- Submissions

Full Text
Perceptions in Reproductive Medicine
Maternal Collapse- A Catastrophic Event: Mini Review
Kanika Chopra1* and Prasoon Gupta2
1Department of obstetrics and gynecology, Lady Hardinge medical college, New Delhi, India
2Department of Critical care and emergency medicine, Sir Ganga Ram Hospital, New Delhi, India
*Corresponding author: Kanika Chopra, Department of obstetrics and gynecology, Lady Hardinge medical college, New Delhi, India
Submission: January 18, 2021;Published: January 28, 2021

ISSN: 2640-9666Volume4 Issue3
Abstract
Maternal collapse is a rare event and is life threatening if not managed timely. The maternal and neonatal outcome depends on the cause of collapse, the gestational age at the time of incident and the management received. Most common causes of collapse are vaso-vagal syncope or epilepsy and most common cause of maternal death is hemorrhage. The normal physiological changes in pregnancy predispose the pregnant mother to risk of collapse and difficulty in resuscitation. Sub-standard care is the predisposing factor responsible for maternal collapse in majority cases. This review is planned with the aim of providing in brief the causes of maternal collapse and its initial management.
Keywords: Maternal collapse;Cardiopulmonary resuscitation;Intensive care;Perimortem cesarean
Introduction
Maternal collapse is defined as an acute event involving the cardiorespiratory and or brain, resulting in reduced or absent consciousness while pregnant or within 6 weeks after delivery [1]. It is a rare event, which in the absence of effective resuscitation techniques can be life threatening to both the mother and the fetus. The main aim in the management of this dreadful condition is appropriate diagnosis and timely management taking into consideration the alterations required in the resuscitation process as per the physiological and physical changes in pregnancy.
Causes of maternal collapse
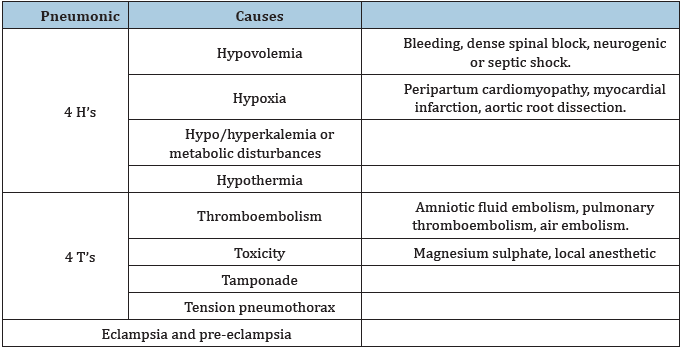
The causes are highlighted in Table 1. Most common causes of collapse are vasovagal syncope or epilepsy and most common cause of maternal death is hemorrhage [2].
Table 1:Causes of maternal collapse [2].
Physiological changes in pregnancy
Various physiological changes in pregnancy can have an impact on the effectiveness of
resuscitation are as follows.
a) Gravid uterus above 20 weeks leads to aortocaval compression causing supine
hypotension [3].
b) Increased CPR circulation demands due to increase in heart
rate and cardiac output and decrease in venous return.
c) Reduced oxygen carrying capacity due to increase in plasma
volume and dilutional anemia.
d) Increased risk of developing hypoxia due to increase in oxygen
consumption.
e) Decreased oxygen carrying capacity and more likelihood
of developing acidosis due to increase in respiratory rate,
decrease in residual capacity and arterial PCO2.
f) Difficult intubation due to laryngeal edema and large breasts
[4].
g) Increased risk of aspiration due to decreased gastric
motility and relaxed lower esophageal sphincter. Aspiration
pneumonitis that develops is known as Mendelsson’s
syndrome [5].
Risk factors that can predispose a pregnant or postpartum patient to the possibility of collapse are:
1. Maternal age more than 35 years.
2. Obesity.
3. Cardiovascular diseases.
4. Medical comorbidities like asthma, hematological disorders,
autoimmune disorders, musculoskeletal disorders, infections,
essential hypertension.
5. Cigarette smoking, substance abuse, alcoholism.
6. Lower socioeconomic status.
There has been development of maternity specific early warning charts, which helps in early detection of any deterioration. Modified early warning score charts (MEWS) incorporate the various vital parameters assessed are temperature, pulse rate, systolic blood pressure, respiratory rate, oxygen saturation, urine output and responsiveness to commands, which include AVPU i.e., alert, responsiveness to voice, responsiveness to pain stimuli or unresponsiveness or new CA i.e., confusion or agitation [6]. Actions of attending health care worker can be determined, depending on the score. Higher the score, earlier the need for intervention required by an expert. These charts may help identify the sick patients timely, but validation of such system does not exist.
Approach to a pregnant/postpartum patient presenting with collapse
Management of the patient presenting in a collapsed state
should follow Resuscitation council UK guidelines as a protocol [7].
a. Call for help.
b. Inform senior obstetrician, anesthetist and critical care or
cardiopulmonary resuscitation team. Inform neonatologist
team if viable gestation as per hospital protocol.
c. Ensure availability of crash trolley including availability of
anti-epileptic drugs.
d. Simultaneously, assess the patient and perform ABCDE.
e. A left lateral tilt of 15 degrees on a firm surface or else manual
displacement of gravid uterus when more than 20 weeks to
relieve aortocaval compression.
The technique used for manual uterine displacement is “up, off and over” method. It is performed by placing a hand below the uterus on the maternal right and pushing the uterus upwards and to the left [8]. Tilt of the patient may hamper the resuscitation, so later technique is preferable.
A. Airways-Ensure patency and clear the airways of any
obstruction i.e., vomitus, blood, foreign body, loose teeth.
B. Breathing-Check for spontaneous breathing by observing
chest movement. Ambu bag and mask can be used to support
breathing and oxygen is started at the rate of 15 liters/minute.
Insertion of supraglottic airways should be undertaken
till intubation can be achieved. Intubation with cuffed
endotracheal tube may be required in absence of breathing. In
absence of breathing, start CPR as per resuscitation council UK
guidelines. Cardiac compression is done at the rate of 100-120
beats per minute. 2 breaths via ambu bag or mask or ventilator
are given for every 30 compressions. Ideally, the person doing
the compression should be changed every 2 minutes to avoid
fatigue and effective resuscitation. After intubation has been
achieved, the ventilation is done at the rate of 10 breaths per
minute and chest compressions continued at the rate of 100-
120 per minute.
C. Circulation-Secure wide IV bore cannula and send blood for
baseline investigations (blood group, cross match, complete
blood count, coagulation profile, liver and kidney function
tests, blood glucose and arterial blood gas analysis) and start
fluid resuscitation as per the cause identified. One has to be
careful in cases of pre-eclampsia and eclampsia.
D. Defibrillation/Drugs- Heart rhythm is assessed during a brief
pause between compressions. If it is ventricular fibrillation
or pulseless ventricular tachycardia, defibrillation is started.
Adhesive pads are preferred over paddles. Any monitors
attached to the patient should be removed prior to shock
delivery. If it is asystole or pulseless electrical activity,
defibrillation is not recommended. Injection adrenaline 1mg
I/V need to be given every 3-5min in this case. Documentation-
I, would like to add documentation in the standard abbreviation
of resuscitation process. All the events and management should
be noted in patient’s file and informed to the attendants. This
has both significant clinical and medicolegal significance.
E. Exposure/Environment-Correction of hypothermia if there.
Etiology- I, would like to add an additional E in this standard
algorithm, in an effort to identify the possible cause of collapse.
It will help the resuscitating team to start the directed
treatment as per the cause.
In case of response to CPR, patient should be shifted to intensive
care unit.
If there is no response to CPR, peri-mortem cesarean section
should be performed within 5 minutes of the collapse at the same
place where resuscitation is being performed [8].
CPR is continued until a decision is taken by a senior obstetrician
and anesthetist in collaboration with cardiac arrest team.
Further treatment has to be channelized according to the cause
identified.
Conclusion
All personal involved in management of cases of maternal collapse should be aware of the need for the adaptations required in the CPR of pregnant patients. Regular interactive training involving multi-disciplinary facilities will help in efficient management of such cases.
References
- Chu J, Johnston TA, Geoghegan J (2020) Maternal collapse in pregnancy and the puerperium. BJOG 127: e14-e52.
- Whitty JE (2002) Maternal cardiac arrest in pregnancy. Clin Obstet Gynecol 45(2): 377-392.
- Chesnutt AN (2004) Physiology of normal pregnancy. Crit Care Clin 20: 609-615.
- Mushambi MC, Kinsella SM, Popat M, Swales H, Ramaswamy KK, et al. (2015) Obstetrics anesthetists association and difficult airway society guidelines for the management of difficult and failed tracheal intubation in obstetrics. Anesthesia 70(11): 1286-1306.
- Mendelsson CL (1946) The aspiration of stomach contents into the lung during obstetrics anesthesia. Am J Obstet Gynecol 52: 191-205.
- Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE (1981) APACHE-Acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 9(8): 591-597.
- Resuscitation Council (2019) Adult advanced life support. UK.
- Neumar RW, Shushter M, Callaway CW (2015) Cardiac arrest in special situations: American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 132(18 Suppl 2): S315-S367.
© 2021 Kanika Chopra. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






