- Submissions

Full Text
Perceptions in Reproductive Medicine
Role of Smoking in Male Infertility
Subrat Panda*, Ananya Das, Anusuya Sharma and Vinayak Jante
Department of Obstetric Gynecology, India
*Corresponding author: Subrat Panda, Department of Obstetric Gynecology, India
Submission: October 04, 2021;Published: October 21, 2021

ISSN: 2640-9666Volume4 Issue5
Abstract
Objectives: Cigarette smoking is associated with subfertility in males and may lead to a decrease in sperm concentration, lower sperm motility, and a reduced percentage of morphologically normal sperms. The objective of the study is to find out the effect of smoking with semen parameters and the relationship between amount of cigarette smoking and semen parameters.
Method: This is a hospital-based cohort study conducted in the Infertility clinics of NEIGRIHMS from December 2019 for a period of 1year. 254 male partners were enrolled for the study. Routine semen analysis was carried out under light microscopy according to WHO guidelines.2010. Data was analysed to find out relation of smoking with semen parameters and the relationship between amount of cigarette smoking per day and semen parameters by using SPSS Software Version 21.
Result: In the one-year period we had 140 cases of non-smoker and 114 cases of smokers. On analysis of the findings of sperm count, smokers have relative risk of 2.45 of getting oligozoospermia (p value=0.0005). Smokers have relative risk of 1.5 of having total motility <50%. For progressive motility, smokers have relative risk of 2.01 of getting progressive motility<32%. No dose relationship with abnormal semen parameter.
Conclusion: Smoking affected sperm count, and total and progressive motility but there was no dose and effect relationship between number of cigarettes per day and its affect on semen parameter.
Keywords: Smoking; Non-smokers; Total motility; Progressive motility; Vitality; Morphology
Introduction
Male infertility plays a key role in conception difficulties of up to 40-50% infertile
couples [1]. Although in some men, a specific disorder may be present; however, no apparent
reason for infertility can be found. This has drawn attention to the impact of lifestyle and
environmental factors, especially diet, obesity, smoking, alcohol intake, recreational drug
use, and exposure to environmental toxins, on reproductive health of such men [2]. Many
studies have shown that cigarette smoking has a deleterious effect on both male and female
reproductive systems and fertility [3]. Nowadays, the population of cigarette smokers is
increasing despite the facts about its effects and hazards to human health and this number
is reaching one third of worldwide population in the 15 years and above age group. Cigarette
smoke contains a large number of substances which are recognized as carcinogens and
mutagens including radioactive polonium, cadmium, benzopyrene, dimethylbenzanthracene,
dimethyl nitrosamine, naphthalene and methnaphthalene. However, the toxicity of many
of these constituents in cigarette smoke has not been well assessed for their effect on the
function of human spermatozoa.
Although the effect of cigarette smoking on sperm function was noticed a long time ago,
the mechanism by which tobacco smoke affects sperms remains poorly understood [4]. Thus, the impact of cigarette smoking on male fertility and sperm
characteristics remains a highly controversial issue. Around 15
number of cigarette smoking may be associated with subfertility in
males and may lead to a decrease in sperm concentration, lower
sperm motility, and a reduced percentage of morphologically
normal sperms [5,6]. Many studies on the effect of smoking on
semen quality have been carried out worldwide [6,7]. Some of these
studies showed that cigarette smoking results in a reduction of
sperm concentration, motility and normal morphology [6]. Others
have shown that cigarette smoking has a detrimental effect on
sperm quality [8]. There were many other studies with inconsistent
and conflicting results.
Materials and Methods
This is a hospital-based cohort study conducted in the Infertility clinic of NEIGRIHMS from December 2019 for a period of 1year.
Inclusion criteria
All males having abnormal semen parameters specially, counts, motility, morphology and vitality.
Exclusion criteria
a. Males with abnormal genital examination (varicocele,
undescended testicles, hydrocele, small sized testes);
b. Males with azoospermia
c. Males with history of mumps.
d. Males with history of surgery for inguinal hernia,
orchidopexy, or any scrotal surgery.
e. Males with chronic medical illness (diabetes mellitus,
hypertension, thyroid disease, cancer patients, and tuberculosis;
and
f. Males who had quit smoking for a period of less than 6
months. Seminal fluid was collected via masturbation into
sterile wide mouth plastic container after 3-5 days of sexual
abstinence in a room near the laboratory.
Samples with partial spillage were rejected; one sample per
male was included in the study. Samples were allowed to liquefy
at 37 °C environment, followed by analysis at room temperature.
Routine semen analysis was carried out under light microscopy
according to WHO guidelines 2010. Semen analysis comprised of
ejaculate volume, pH, viscosity, and sperm concentration (million/
ml), which were determined using Makler Chamber. Sperm
motility was determined as percentage of motile spermatozoa, and
morphology as percentage of normally-shaped spermatozoa. The
volume of ejaculate was measured by aspirating the whole sample
into a graduated pipette, the total sperm count was measured by
multiplying the sperm concentration by the volume of ejaculate.
For sperm morphology, slides were smeared with a small volume
of semen, and allowed to dry at room air temperature, stained with
eosin, then read for normal or abnormal sperms according to WHO
criteria 2010. Data was analysed to find out relation of smoking
with semen parameters and the relationship between amount of
cigarette smoking and semen parameters by using SPSS Software
Version 21.
Result & Observations
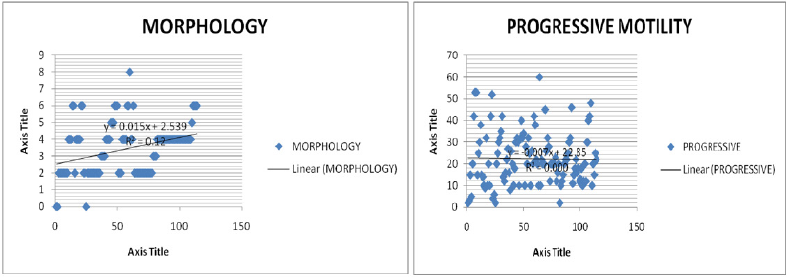
In the one-year period we had 140 cases of non-smokers and 114 cases of smokers. When the semen parameters in terms of sperm count was analyzed, smokers have relative risk of 2.45 getting oligozoospermia (p value=0.0005). In case of total motility< 50%, smokers have relative risk of 1.5 (p value 0.015). For progressive motility, smokers have relative risk of 2.01 of getting progressive motility<32% (p value<0.0001). But for vitality and morphology, we did not get any significant difference between smokers and non-smokers. In our study, the participants in smoking group were taking cigarettes varying from 5 to >20 cigarettes per day. We also analysed to see any correlation of number of cigarettes and relationship to the semen parameters by applying Pearsons Correlation test R2 (Count= 0.007, Total Motility=0.014, Progressive motility= 0, Morphology= 0.012, Vitality= 0.098) but we did not get any significant correlation between number of cigarettes and semen parameters as shown in the graphical representation (Table 1); (Figure 1 & 2).
Table 1: Effect of smoking on semen parameters.
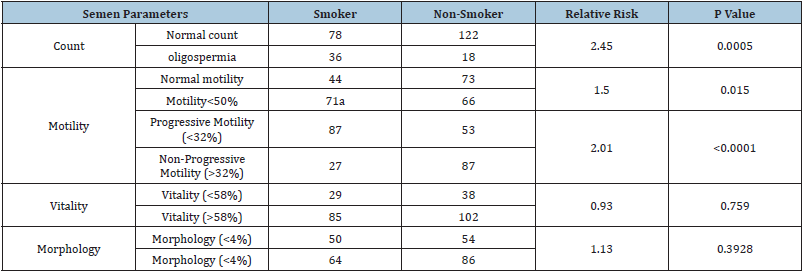
Figure 1: Correlation of sperm motility and vitality with smoking.

Figure 2: Correlation of sperm morphology and progressive motility with smoking.
Discussion
Despite worldwide anti-smoking campaigns, cigarette smoking
is very common. In India, the prevalence of smoking in males
in reproductive age group (15-69 years) is 24%. In our study,
we had 44.8% smoker males attending our infertility clinic. The
exact mechanism of action of nicotine on semen parameters is not
known. Smokers have lower seminal zinc levels than non-smokers,
with associated decrease in sperm concentration, motility, and
morphology. Interestingly, smokers with normal seminal zinc
concentrations did not experience the same degree of abnormal
semen parameters as those smokers with decreased seminal zinc,
suggesting that zinc concentrations could play a role [7].
In our study, smokers have a relative risk of 2.45 of having
oligozoospermia than the non-smokers. Smokers have a relative
risk of 2.01 of decreased progressive motility (<32%) than the
non-smokers. But we did not get any significant difference in
morphology and vitality. We also did not get any correlation
between the number of cigarettes/day and semen parameters. A
cross-sectional analysis of 2542 healthy men from 1987 to 2004
by Ramlau-Hansen [6] found that on semen analysis, cigarette
smokers had lower semen volumes, sperm counts, and percentage
of motile sperm compared to men who did not smoke. In another
large cohort of 1786 men undergoing infertility workup (655
smokers and 1131 non-smokers), Kunzle et al. [8] demonstrated
that smoking was associated with decrease in sperm density
(15.3%), total sperm counts (17.5%), and total motile sperm
(16.6%) compared with non-smokers. Zhang et al. [9] studied 362
Chinese men attending an infertility clinic and found that smokers
demonstrated decreased semen volumes, sperm concentrations,
and rates of forward progression compared with non-smokers.
Merino and colleagues, [10,11] who studied 358 Mexican
men stratified into 3 categories based on the number of cigarettes
smoked per day, also confirmed this type of dose dependency. The
authors confirmed the effects of smoking on reduced sperm density
and abnormal morphology, but also extended these findings to
note that men who smoked < 10 cigarettes per day experienced
significant changes in their semen analysis parameters. Therefore,
even “light” smokers appeared to be at risk for adverse effects on
fertility. Mahadeo Maroti et al in their study showed There was no significant difference between mild, moderate and heavy smoker.
Reecha Sharma et al. [2] found deterioration of semen quality is
more pronounced in moderate and heavy smokers. Künzle et al.
[8] prospectively studied 2,105 participants, of whom 839 persons
(39.9%) were smokers and 1,266 persons (60.1%) were nonsmokers
[12-14]. Sperm concentration, motility, and morphology
were significantly affected in smokers. Nevertheless, sperm vitality,
ejaculate volume, and progressive motility concentrations were
slightly but not significantly reduced among smokers. In our study,
we definitely found that smoking affected sperm count and motility
but no dose dependent relationship between smoking and semen
parameters could be elicited.
Conclusion
Smoking definitely affects male fertility adversely. Healthcare providers should facilitate individuals to quit smoking by educating, monitoring and constant support. The data on smoking and male fertility reinforce the preferred preventive approach of discouraging smoking and eliminating exposure to tobacco smoke among both males and females in general, and males in particular, while trying to conceive.
References
- Kumar N, Singh AK (2015) Trends of male factor infertility, an important cause of infertility: A review of literature. J Hum Reprod Sci 8(4): 191-196.
- Sharma R, Kelly RB, Jennifer M Fedor, Agarwal A (2013) Lifestyle factors and reproductive health: Taking control of your fertility. Reprod Biol Endocrinol 11: 66.
- Zenzes MT (2000) Smoking and reproduction: gene damage to human gametes and embryos. Hum Reprod Update 6(2): 122-131.
- Windham GC, Swan SH, Fenster L (1992) Parental cigarette smoking and the risk of spontaneous abortion. Am J Epidemiol 135(12): 1394-1403.
- Lewin A, Gonen O, Orvieto R, Schenker JG (1991) Effect of smoking on concentration, motility and zona-free hamster test on human sperm. Arch Androl 27(1): 51-54.
- Zinaman MJ, Brown CC, Selevan SG, Clegg ED (2000) Semen quality and human fertility: A prospective study with healthy couples. J Androl 21(1): 145-153.
- Liu RZ, Gao JC, Zhang HG, Wang RX, Zhang ZH, et al. (2010) Seminal plasma zinc level may be associated with the effect of cigarette smoking on sperm parameters. J Int Med Res 38(3): 923-928.
- Künzle R, Mueller MD, Hänggi W, Birkhäuser MH, Drescher H, et al. (2003) Semen quality of male smokers and non-smokers in infertile couples. Fertil Steril 79(2): 287-291.
- Zhang JP, Meng QY, Wang Q, Zhang LJ, Mao YL, et al. (2000) Effect of smoking on semen quality of infertile men in Shandong, China. Asian J Androl 2(2): 143-146.
- Olmedo BS, Chillik C, Kopelman S (2001) Definition and causes of infertility. Reprod Biomed Online 2(1): 41-53.
- Augood C, Duckitt K, Templeton AA (1998) Smoking and female infertility: A systematic review and meta-analysis. Hum Reprod 13(6): 1532-1539.
- Osser S, Liedholm P, Ranstam J (1984) Depressed semen quality: A study over two decades. Arch Androl 12(1): 113-116.
- Arabi M, Moshtaghi H (2005) Influence of cigarette smoking on spermatozoa via seminal plasma. Andrologia 37(4): 119-124.
- Chia SE, Lim ST, Tay SK, Swee TL (2005) Factors associated with male infertility: A case-control study of 218 infertile and 240 fertile men. Brit J Obstet Gynaecol 107: 55-61.
© 2021 Subrat Panda. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






