- Submissions

Full Text
Perceptions in Reproductive Medicine
Birth Control and Contraception: The Dilemma of Informed Consent
Kurt Kraetschmer*
Austria
*Corresponding author:Kurt Kraetschmer, MD, PhD, Hermanngasse 4, A-2700 WrNeustadt, Austria
Submission: October 30, 2017;Published: August 20, 2018

ISSN: 2640-9666Volume2 Issue5
Abstract
The paper analyses the most pertinent publications on contraceptive efficacy from the viewpoint of the principle of informed consent. It proves by way of an international comparison that some of the most prominent publications on this topic fall short of providing complete and comprehensive information. It concludes that U.S. women are not in a position to exercise their right of self decision due to a lack of information and disregard for the principle of nil nocere on the part of authors and publishers. The implications are heightened attention to the need of intensified counseling in the clinical practice.
Keywords: Contraception; Bioethics; Family planning; Reproductive medicine
Introduction
Despite a prognosticated falling world population growth rate, reproductive health care continues to be an issue of international urgency. U.S. researchers have added an additional aspect to sexual and reproductive health with the finding that “every $1 spent on public funding for family planning saves taxpayers $3.74 in pregnancy-related costs [1]. “Given that about sixty-two percent of women of reproductive age are currently using contraception [2], it can be estimated that this percentage would be considerably higher if women were informed more accurately about contraceptive methods. The following discussion aims at rectifying inaccurate data that are widely disseminated and at clarifying misunderstood notions of natural non-hormonal contraception.
Discussion
Whenever women inquire about the possibilites of contraception and birth control, they turn to the most influential authorities in this field to seek complete and comprehensible infomation. In doing so, they follow the stipulation of the Code of Ethics of the American Medical Association which states: “The patient‘s right of self-decision can be effectively exercised only if the patient possesses enough information to enable an intelligent choice [3].“ Given such ethical requirement it is imperative that all those who act as provider of information on contraceptive options present the whole range of contraceptive possibilities to the consumer. Unfortunately, not all providers of information comply with this request. Among them, the Food and Drug Administration (FDA) is the most prominent, as it presented as early as 2013 a survey of FDA approved methods of birth control which, alas, is incomplete [4]. Although the FDA cites as its source the widelyknown authors of contraceptive technology [5], it does not render the entire findings of these authors in two important aspects. First, it does not indicate with the same precision the percentages of women who will not get pregnant; second, it leaves aside some of the contraceptive methods, which in contraceptive technology research appear as highly effective in case of perfect use.
According to contraceptive technology, the symptothermal method with a failure rate of 0.4 for perfect use appears as the most reliable of the fertility awareness-based methods, ie, those with no side effects or risks, and comes close to the 0.3 failure rate of combined pill and progestin-only pill. Other methods among those that have no side-effects and risks are Ovulation (3.0), TwoDay (4.0), and Standard Days (5.0); their efficacy is comparable to coitus interruptus (4.0) or diaphragm (6.0).
These data presented by sound scholarly research in contraceptive technology is frequently ignored by research and public health media. In many instances only one common failure rate for typical use is indicated whereas failure rates for perfect use are omitted. Thus, the U.S. Department of Health and Human Services [6] provides information on family planning and assigns collectively 24% (“number out of every 100 women who experienced an unintended pregnancy within the first year of typical use“) to the so-called “fertility awareness-based methods.“ These are considered as the least effective, just slightly superior to the “spermicide method“ (28%), and no mention is made of the findings in research on contraceptive failure, where perfect use estimates for the most reliable of the fertility awareness-based methods are considered to be “0.4 per 100 woman-years for the symptothermal method [7],“ 3.2 for the Ovulation method, 3.5 for the Two Day method and 4.8 for the Standard Days method.
The lack of accuracy and completeness found in public health media stands in contrast to European publications where each method is assigned its proper failure rate. Instead of collectively attributing failure rates to a group of methods, European scholars over the years have made efforts to assess each method individually [8]. As a result of these efforts the symptothermal method with a Pearl Index of 0.8 has emerged as the most reliable of the “natural family planning methods,“ followed by the basal temperature method (Pearl Index 1-3), cervical mucus (Pearl Index 15-32), and calendar after Knaus-Ogino (Pearl Index 15-40) [9]. The clear distinction among the various methods made by European research is rather an exception in U.S. publications where inaccurate failure rates are still being disseminated through various public health media and research publications.
As recently as 2015, the American Congress of Obstetricians and Gynecologists stated that natural family planning “is not as effective as other methods of birth control [10].“ As can be seen from an international comparison it is misleading to speak collectively of natural family planning without distinguishing among the various methods; and it is incorrect to state that they are not as effective as other methods, because the efficacy of the symptothermal method in case of perfect use (0.4) is almost equal to oral contraceptives, ie, combined pill and progestin-only pill (0.3) [5]. Not surprisingly, the ACOG has denied its own 2015 statement in a more recent statement in which the fertility awareness methods are lauded for their advantages regarding cost and safety [11].
On the other hand, no rectification of an inaccurate ranking of fertility awareness-based methods has as yet been initiated by an institution as influential as the Centers for Disease Control (CDC), which still presents a ranking where the fertility awareness-based methods are not individually assessed but treated as a group belonging to the least effective methods [12].
Unexpectedly, even scholarly publications fail to honor the principle of informed consent. The widely-known National Health Statistics Report [2] speaks in an unspecific manner of “fertility awareness“ and assesses the probability of pregnancy for typical use of all methods belonging to fertility awareness with one single rate of 25.3, and no figures are cited for perfect use of each one of these methods. Idiosyncratic failure rates are to be found also in wellknown reference-books such as the MSD Manual [13]. Although this scholarly work explains correctly that the symptothermal method is the most precise in determining the days where abstinence is mandatory, it assigns a failure rate of 10%, which obviously does not reflect the efficacy in case of perfect use established by international research as 0.3% [14].
As the above discussion shows, numerous highly influential agencies provide information on contraception, birth control, and family planing, but this information is either incomplete, inaccurate or outdated. The ensuing disadvantage for the consumer who expects to find information according to the principle of informed consent is ignorance of some of the safest (ie, no adverse events or interactions with other medications) natural methods and their noteworthy perfect use estimates.
Research publications and public health media should refrain, in the future, from disseminating information in a way that is incompatible with the principles of informed consent, nil nocere, and patient autonomy. These principles require that there be complete and comprehensive information for the patient, that priority be given to the least harmful method, and that each woman exercise her right of self-decision after having received information on all the available methods including side effects and risks.
Implications
If it is true that taxpayer money can be saved through family planning, it can be concluded that researchers and public health publishers should sense an ethical obligation in accordance with the principle of informed consent to strive for accuracy and completeness in information on contraceptive methods. In the clinical practice, the apparent burden of additional time commitment for counseling will be outweighed by the gains owing to the absence of any adverse events and interactions with other medications. Thus, it should be a primordial goal of reproductive health care that each woman be enabled to exercise her autonomy after having been informed comprehensively about all methods of contraception including their potential harm, so that a decision can be made also with respect to the least harmful methods, as stipulated by the bioethical principle of nil nocere (Table 1).
Table 1:Food and drug administration (FDA) approved methods of birth control.
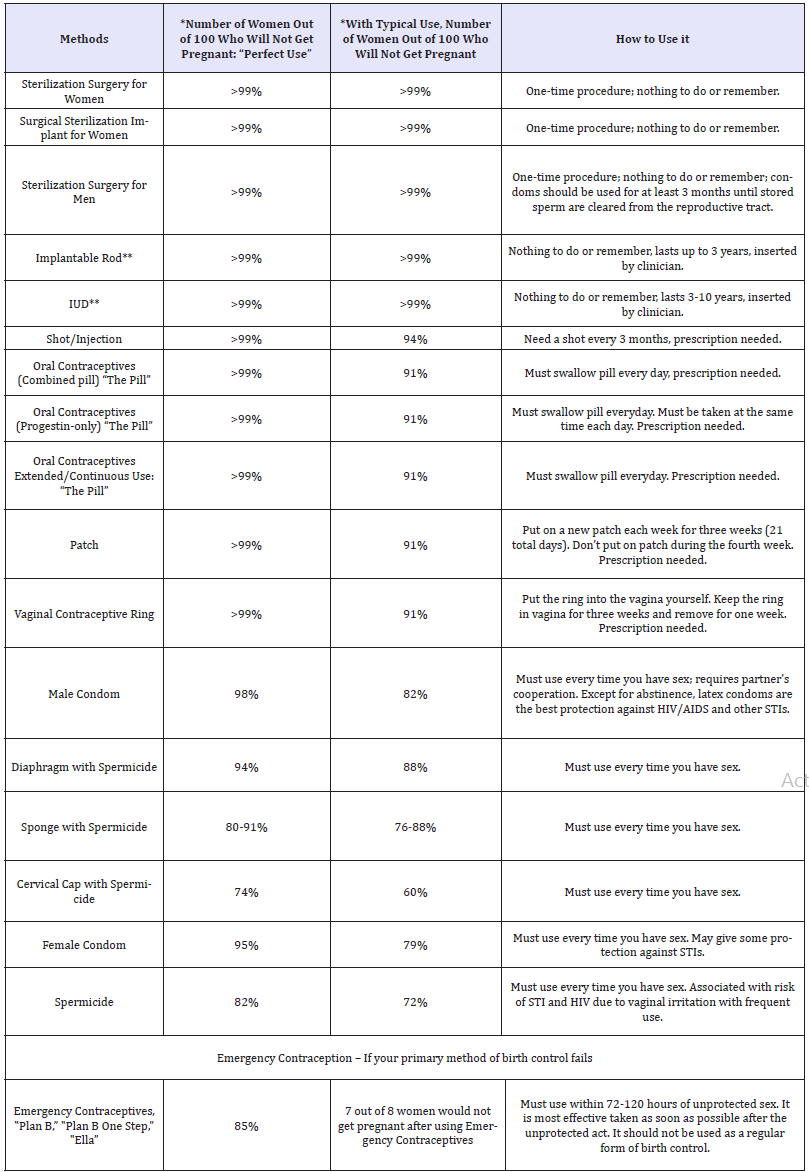
*Effectiveness rates are listed for ‟perfect use” and ‟typical use.”
**Implantable rod and IUD considered Long-Acting Reversible Contraceptives (LARC) and are highly recommended for young women who do not wish to become pregnant, but may want to have children later. Source: Contraceptive Technology 20th, 2011.
References
- Cleland K, Peipert J, Westhoff C, Spear S, Trussell J (2011) Family planning as a cost-saving preventive health service. NEJM 364(18): e37.
- Jones J, Mosher W, Daniels K (2012) Current contraceptive use in the United States, 2006-2010, and changes in patterns of use since 1995. Natl Health Stat Report 60: 1-25.
- Code of Medica Ethics (1992) Current opinions. American Medical Association, Illinois, Chicago, USA.
- (2016) US Food and Drug Administration.
- Trussell J (2011) Contraceptive efficacy. In: Hatcher RA, Trussell J, Nelson AL, Cates W, Kowal D, et al. (Eds.), Contraceptive Technology, (12th edn), Ardent Media,. CT Failure, New York, USA.
- (2016) US Department of Health.
- Trussell J (2011) Contraceptive failure in the United States. Contraception 83(5): 397-404.
- Herrmann FP, Heil J, Gnoth C, Toledo E, Baur S, et al. (2007) The effectiveness of a fertility awareness-based method to avoid pregnancy in relation to a couple‘s sexual behaviour during the fertile time: a prospective longitudinal study. Human Reproduction 22(5): 1310-1319.
- Gröger S, Grüne B (2000) Kontrazeption. In: Diedrich K (Ed.), Gynäkologie und Geburtshilfe. Springer, Berlin, Germany, pp. 60-87.
- (2016) Birth control (Contraception): Resource overview. American Congress of Obstetricians and Gynecologists, USA.
- (2017) Fertility Awareness-Based Methods of Family Planning. American Congress of Obstetricians and Gynecologists (ACOG), USA.
- Centers for Disease Control and Prevention (CDC) (2016) US medical eligibility criteria for contraceptive use.
- Beers MH, Berkow R (1999) MSD Manual. (17th edn), Merck & Co Inc. Whitehouse Station, USA.
- Freundl G, Sivin I, Batár I (2010) State-of-the-art of non-hormonal methods of contraception: IV. Natural family planning. Eur J Contracept Reprod Health Care 15(2): 113-123.
© 2018Kurt Kraetschmer. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






