- Submissions

Full Text
Perceptions in Reproductive Medicine
Reproductive Medicine: A Challenge to Implicate
Anugrah Ray and Debjani Nath*
Department of Zoology, India
*Corresponding author:Debjani Nath, Department of Zoology, University of Kalyani, West Bengal, India
Submission: February 13, 2019;Published: February 25, 2019

ISSN: 2640-9666Volume3 Issue2
Introduction
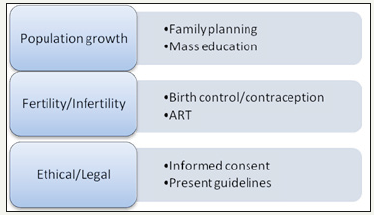
The world population is steeply increasing at the rate of around 1.07% per year. With this growth rate, the human population is going to touch 7.7 billion [1]. This figure has been emerging in the periphery growing infertility cases in both males and females as well. It is estimated that about 15% of couples have been suffering from the said problem [2]. The scenario is even more complex because males are solely responsible for 20-30% of these cases and the overall contribution towards infertility is 50%. It is also to be noted that the so-called percentage has been calculated using the hypothesis that females contribute 50% in overall cases of infertility. So, the reports on male infertility is based on the data collected by the cases on female infertility. The figure does not accurately represent entire regions of the world because we haven’t enough data on the rate of male infertility [2,3]. This note will encompass the ongoing problems associated with infertility/subfertility together with reproductive dysfunction and the lime light furnished by the reproductive medicine to tackle and overcome these problems. Reproductive Medicine basically deals with fertility preservation, diagnosing and treating the problems of infertility, and other reproductive issues. It also handles major discipline like family planning, puberty, menopause and sexual education. To overcome the challenges and find the solutions, it has got multidirectional scopes which are depicted in the (Figure 1).
Figure 1:The figure depicts the challenges and current practices to solve the issues.
Assessment Methods
The current practices involve the following assessment methods: Laboratory screening, medication, surgery, counseling, life style changes and mass education.
Present scenario
The technique of in vitro fertilization was reported in 1978 in the UK. Now, it has elapsed 40 years; ART (Assisted reproductive technology) has witnessed the birth of nearly 8 million babies worldwide [4]. This figure is a cumulative outcome of IVF (In vitro fertilization) and other fertility treatments and it is just an estimate by an international committee, ICMART (International Committee for Monitoring Assisted Reproductive Technologies). Contrary to developed countries, in developing countries, there are no strict guidelines and legal framework and the number of ART cases like IVF and ICSI (Intracytoplasmic sperm injection) has been increased rapidly. For example, the actual number of ART clinics running in different cities of India outnumbered the ART clinics which are enrolled under National Registry of ART Clinics and Banks in India, Indian Council of Medical Research. This situation is responsible for unnecessarily large number of ART procedures (particularly ICSI) practicing by the health care professionals on individuals/couples. Clinical data shows that ICSI resulted in a smaller number of live births compared to IVF when male infertility was not the problem. The ICSI was developed for the treatment of male infertility but it is approaching 100% in the Middle East and a few countries of the world. The world report covered for the years 2008, 2009 and 2010 highlighted that in 2010 there were 220,000 IVF treatments, but there were more than 455,000 ICSI treatments in the world. In Asian countries, ICSI practices were 1.4 times of IVF and the same is different in different regions of the world; starting from 2.7 times in North America, 6 times in Latin America and more than 60 times in Middle East [5,6].The national summary report 2016 compiled by Centers for Disease Control and Prevention, USA summarized the outcomes of all 463 fertility clinics stated that out of 263,577 ART cycles, only 75 % succeeded to transfer at least one embryo. These 75% (197,737) of total cycles ultimately resulted into 65,969 live births [7].
Etiology and challenges
Male infertility is the least understood problem of young males. The problems have been suspected at the genetic level which results into spermatogenic failure. Genetic problems forced us to move towards one side of the pole and the treatment options are available on the other side of the pole of the circle in which problems are entangled. Gene editing is the only option available to traverse and cross the barrier of etiology, but it is still far from reality even in coming years at least for human subjects. Scientists have been successfully rectified the culprit genes responsible for fertility issues in mice but when we consider the humans, the first challenge is not technical, but it is legal and of course ethical. The question of ethical issues has been with us when researchers put the ideas of embryo manipulation in the lab.
Overcoming the challenges
For the genetic issues, we must wait for a legal framework which will cover the guidelines for manipulating the human embryos at the genetic level. The day-to-day encountered problems have already been rectified by medicine. Most of the common problems fall under the category of hormonal imbalance and for that there is medicines available over-the-counter following doctor’s prescription.
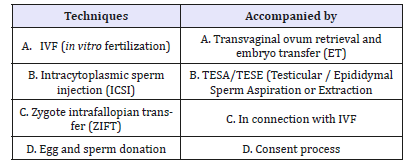
Abnormality in testosterone production is one reason in the etiology of male infertility [8]. The degree of infertility in male comprises the situation of azoospermia to oligozoospermia. Azoospermia is the extreme case in which there is complete absence of spermatozoa. The options available to treat azoospermia patients are not hopeful if someone wants to father a child. On the other hand, oligozoospermia can be treated by several methods which include life style changes, nourishments, hormonal balance and education. The treatment is already revolutionized by the ART processes; particularly the use of ICSI increases the chance of infertile males to father children [9]. On the other hand, infertility problem in females results in problems with ovulation, damage to fallopian tubes or uterus, problem in cervix etc. [10]. Aging is also a contributing factor in female infertility. But the good news is that ART is equally applicable in female candidates in the form of IVF, ICSI and ET (Embryo Transfer). The major practices under the ART comprise with the following methods/techniques as mentioned in (Table 1).
Apart from that, pre-implantation genetic diagnosis is also conducted on embryos prior to implantation.
Finally, even if we succeeded to discover new technique; the challenge of ethical/legal concern has raised. Despite of informed consent from the individuals/couples, there is no direct law which includes the human subjects for manipulation at genetic level to cure infertility/subfertility/sterility with the help of reproductive medicine (Table 1). The ethical issues are off course the major obstacles in implementing the whole techniques for the benefit of human civilization. We are already facing the process of posthumous reproduction. This technique has been available since 1950s, but experts have been facing regional and religious issues. There is no doubt that posthumous reproduction is an excellent idea which allows an option for fathering children in the event of sudden injury or death as these events are very common for astronauts and soldiers [11-13].
Table 1:Table shows current practices and techniques accompanied ART.
Acknowledgement
The authors acknowledge the Vivekananda fellowship scheme of the Government of West Bengal and PURSE programmer of Department of Science and Technology, Govt of India for the support.
References
- National Research Council (2000) Beyond six billion: forecasting the world’s population. The National Academies Press, Washington, DC, USA.
- Isidori A, Maurizio L, Romanelli F (2005) Treatment of male infertility. Contraception 72: 314-318.
- Agarwal A, Mulgund A, Hamada A, Chyatte MR (2015) A unique view on male infertility around the globe. Reprod Biol Endocrinol 13: 37.
- Sadeghi MR (2018) The 40th anniversary of IVF: has art’s success reached its peak? J Reprod Infertil 19(2): 67-68.
- Sullivan EA, Hochschild ZF, Mansour R, Ishihara O, et al. (2013) International committee for monitoring assisted reproductive technologies (ICMART) world report: assisted reproductive technology 2004. Hum Reprod 28(5): 1375-1390.
- Dyer S, Chambers GM, de Mouzon J, Nygren KG, et al. (2016) International committee for monitoring assisted reproductive technologies - world report on assisted reproductive technologies: 2008-2009-2010. Hum Reprod 31(7): 1588-609.
- Centers for Disease Control and Prevention: 2016 Assisted reproductive technology national summary report.
- Sokol RZ (2009) Endocrinology of male infertility: evaluation and treatment. Semin Reprod Med 27(2): 149-158.
- Practice committee of the society for assisted reproductive technology (2006). Genetic considerations related to intracytoplasmic sperm injection (ICSI). Fertile Steril 86(5 suppl 1): S103-S104.
- Tao X, Ge SQ, Chen L, Cai LS, et al. (2018) Relationships between female infertility and female genital infections and pelvic inflammatory disease: a population-based nested controlled study. Clinics (Sao Paulo) 73: e364
- Gilbert S (1993) Fatherhood from the grave: An analysis of postmortem insemination. Hofstra Law Rev 22(2): 521-565.
- Shefi S, Raviv G, Eisenberg ML, Weissenberg R, et al. (2006) Posthumous sperm retrieval: analysis of time interval to harvest sperm. Hum Reprod 21(11): 2890-2893.
- Tremellen K, Savulescu J (2015) A discussion supporting presumed consent for posthumous sperm procurement and conception. Reprod Biomed Online 30(1): 6-13.
© 2019 Debjani Nath. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






