- Submissions

Full Text
Perceptions in Reproductive Medicine
Antepartum Testing on a Zika Infected Fetus: A Case Report
Leon Maria DO and Faustin Daniel MD*
Wyckoff Heights Medical Center, USA
*Corresponding author:Faustin Daniel MD, Wyckoff Heights Medical Center, USA
Submission: June 22, 2019;Published: June 25, 2019

ISSN: 2640-9666Volume3 Issue3
Introduction
The Zika virus is a flavivirus first identified in monkeys in Uganda in 1947 and later found in humans in 1952. The most recent outbreak Zika infection occurred in 2015 in Brazil and has now spread throughout the Americas and even into some parts of the United States. Its primary mode of transmission to humans is via the Aedes mosquito family. Once infection occurs, Zika virus disease may occur, which may include symptoms such as fevers, rash, arthralgia and conjunctivitis. Perinatal transmission occurs either by vertical transmission or during delivery [1]. Zika virus infection in the antenatal period has been responsible for a variety of intracranial anomalies and microcephaly especially if the infection occurs during the first trimester. In the following case report, we present a pregnant woman with severe fetal intracranial anomalies and microcephaly but whose antenatal fetal monitoring parameters remained normal until her delivery by elective repeat c/section at 40 weeks of gestation.
Case Report
A 32-year-old gravida 2 P1001 was first seen at 32 weeks of gestation at the Antepartum unit of Wyckoff Heights Medical Center in Brooklyn for evaluation of a pregnancy complicated by a 7-week lag in fetal head size, noted on routine sonographic evaluation of fetal growth [2]. This patient has received prenatal care in her home country of Haiti until one day before the first prenatal visit at our institution. The patient reported having had a febrile illness during the first trimester of her pregnancy, but a clinical examination performed by her physician concluded this was a common viral illness but Zika testing was not available. At our facility, a detailed sonographic examination of the pregnancy showed the fetus to display microcephaly, with head circumference and biparietal diameter measurements below the 2.3 percentile for gestational age. Along with the microcephaly, dilatation of the lateral ventricles was also noted (Figure 1). The work up for genetic and infectious diseases confirmed normal 46 XY fetal karyotype and suggested possible Zika infection as the IgM for flavivirus was positive (The Zika RNA by PCR was negative).
Figure 1:Ultrasonographic image showing, fetal head circumference (HC) and biparietal diameter (BPD)as well as the dilated lateral ventricle.
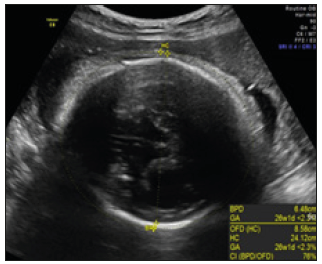
Figure 2:NST performed on 06/17/16.
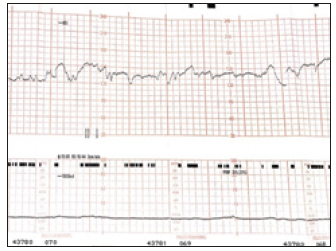
Figure 3:NST performed on 07/17/16.
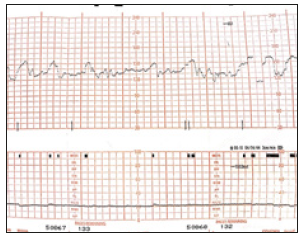
The patient was immune to rubella, toxoplasma gondii and cytomegalovirus. The patient was enrolled in our fetal surveillance program which included weekly fetal heart rate monitoring (Non- Stress Test, NST) as part of a biophysical profile and fetal biometric measurements every three weeks. The weekly non-Stress tests performed were all reactive. On Figure 1 & 2 we can appreciate two reactive tracings at two different dates. Moderate variability, with adequate baseline fetal heart rate and accelerations are seen in both fetal heart rate tracings. No decelerations were noted [3]. In this case we note that in spite of the Zika’s viral effect on the fetus, there was no evidence of central nervous system depression as evidenced by the fetal heart rate tracing and the Apgar scores at birth were 9 and 9 at 1 and 5 minutes. Serology testing on the newborn later confirmed Zika virus infection with a positive Zika IgM antibody.
Discussion
In the case presented, microcephaly and dilated lateral ventricles diagnosed by ultrasound imaging, and the positive maternal flavivirus serology led to the presumptive diagnosis of perinatal Zika. The viral infection which was confirmed by culture at birth. It is remarkable that the intracranial lesions in this case seem to spare the fetal central nervous system control over the cardiovascular system as we know it. Precisely the fetal cardiac activity is under the dual influence of the sympathetic and parasympathetic systems, causing a succession of relative tachycardia alternating with bradycardia tendencies, thus the baseline variability which we associate with adequate fetal oxygenation (Figure 2 & 3). Antepartum surveillance is widely used to identify fetal compromise especially those instances associated with acid base disturbances due to oxygen deprivation [4-6]. This often allows obstetricians to intervene before further compromise or even fetal death occurs.
The biophysical profile which evaluate five parameters related to the fetal wellbeing status namely the fetal body movements, tone, respiratory movements the amniotic fluid volume and the fetal cardiac activity assessed by the non-stress test (NST), often likened to an intrauterine equivalent of the Apgar’s score. In this patient, the weekly biophysical profile was reassuring, including a reactive NST (Figure 2 & 3) at every session until the day of delivery when the immediate neonatal evaluation yielded an Apgar score of 8 at 1 minute and 9 at 5 minutes [7]. The Zika virus is one of the most recently known infectious teratogens, responsible for multiple intracranial anomalies and loss of cerebral tissue, associated with fetal microcephaly. Our experience in monitoring the wellbeing of this fetus severely affected by the maternal Zika virus infection serves to show that at least in some fetuses so affected our monitoring tools can reliably predict the fetal status and guide our decision on the timing of delivery and avoid worsening of the neonatal prognosis for an already compromised intrauterine patient.
References
- (2019) Practice advisory. ACOG?
- (2014) Antepartum fetal surveillance. Practice bulletin 145. Obstet Gynecol 124: 182-192.
- Besnard M, Lastere S, Teissier S, Lormeau VM, Musso D (2014) Evidence of perinatal transmission of zika virus, French polynesia. Euro Surveill 19(13).
- Oliveira MS, Malinger G, Ximenes R, Szejnfeld PO, Alves SS, et al. (2016) Zika virus intrauterine infection causes fetal brain abnormality and microcephaly: tip of the Iceberd? Ultrasound Obstet Gynecol 47(1): 6-7.
- Sonja AR, Jamieson D, Honein M, Petersen L (2016) Zika virus and birth defects-reviewing the evidence for causality. N Engl J Med 374: 1981- 1987.
- Cauchemez S, Besnard M, Bompard P, Dub T, Artur GP, et al. (2016) Association between zika virus and microcephaly in French polynesia, 2013-15: A retrospective study. Lancet 387(10033): 2125-2132.
- Mlakae J, Korva M, Tul N, Popovic M, Prijatelj PM (2016) Zika virus associated with microcephaly. N Engl J Med 374(10): 951-958.
© 2018 Faustin Daniel MD. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






