes)” [19].
Concerning the salient question of drug interaction, it is mentionable that the Mayo Clinic provided more comprehensive information than the FDA, which is primarily responsible for such an issue. More precisely the FDA admitted that there exists no systematic evaluation of the risk of co-administering bromocriptine with other drugs. “The risk of using Bromocriptine in combination with other drugs has not been systematically evaluated, but alcohol may potentiate the side effects of Bromocriptine” [20]. In a more detailed explanation, the FDA draws attention to interactions with dopamine antagonist, butyrophenones, and other agents. Decreased efficacy of bromocriptine is caused by phenothiazines, metoclopramide, haloperidol, and pimozide. As bromocriptine is a substrate of CYP3A4, caution should be exercised in Coad ministering drugs which are potent inhibitors of CYP3A4, namely azole antimycotics and HIV protease inhibitors. “The concomitant use of macrolide antibiotics such as erythromycin was shown to increase the plasma levels of Bromocriptine (mean AUC and Cmax values increased 3.7-fold and 4.6-fold, respectively)” [20]. Concerning acromegalic patients increased plasma levels of bromocriptine were observed in concomitant treatment with bromocriptine and octreotide. Concomitant administration of bromocriptine and other ergot alkaloids is not recommended according to the FDA. “Dose adjustment may be necessary in those cases where high doses of Bromocriptine are being used (such as Parkinson’s disease indication)” [20]. In contrast to this short summary concerning interactions presented by the FDA, the Mayo Clinic provides a detailed list of drug interactions, and these are divided into three groups: those which are not recommended to be used together with bromocriptine (Eletriptan, Frovatriptan, Letermovir, etc.), those that are not recommended but may be used with caution (Abametapir, Almotriptan, Amoxapine, Boceprevir, Ceritinib, etc), and those which should be used only in exceptional cases and under rigorous medical surveillance (Abametapir, Almotriptan, Amoxapine, Boceprevir, Ceritinib, Clarithromycin, Clomipramine, etc.). An increased risk of certain adverse events may be caused by the use of the following drugs: Bromperidol, Cyclosporine, Kava, Thioridazine [21]. It is still an open question whether the taxonomy of drug interactions proposed by the Mayo Clinic will prevail in the clinical practice, but it certainly is a noteworthy attempt to ascertain safety through a better understanding of drug interactions. Besides bromocriptine for hyperprolactinemia, Human Menopausal Gonadotropin (HMG) is used for ovarian stimulation. It is considered by one website as a “leading treatment” which contains an equal balance of FS and LH administered “to stimulate the ovaries to produce multiple eggs during one cycle” [22]. Unfortunately, information on safety by this website is restricted to the laconic statement that the side effects of the three leading hMGs are in line with those of FSH medications: Three leading hMGs are Menopur®, Humegon® and Repronex®. Their side effects are in line with those of FSH medications, due to how similarly they function. hMG is derived similarly to FSH, from the urine of menopausal women [22].
In a clinical drug investigation of 2018, the profile of purified human menopausal gonadotropin for use in infertility had been presented. Unfortunately, in this profile the parameter safety is not addressed at all, and the focus is exclusively on efficacy: “Menopur® is a highly purified, urine-derived, human menopausal gonadotropin containing both Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH) activity” [23]. Menopur is considered as an appropriate option for Controlled Ovarian Stimulation (COS) for both, ART and Ovulation Induction (OI) in cases of anovulatory infertility. Concerning its endocrine profile, it is considered to be “associated with a different endocrine profile from that of recombinant (r) FSH in these settings (in terms of serum levels of FSH, androgens and/or estradiol) [23]. Research on hCG has been extensive for a number of years. More recently in 2020 a study compared highly purified human menotropin to recombinant follicle-stimulating hormone in high responders undergoing intracytoplasmic sperm injection. It remains unknown whether this comparative study investigated systematically the question of adverse events, risks and complications associated with the medicines used. At least in their conclusion the authors allude to safety by mentioning pregnancy as an adverse event.
They also note that number of adverse events was lower in the treatment with HP-hMG which seemed to have a better risk/benefit profile: “In high responders, HP-hMG provided comparable efficacy to rFSH with fewer adverse events, including pregnancy loss, suggesting its optimized risk/benefit profile in this population” [24]. Earlier, in 2019, authors published a clinical trial with the aim of comparing the efficacy of HP-hMG plus recombinant human follicle-stimulating hormone (rFSH) to rFSH alone “on Controlled Ovarian Stimulation (COS) in vitro fertilization-embryo transfer (IVF-ET)” [25]. On the basis of their findings the authors conclude that “the use of combined HP-HMG with FSH may be superior to rFSH alone in stimulating the ovary in normal responders undergoing IVF treatment” [25]. As can be expected, the authors admit that confirmation of their study through prospective studies with large samples are needed. Regrettably, the topic safety remains unmentioned in this study. As can be seen from an analysis of drugs used in reproductive medicine, pharmacovigilance has unearthed so far only fragmentary information on adverse events and safety hazards. Given the numerous lacunae regarding safety it is encouraging to see that some publications do indeed attempt to shed light on this topic.
Safety and adverse events addressed by research and health agencies
The problem of safety of contemporary infertility treatments has been addressed already in 2002 when a publication analyzed risks and challenges [26]. Interestingly enough, according to this study, the primary safety problem seems to be the incidence of multiple birth and the ensuing sequelae. A publication of 2016 in a pharmacological journal was devoted to drug safety, ie, the concept, the inception, and the importance in patients’ health. The results of this review are limited because emphasizing the role of health care professionals and advocating the idea of patient counseling to improve drug safety is no more than dwelling on the obvious, as can be seen from the following statement: “However, adverse drug reactions can be minimized if more precautions are taken by healthcare professionals, especially including the patient as one pillar of the therapeutic plan and providing more patient counseling, which will improve drug safety” [27].
From an international perspective a German a publication of 2013 is of interest for pharmacovigilance because it draws attention to guidelines for ascertaining the safety of medicines and offers a new definition for “adverse events” [28]. The new definition considers a side effect as a harmful and unintended (“schädliche und unbeabsichtigte”) reaction to a medicine. What is new in this definition is the inclusion of reactions due to overdosage, misuse, abuse or other medication errors. Clearly, the innovations announced by this publication are rather modest because the newly created possibility for patients and consumers to report adverse events to the agencies and institutions in charge have been a matter of course for some time in other countries. The most important innovation seems to be a patient information leaflet which is required and explicitly asks patients to report not only adverse events but even suspicions of adverse events to doctors, pharmacists, relatives in health professions or directly to the federal agency in charge [28]. It remains to be seen whether all members of health professions will respond to this request because many of them are accustomed to receiving remunerations for the services they provide. Unless pharmaceutical companies offer some incentives for reporting adverse events of their products, reporting will be doomed to failure, even if each patient information leaflet is accompanied by a request and an appropriate form for such feedbacks.
Given unsatisfactory definitions of safety and adverse events it is not surprising that health agencies have attempted to provide clarifications. Thus, the FDA has attempted to define the concept of adverse events by using the idea of an “undesirable experience” and a “patient outcome.” According to the FDA “an adverse event is any undesirable experience associated with the use of a medical product in a patient. The event is serious and should be reported to FDA when the patient outcome is death, life-threatening, hospitalization, disability or permanent damage, congenital anomaly/birth defect, required intervention to prevent permanent impairment or damage, other serious (important medical events)” [29]. Examples for the conditions enumerated by the FDA include allergic bronchospasm, the need of treatment in an emergency room, serious blood dyscrasias or seizures/convulsions, even if they do not result in hospitalization. Other examples of medical events would be the development of drug dependence or drug abuse [29]. As can be seen, the FDA defines an adverse event as an experience but fails to specify why and how this experience comes into existence in conformity with the principle of cause and effect. I suggest that a comprehensive definition should also address this aspect as well as the quality of life in the following fashion: An adverse event is a reaction to a drug used which impacts on the user’s biopsychosocial health status in such a fashion that his or her condition must be considered as a mild, moderate, or severe deterioration of the quality of life. The FDA’s definition of adverse events reveals another crux of pharmacovigilance, namely the discrepancy between theoretical concepts and their applications in practice. The FDA correctly considers hospitalization or treatment in an emergency room as “serious” adverse event. Precisely such events occurred in association with an intratubal device for permanent contraception which had been approved by the FDA in 2002. Despite thousands of complaints worldwide and timely removal of the hazardous implant from the Australian market, the FDA failed to take appropriate action [30].
On the contrary, the FDA insisted on the safety of the device, implemented no more than insufficient and ineffective measures, and finally left it to the manufacturer to withdraw the implant from the market -- without issuing any ordonnance. The manufacturer’s willingness to pay US$ 1,6 billion to settle claims indicates the magnitude of economic ramifications due to the incompetence of a chief proponent of pharmacovigilance [31]. The case of this intratubal implant for permanent contraception also shows that pharmacovigilance depends on the cooperation of pharmaceutical companies, and it happened more than once that companies violated their ethical obligations and simply refrain from reporting adverse events. “Bayer AG failed to report thousands of complaints of injuries allegedly caused by its Essure contraception device to the U.S. Food and Drug Administration, according to newly unsealed documents” [32]. Shortcomings are conspicuous not only in the operating mechanism of the FDA but also in those of other leaders of pharmacovigilance. Thus, the EMA has defined its role as pharmacovigilance with the same wording as the WHO and claims that it coordinates the pharmacovigilance system and supports it within the EU. However, attempts to provide a better understanding of “safety” or “adverse event” are still missing, as can be seen from the following statement: “The European Medicines Agency (EMA) coordinates the European Union (EU) pharmacovigilance system and operates services and processes to support pharmacovigilance in the EU” [33].
The Australian authorities on their part claim that they monitor “the safety of medicines to improve the understanding of their possible adverse effects” [34]. To accomplish this goal the TGA emphasizes the need for reporting all suspected adverse events, but apparently restrict this activity to health professionals: “It is important that health professionals report all suspected adverse events, including known adverse events (to monitor their frequency), for all drugs, no matter when they were registered” [34]. Particularly important for the ATG are those adverse events that occur rarely, are particularly dangerous, and occur after prolonged exposure, as well as drug interactions not observed in clinical trials: “It is particularly important for detecting rare and potentially dangerous adverse effects, those occurring after prolonged exposure, and drug-drug and drug-disease interactions that may not have been observed in clinical trials”[34]. The importance attached by the ATG to supplementing experiences of clinical trials is self-explanatory and is an ongoing issue in studies on post-marketing-experienced adverse events. It must be borne in mind also that lawyers closely watch the unearthing of new adverse events to argue on grounds of liability and negligence. “Plaintiffs in the Essure lawsuit claim that Bayer is guilty of negligence and also of failing to warn the public about the risks associated with Essure. Furthermore, the lawsuits claim that the manufacturer falsified documents in order to get market approval for Essure” [35].
As can be seen from the foregoing analysis of research articles and publications by health agencies, numerous attempts have been made to define adverse events and to explain how they jeopardize a patient’s health. Regrettably, effective strategies for achieving the goals of PV have not yet been implemented. Soliciting reports from health professionals or users will produce meager results because the activity of reporting involves time and energy, and remunerations for such endeavors are presently nonexistent. Intensified reporting of adverse events will occur only if pharmaceutical companies are willing to provide appropriate remunerations. After all, it is in their own interest if improved quality of their product leads to an increase of revenues. At present lawyers and law firms seem to be more successful in motivating victims of adverse events to report the harm they experienced through the use of certain medicines or devices. During a time plagued by Covid-19 the problem of safety in reproductive medicine is further aggravated. Most recently a review has been published which focused on COVID-19 and human reproduction.
The authors of this review hypothesize that the virus targets not only the respiratory system but also male and female organs of reproduction which express its main receptor ACE2: “Emerging evidence suggests that the virus also targets male and female reproductive organs that express its main receptor ACE2, although it is as yet unclear if this has any implications for human fertility” [35]. Also, in 2021 appeared a study on the potential impacts of COVID-19 on reproductive health based on scientific findings and encompassing the social dimension. Authors claim that their study illustrates two aspects: first the impact of the COVID-19 pandemic on the reproductive process and second the sociosexual dimension of the disease. They recommend precautions that should be taken “to avoid infection via sexual transmission or vertical transmission, which may alleviate the fear associated with continuing normal social relationships and economic activities” [36]. The question of how to define “normal” social relationships is not answered by the authors; neither is there an explanation of the economic activities affected by the pandemic.
In 2020, a comprehensive review of the impact of COVID-19 on human reproductive biology, assisted reproduction care, and pregnancy has been presented from a Canadian perspective. Given the availability of only a restricted amount of data on pregnant women the authors suggest that during pregnancy COVID-19 symptoms and severity are similar to those in non-pregnant women. Concerning effects of SARSA-CoV-2 on gametes they consider evidence as insufficient: “In summary, reported data on pregnant women is limited, suggesting that COVID-19 symptoms and severity of the disease during pregnancy are similar to those in non-pregnant women, with pregnancy outcomes closely related to severity of maternal disease. Evidence of SARS-CoV-2 effects on gametes is limited” [37]. Besides the research mentioned above, the NIH has reported on COVID-19 and underscored an issue related to reproductive medicine, namely “a small increase in menstrual cycle length” linked to COVID-19 vaccines [38]. What is conspicuous in this report and generally in the studies on COVID-19 proposed so far is a lack of systematic inquiry into the safety of vaccines administered for each individual patient according to precision medicine. Such an inquiry should explore the correlations between the vaccine administered and all the medicines used by the patient, including hormonal contraception. Precisely this question would be the primary responsibility of pharmacovigilance, and to answer it one crucial aspect has to be considered that often goes unmentioned in research publications, namely the economic dimension. Manufacturers of medicines used in reproductive medicine are guided by the golden principle of free market economies, namely profit maximizing. Political and economic developments on the world market during the last decades have shown that this principle supersedes all other principles also in the clinical practice, even long-established principles such as ledge artis (according to the law of the art) [39].
Benefits of natural approaches to enhance chances of conception
In view of unresolved problems and unanswered questions concerning the safety of drugs it is not surprising that an increasing number of women express the desire to pursue alternatives to ART, and some research publications provide an impetus for such desires. In these publications, the chances of exposure to conception is a pivotal topic. Thus, as early as 2002 it has been suggested that “sufficient exposure to the chances of conception” should be assured before any treatment is initiated [40]. One of the most noteworthy auxiliary instruments for exposure to the chances of conception is a device which allegedly indicates with highest precision the time of ovulation [41]. The new technology is the result of research on the effects of progesterone on respiration which go back to the last century where endocrinological research had elucidated the thermogenic effect of progesterone and its stimulatory effect on respiration: “Progesterone is thermogenic and is probably responsible for the rise in basal body temperature at the time of ovulation.
It stimulates respiration, and the alveolar partial pressure, PCO2 (PACO2), in women during the luteal phase of the menstrual cycle is lower than that in men. In pregnancy, the alveolar PACO2 falls as progesterone secretion rises” [42]. Clinical findings on progesterone and its effect on respiration were published in the year 2002, when authors presented a study on the expiratory CO2 measurement for determining accurately the fertile days of the menstrual cycle [43]. In outlining their study design the authors specify that the end tidal pCO2 (etpCO2) was determined at several occasions in 195 menstrual cycles of altogether 160 women. Luteinizing hormone (LH), estradiol, and progesterone were determined by immunoassay with the goal of detecting the preovulatory LH-surge. A biphasic pattern of the end tidal pCO2 was observed during each cycle. During luteal phase values were on the average 6.5mmHg lower than during follicular phase. End tidal pCO2 started to decrease one to eight days (median 4.5) prior to the preovulatory LH-surge and this reduction coincided with both, the appearance of a dominant follicle and the rise of estradiol in serum previous to ovulation. At the end of the luteal phase, the end tidal pCO2 increased within only 2 to 3 days. Of particular importance is the fact that, according to the authors, the end tidal pCO2 does not depend on circadian rhythms and is not influenced by physical activity. These finding justify their claim “it is a reliable and easy to use technique to predict the fertile phase in a menstrual cycle” [43]. In addition, findings regarding pCO2 give support to nonhormonal methods which rely for their efficacy on the LH surge: “In the perspective of natural family planning it is a promising, practical and nowadays easily affordable method to detect the LHsurge and predict ovulation” [43].The primary advantage of this new technology to determine the time of ovulation is not only its easy usability and high reliability but also its extraneousness to any adverse events or health hazards. Given the possibility to circumvent adverse events associated with medicines used in reproductive medicine, women should be informed about alternatives according to the principle of informed consent. This principle, emphasizing patient autonomy, states explicitly that each patient should be informed about procedures and medicine in such a fashion that she/he is enabled to make an “intelligent choice” [44].
Conclusion
On the basis of the findings of this research article it can be recommended that pharmacovigilance be defined in a cogent and comprehensive fashion so that each user of medicines understands that she or he is part and parcel of a worldwide monitoring system which is headed by such authorities as the WHO, the FDA, the EMA, and the AGTG. Consumers should be aware that these authorities do not always stand up to their expectations to protect the public health by monitoring the safety of drugs on the world market. Shortcomings in the actions taken by health authorities are at times causally related to lack of cooperation on the part of pharmaceutical companies which rigorously pursue their objective of profit maximizing. Concerning drugs used in ART intensified research on drug interactions is mandatory. In light of risks associated with ART, the interest of women in “natural” approaches to reproductive medicine should be honored. Research on these options should be intensified and research results should be disseminated by public and private health institutions.
References
- WHO (2022) Pharmacovigilance. Switzerland.
- WHO (2022) Reproductive health. Switzerland.
- Trussell J, Raymond EG, Cleland K (2014) Emergency contraception: A last chance to prevent unintended pregnancy. Contemporary Readings in Law and Social Justice 6(2): 7-38.
- Wikipedia (2022) Reproductive Medicine.
- Clowes B (2020) The early history of assisted reproduction. Human Life.
- CDC (2022) National art surveillance.
- Wammerl P (2020) Fertility clinic: Anesthetist admits fatal error.
- FDA (2022) Propofol.
- FDA (2022) Clomiphene Citrate.
- (2022) Clomiphene.
- FDA (2022) Federal Register Clomiphene Citrate.
- Schill T, Strik D, Germer U (2000) Sterility and infertilite t. In: Diedrich (Edt.), Gynaecology and obstetrics pp: 90-122.
- Mayo (2022) Clinic-Clomiphene.
- (2022) Therapeutic goods administration. Clomifene.
- Samperi I, Lithgow K, Karavitaki N (2019) Hyerlactinaemia. J Clin Med 8(12): 2203.
- (2022) Bromocriptin.
- NIH (2022) Bromocriptin-structural formula.
- (2022) Bromocriptin (Parlodel). Side effects.
- (2022) European medicines agency-Bromocription.
- (2022) Bromocriptin-FDA.
- (2022) Mayo clinic-bromocription. Mayo Clinic, USA.
- (2022) Human menopausal gonadotropins.
- Deeks ED (2018) Highly purified human menopausal gonadotropin (Menopur): A profile of its use in infertility. Clin Drug Investig 38(11): 1077-1084.
- Witz CA, Daftary GS, Doody KJ, Park JK, Seifu Y, et al. (2020) Randomized, assessor-blinded trial comparing highly purified human menotropin and recombinant follicle-stimulating hormone in high responders undergoing intracytoplasmic sperm injection. Fertil Steril 114(2): 321-330.
- Li Shu, Qianhua Xu, Meng Q, Xue D, Zhang Y, et al. (2019) Clinical outcomes following long GnRHa ovarian stimulation with highly purified human menopausal gonadotropin plus rFSH or rFSH in patients undergoing in vitro fertilization-embryo transfer: A multi-center randomized controlled trial. Ann Transl Med 7(7): 146.
- Mitchell AA (2002) Infertility treatment-more risks and challenges. N Engl J Med 346: 769-770.
- Alshammari TM (2016) Drug safety: The concept, inception and it importance in patients’ health. Saudi Pharm J 24(4): 405-412.
- Bräutigam K (2013) Medicines act: Too risks of side effects. Dtsch Arztbl 110(6): A-206/B-193/C-193.
- (2022) FDA-safety communications.
- (2020) Washington post.
- (2020) The wallstreet journal.
- (2020) Washington post.
- (2020) EMA-Pharmacovigilance.
- (2022) Australian therapeutic goods administration. Adverse Drug Events.
- Anifandis G, Tempest HG, Oliva R, Swanson GM, Simopoulou M, et al. (2021) COVID-19 and human reproduction: A pandemic that packs a serious punch. Syst Biol Reprod Med 67(1): 3-23.
- Hashem N, Abdelnour SA, Alhimaidi AR, Swelum AA (2021) Potential impacts of COVID-19 on reproductive health: Scientific findings and social dimension. Saudi J Biol Sci 28(3): 1702-1712.
- Madjunkov M, Dviri M, Librach C (2020) A comprehensive review of the impact of COVID-19 on human reproductive biology, assisted reproduction car and pregnancy: A Canadian perspective. J Ovarian Res 13 (1): 140.
- (2022) National Institutes of Health (NIH).
- Kraetschmer K (2013) Is the lege artis principle obsolete? J Forensic Res 4: 194.
- Johannes LHE (2002) Female subfertility. Lancet 360 (9327): 151-159.
- (2022) Breathilo.
- Ganong WF (1995) Review of medical physiology.
- Moeller KT, Hein A, Licht P, Schmidt A, Veitenhansel S, et al. (2006) Exspiratorische CO2-Messung in der Zyklusüberwachung-ein einfacher und zuverlässiger Marker zur Bestimmung der fertilen Tage. Journal für Fertilität und Reproduktion 13(1): 5-12.
- (1992) Code of Medical Ethis. Current Opinions, American Medical Association. Illinois, USA.
© 2022 Kurt Kraetschmer. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






