- Submissions

Full Text
Perceptions in Reproductive Medicine
An Assessment of the use of Insecticide Treated Net among under Five in Ekiti State as a Means of Prevention of Malaria
Owoseni Joseph Sina*
Department of Sociology, Ekiti State University, Nigeria
*Corresponding author:Owoseni Joseph Sina, Department of Sociology, Ekiti State University, Ado-Ekiti, Nigeria
Submission: June 02, 2018;Published: August 17, 2018

ISSN: 2640-9666Volume2 Issue4
Abstract
Insecticide- treated nets are the most powerful malaria control tool if used correctly. Yet up to date, utilization is still unacceptably low: only 3 percent of African children are currently sleeping under an ITN, and about 20 percent are sleeping under any kind of net. Worse still, malaria continues to be the leading cause of child mortality and morbidity. The aim of this study was to investigate the intra-household factors that affect the utilization of ITNs in households with children under five. The study specifically sought to identify the intra-household practices that affect the use of ITNs among the under five; examined the knowledge, attitudes, perceptions and beliefs of caregivers towards the usage of ITNs; and lastly analysed the affordability of ITNs by households with children under five years. This study was conducted in Emure Ekiti, which were randomly selected and used a cross sectional design. The study findings show that first; there were intra-household factors that affected utilization of ITNs in households with children under five. These factors that affected utilization include; type of household structure, number of people sleeping in the household, intra-household gender relations, sleeping arrangements, disruption of sleeping patterns due to visitors and cultural rituals and functions. These factors affect consistency in utilization of ITNs and proper deployment. Secondly, knowledge on ITNs was found to be low though general knowledge about mosquito nets was found to be high. Utilization was also affected by poor perceptions, beliefs and attitudes that discourage caregivers from using the ITNs. Thirdly, access to ITNs was very inadequate and unavailable within the study community. The majority of the people being peasants, there were insufficient incomes and therefore ITNs were not a priority given the level of poverty. This study concluded that financial inadequacies at the household level, poor perceptions of caregivers and intra-household dynamics impact negatively on effective utilization of ITNs among the under fives. I would therefore recommend that; public-private partnership be adapted to ensure availability of ITNs and insecticides in local shops and other outlets including arrangements at village level to re-treat the nets, the economic level of caregivers should be boosted to counteract the financial inadequacies, adoption of a behaviour change strategy to transform caregivers ‟ perceptions, beliefs and attitudes; and massive education of the community.
Keywords: Prevention; Assessment; Malaria; Insecticide; Under-five; Emure-ekiti
Introduction
Insecticide Treated Bed Nets (ITNs/LLIN) were introduced in Nigerian as an effective means of preventing mosquito bites and malaria transmission following the meeting of African Heads of States in Abuja, Nigeria in the year 2000 [1]. Pregnancy women and children aged 0 to 5 years were the main target populations being the people most affected by the malaria scourge [1-3]. Following this giant stride in preventive medicine, studies have shown that ITNs/LLIN use in pregnancy reduced the incidence of malaria in pregnancy and hence the incidence of pregnancy related complications such as premature deliveries, low birth weight babies, maternal anaemia and intra uterine foetal deaths [4,5].
Despite the concerted efforts make by the various health authorities to promote the use of ITNs by pregnant women, studies [6-10] have shown that the level of awareness, ownership, and actual use of ITNs/LLIN by pregnant women has varied from one locality or zone to the other. Although the awareness level has improved over time, studies [11] have shown that a lot of factors still militate against actual ownership and correct use of ITNs/LLIN. Insecticide Treated Nets (ITNs) provide effective barrier or shield between the user and mosquitoes or other biting insects thereby protecting against mosquito bites and malaria transmission.
The global incidence of malaria is substantial, with an estimated 300 million suspected cases each year of which one million die. More than 90% of these deaths occur in sub-Saharan Africa where young children are the most affected [12] Malaria is a serious public health problem, causing suffering, deaths and poverty in Nigeria, [13]. It is the third commonest cause of morbidity and mortality, coming after HIV and AIDS and tuberculosis across all age groups, with around 1.5 million malaria cases and approximately 1,000 deaths occurring annually over the past five years [12].
Malaria currently accounts for nearly 110 million clinicallydiagnosed cases per year, 60% of outpatient visits, and 30% of hospitalizations in Nigeria alone [14]. Pregnant women and children are most at risk of malaria transmission and its effects [13]. About 300,000 children die of malaria and over 30 million pregnancies threatened throughout Africa each year [15]. It accounts for 11% of maternal mortality and 12-30% of mortality in children below 5 years in Nigeria, the hardest-hit country in Africa. Malaria in pregnant (MIP) women is a major risk factor of child death in the first month of life [16]. It causes about 15% of maternal anaemia and about 35% of preventable low birth-weight, which is a leading cause of neonatal mortality Centre for Disease Control and Prevention [17]. MIP prevalence in Nigeria is estimated at 48% in 2000 and 2001 [18], and the prevalence in the first, second and third trimester is 37.5%, 47.3%, and 47.5% respectively [19]. However, the use of ITNs/LLIN in Nigeria falls short of global targets. The 2008 Nigeria Demographic and Health Survey (NDHS) results indicate that 17% of households in Nigeria own a mosquitonet (treated or untreated), and 8% of households own more than one mosquito-net. Sixteen percent of households own at least one ever-treated mosquito-net, and 7% own more than one evertreated mosquito-net. The average number of ITNs per household was less than one, which could be attributed to a weak supply and distribution mechanism [20]. Several measures which included use of insecticide- treated nets, indoor residual spraying (IRS), larviciding, environmental management, intermittent preventive treatment in pregnancy and community education were put into action to control both the malaria vectors and parasites, to reduce malaria cases in Nigeria. The Nigerian government distributed free insecticide-treated nets for malaria prevention across its states. Among the available malaria interventions, use of insecticidetreated nets (ITNs/LLIN) finally became the major intervention to limit malaria incidence in our localities. ITNs/LLIN availability was scaled up by way of their free distribution, achieving near 100% coverage of the population at risk of contracting malaria. The distribution of free ITNs/LLIN in Nigeria was meant to support the WHO’s recommendation for universal access to ITNs/LLIN where all people living in malaria affected areas were expected to sleep under ITNs/LLIN every night all year round [21].
Insecticide-treated nets were proven to have a powerful impact on reduction of vector-borne diseases including malaria when used correctly and consistently Roll Back Malaria [22]. Of particular importance is the users’ choice of mosquito net in terms of shape and colour as well as practice to mend them when damaged [23]. This was a major problem in the use of, especially the rectangular ITNs/LLIN. Rectangular mosquito nets are often used where malaria or other insect-borne diseases as well as nuisances are common, especially as a tent-like covering over a sleeping bed. For effectiveness (the potential impact of an intervention, when deployed in real life conditions), the mosquito net must not rest directly on the skin of the sleeping person because mosquitoes can then reach and bite a person through the mosquito net webbing. When they are hung over sleeping beds, rectangular mosquito nets provide more room to the user than conical nets. Rectangular ITNs/ LLIN have been used in several countries in Africa such as Tanzania and Nigeria and their acceptance was good. Evidence from these countries has shown that some rooms in the households were potential sleeping areas which would warrant hanging rectangular ITNs/LLIN during bed time and removing in the morning [24]. Of the available ITNs/LLIN shapes on the market, the people of Nigeria were introduced to rectangular as well as conical ITNs/ LLIN for use in homes to prevent malaria. Conical shaped ITNs/ LLIN were introduced before rectangular ones which implied that the community became used to rectangular rather than conical ITNs/LLIN by the time the latter were introduced ten years later. The mosquito net industries designed and manufactured both rectangular and conical ITNs/LLIN for malaria prevention at homes. The rectangular ITNs/LLIN was introduced to achieve what conical often could not as it reduces body contact between the user and the mosquito net; all in all initially seen as improvements in terms of ITNs/LLIN as a malaria prevention tool. Despite 100% ITNs/LLIN coverage in Nigeria, malaria incidence continued to increase from 49.2% in 2007 to 66.7% in 2008 [25]. Based on the assumption that effective use of ITNs/LLIN in an area with 100% coverage should reduce malaria incidence; it was not clear why this efficiency was not also achieved. This study investigated the use of insecticide treated nets (ITNs/LLIN) and factors affecting their use in malaria control among children under five years of age in Emure LGA, Ekiti State.
Statement of Problem
The success of malaria control with ITNs/LLIN has been bogged down by problems of delivery, distribution, usage and even acceptability of this method in Africa. Public awareness and acceptance of insecticide treated nets varies from community to community in countries where this method of malaria control has been adopted. As a result of poor acceptability of ITNs/LLIN, The public health implication is that more work needs to be done by both the government and health workers in various state to further raise the level of awareness through health education, increase the accessibility and affordability of ITNs/LLIN through mass importation so as to motivate more people to use them and finally to raise the level of formal education through compulsory and free education to secondary level. The burden of malaria, its prevention and control remains a challenge despite the existence of effective technologies [26,27].
Despite the efficacy of these nets, most of people either neglect or ignore usage of bed nets. Malaria vectors start biting by late evening when people are not yet go under bed nets, this represent an opportunity to transmit the disease. Outdoor sleeping is a common habit among student; people who sleep outdoors are exposed to mosquito bites result in developing malaria infection. These are major problem among young people.
Objectives of the Study
Broad objective
The objective of this research study is to assess the knowledge and use of insecticide treated net among Emure Local Government, Ekiti State as a means of prevention on malaria.
The specific objectives are to:
A. Determine the Level of awareness of Insecticide Treated Nets use among mothers in Emure Local Government, Ekiti State.
B. Understand the proportion of under-five sleeping under the ITN every night
C. Identify barriers on utilization of Insecticide Treated Nets use among Emure Local Government, Ekiti State
D. Determine the factors influencing the usage of Insecticide Treated Nets among Emure Local Government, Ekiti State.
Significance of the Study
This study has helped to establish the efficacy of ITNs/ LLIN against the ordinary nets in the reduction of malaria morbidity and incidence (among the vulnerable groups) in the area of study. It has also, confirmed that a cost effective, sustainable and replicable malaria control programmes/strategy in the whole LGA, state or elsewhere in Nigeria is possible and feasible. The result of the present study will however, be used to add to the National malaria morbidity and mortality database and to reinforce the need for a community or nation-wide ITN use and adoption currently advocated for It is hope that if the report of this study is published, it will ensure to create more awareness on use of Insecticide Treated Nets in preventing malaria in our society and encourage its usage, particularly in Emure Local Government, Ekiti State?
Methodology
The study design
This was a cross-sectional descriptive survey of malaria knowledge and prevention practices (especially use of ITNs LLIN) among children in Emure Local Government, Ekiti State [28]. This design was used because of its ability to provide snapshot of the frequency of health related characteristics (such as appropriate insecticide treated nets used) in a defined population at a given point. In addition it is able to make room for planning and allocation of resources./
Area of study
This research was conducted in among the mothers and caregivers of children under age five years of age attending the clinic at the comprehensive health centre in Emure Local Government Ekiti State.
Target population
The target population was all Children under five years of age in Emure LGA of Ekiti State.
Study population
The study population was selected using simple random sampling technique among children under five years of age attending Comprehensive Health Centre Oke-Emure, Ekiti State.
Sample and sampling techniques
A total of 300 respondents were involved in the study by simple random sampling techniques.
Research instruments
Questionnaire was used for data collection. Questionnaires were constructed to seek the opinions of the respondents on the research problem.
Method of data collection
Questionnaire was distributed to the mothers and caregivers at the immunization clinic days in Emure Comprehensive Health Centre, Emure–Ekiti. These questionnaires were duly filled and returned immediately to avoid missing or lost. The illiterates were helped in filling the questionnaires.
Method of data analysis
The data generated through the questionnaires would be analysed in chapter four using method of simple percentage.
Limitation of the study
The study was limited to only mothers and caregivers of under five years old attending government based clinic in Emure town of Emure-Ekiti, excluding the fathers, caregivers of above five years old etc [29].
Ethical consideration
A formal permission was obtained from the concerned authority. Respondents’ consents were gained through verbal introduction of self and explanation of what the study entails before the administration of the questionnaires and confidentiality of the information provided in the questionnaires was guaranteed.
Results and Discussion of Data
This chapter presents findings and discussion of the study. Generally, the findings and discussion will examine utilization of ITNs/LLIN specifically focusing on the intra-household practices in households with children under five. The results presented in this study are based on structured questionnaire use with a random sample of 300 respondents. Insecticide treated nets have been proved to reduce all-cause child mortality by 14-33 percent in rural sub-Saharan Africa. ITNs/LLIN have been promoted to protect the most susceptible to severe malaria: children under five and pregnant women. However, expanded ownership of mosquito nets can make a substantial reduction in malaria morbidity and mortality only if the nets are used and the most vulnerable household members are given priority for sleeping under them. But to what extent are nets that are owned actually used? If a household owns a net, which household members are most, and least, likely to sleep under it? How many family members sleep under a net, and what are the most common groupings under a net? What are the socio-cultural and economic factors within the household affect proper use of the ITNs/LLIN in the household among the under-fives? All answers to these questions will be given in the proceeding sections of this study [30].
Socio-demographic characteristics of the study participants
The socio-demographic characteristics are critical in understanding the results of this study. Using the generic behavioural model of Andersen, they predispose individuals within the household to use or not to use ITNs/LLIN. Description of the basic characteristics of respondents interviewed in this study provides the background for interpreting findings on utilization of ITNs/LLIN in households with children under five. These include; age, marital status, level of education and occupation [31].
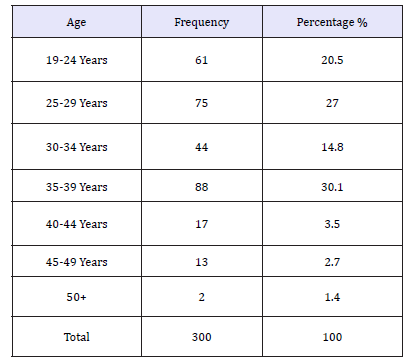
Age of respondents
In terms of age, this study classified the participants into seven age groups with the purpose of trying to reveal how the various age categories varied in their understanding of utilization of ITNs/LLIN among the under-fives. The age of respondents ranged from 19-71 years with the majority aged between 35-39 years comprising of 30.1 percent, followed by those aged between 25-29 years (25.0 percent) and 19-24 years (20.5 percent) as shown on the below Table 1.
Table 1:Age group of respondents.
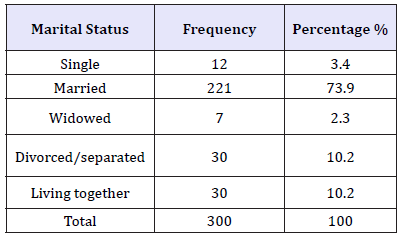
Marital status
Marital status is important in African tradition as children are expected to be raised up in marriage set up due to shared responsibilities between the couples. In terms of marital status, 73.9 percent of the study participants were married, 10.2 percent divorced/separated, 10.2 percent living together/cohabiting, 3.4 percent single and 2.3 percent widowed as presented in the below Table 2.
Table 2:Marital status of respondents
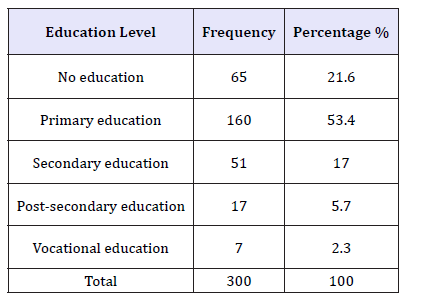
Level of education
Education acts as a mechanism of social-economic transformation especially in the field of child development and health care promotion by people staying in the rural areas who constitute 80 percent of the community population. Wider gaps exist in literacy levels between the urban and rural dwellers in the community. The education levels in rural areas still remain low despite the government efforts to promote education for all (Table 3).
Table 3:Level of education.
Occupation of respondents
Occupation is the basis upon which households are able to survive and meet the daily needs within the household. Occupation also determines the level of income the household is able to have and consequently ability to meet household needs. The respondents in this study community derive their livelihood mainly from farming which is basically subsistence [32].
In terms of occupation, the majority (70.5 percent) of the study participants were engaged in small scale farming engaged in growing of crops like maize, potatoes, sweet potatoes, beans, ground nuts and bananas. These crops are mainly gown for home consumption and surplus is sold for cash. Agriculture in this community is the dominant economic activity for both revenue and employment. However, this sector does not generate sufficient income to sustain households‟ requirements. 30 percent of the study participants were fully house wife. These salaried workers were employed as primary school teachers. The self-employed had small businesses in form of retail shops within the small trading centres. The smallest percentage of respondents was 8 percent which is civil Servant. Generally, majority of the people were engaged in some kind of economic activity that enables them earn a living though not sufficient enough to meet the daily requirements within the households including affordability of ITNs/LLIN (Table 4).
Table 4:Occupation of the respondents.
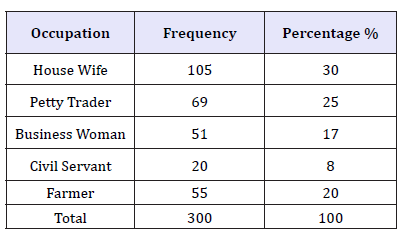
Table 5:Identify the source of ITNs/LLIN.
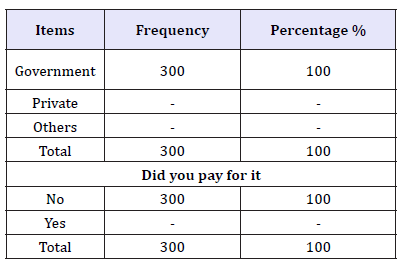
Table 5 above show the sources of Insecticide treated net 100% of the respondents agree that the nets is given to them free by the government of Ekiti State.
Question 5 indicates that all the respondents accept that the ITN/ LLIN were given to them without paying any money to its agents.
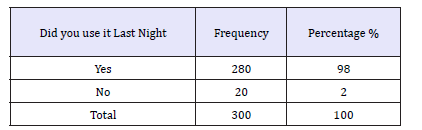
As seen from the Table 6 above, only 10.2 percent had more than 3 nets in their households, 2.3 percent had 3 nets, 5.7 percent had 2 nets and the majority 38.6 percent had only 1 net in the household. This means that the majority of the household members do not have nets as one net cannot be shared among all of them. Number of people under one net was found to range from 1 to 6 people as 22.7 percent slept 2 people in one net, 14.8 percent 3 people and 9.1 percent 4 people in one net. This does not provide for effective usage of the mosquito net due to overcrowding of the net yet most of the net possessed were found to be single as shall be seen in the subsequent sections [33-36]. Respondents were further asked to mention who in the household sleeps under the net. Here, the researcher wanted to know who specifically in the household sleeps in the net to get a clear picture. More than one response was possible as presented in the below Table 7.
Table 6:Ownership of ITNs/LLIN.
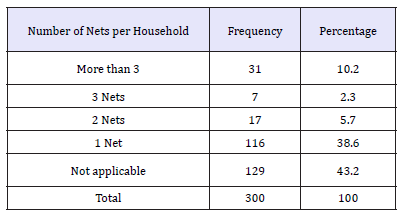
Table 7:Number of respondents that slept under ITN/ LLIN last night.
Ownership of ITNS/LLIN
Mosquito net ownership is rising in sub-Saharan Africa but will substantially reduce malaria only if nets are used and the most vulnerable household members sleep under them. Views were sought on ownership of ITNs/LLIN s in the household which revealed that ownership of ITNs/LLIN in the household is slightly lower than any kind of nets. It was found out that 46.6 percent of the respondents had at least an ITNs/LLIN within the household and 34.1 percent did not have. Whereas knowledge about ITNs/ LLIN was high in this community (61.4 percent) as shall be seen in the coming section, ownership of ITNs/LLIN is very low. More than half of the respondents did not have ITNs/LLIN in their households. A cross examination of the actual nets used in the households reveal the following results in the table below. In order to know the actual type of net used in the household, respondents were cross examined by asking the type of net currently being used in the household. As shown in the Table 8 above, only 35.2 percent were using ITNs/currently treated nets, 1.1 percent ever treated nets and 20.5 percent ordinary nets. Different reasons were given as to why some people were not using Insecticide treated nets. They include; not having money to buy the ITNs (36.4 percent) and stopped using it because mosquitoes had reduced. It was also interesting to find out that some people did not know where ITNs are and others had not bothered to get nets. It should also be noted that ITNs being slightly expensive compared to non-treated nets made some people to buy just ordinary nets and others did not know whether the net was treated or not. For those who knew treated nets mentioned that treated nets have a chemical which can be felt by smell.
Table 8:Types of nets used in the household.
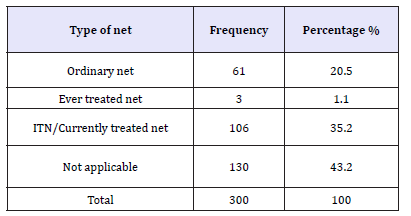
Table 9:Reasons for not using treated mosquito nets in the household.
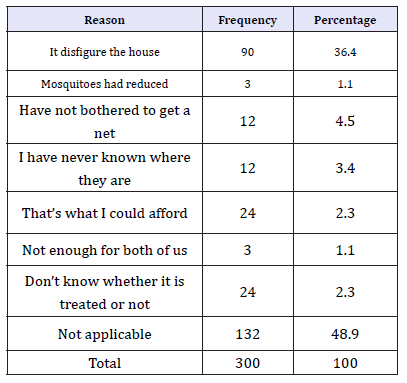
As seen from the Table 9 above, caregivers gave different reasons as to why they were not using mosquito nets. Key informants gave similar reasons as to why some households were not using nets. The community development officer had this to say;
“Some people drink a lot and forget to put on a net. The net can be there but because the husband and the wife come home when drunk, they forget to put it on”
Other reasons mentioned by key informants include; Misconceptions that ITNs/LLIN make someone sweat. “Sometimes I spend the whole night without covering myself, how can I start sleeping in a sack!”
One of the respondents commented. “People have a feeling that mosquito nets cause a lot of heat and therefore make it uncomfortable for someone sleeping in it. Inadequate income to raise money to buy the nets is our major problem. The crops we grow cannot raise money to pay for children’s school fees at the same time buy nets. The house is small to allow net hanging. It needs a house with big rooms. Not readily available. I only saw them once being sold by a hawker who had come from the community. Some people say that when you sleep under the net, you can be affected by the chemicals” (Table 10).
Table 10:Distribution of number of malaria attacks in the past 1 year by use of ITN.
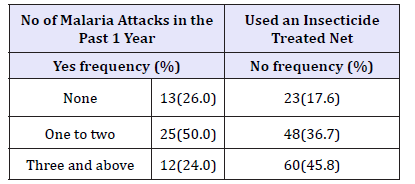
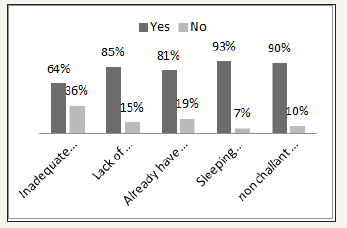
Figure 1 above present respondents’ view about the factors militating against malaria during pregnancy as follows: 64% said inadequate money to get insecticide treated net as a factor that militates against malaria while 36% did not see this as a problem. 85% agreed that lack of proper education on how to prevent malaria is one of the factor that militate against prevention of malaria while 15% did not agree to this. When asked if already having nets on doors and windows with no felt need for ITNs can be a factor, 81% said yes while 19% said no. 93% agreed that sleeping under ITNs produce heat and bad dream, is a factor that militate against the prevention of malaria while 3% did not agree. Finally, 90% agreed that nonchalant attitude towards the use of ITN is one of the factors that militates against the prevention of malaria during pregnancy while 10% did not agree.
Figure 1: Factors militating against the prevention of malaria during pregnancy among respondents.
Discussion
High level of awareness (96.8%) and knowledge of the importance of ITNs/LLIN in killing mosquitoes and preventing mosquito bites by majority (86.0%) of the respondents was demonstrated in this study. A statistically significant association between educational level of respondents and knowledge of ITNs/ LLIN was also observed (x2=120.481, p< 0.001). This is contrary to the findings in a study in Ogun State, Western Nigeria that reported poor awareness (48.9%) and knowledge (31.2%) of the importance of ITNs/LLIN among pregnant mothers. However, similar to the findings in this study, it also reported a statistically significant association between educational level and knowledge of ITNs/LLIN (Abiodun et al., 2012). A low prevalence (27.6%) of ITNs/LLIN use was reported by the respondents in this study, despite the high level of awareness and knowledge of the commodity. Contrary to the findings in this study, a study in Owerri, Nigeria reported high awareness and usage of ITNs/LLIN among pregnant women [29]. The major barrier to ITNs/LLIN use was non-availability as only 36.2% of the respondents in this study own a ITNs/LLIN. However, use of ITNs/LLIN was high (74.6%) among the respondents that own a ITNs/LLIN. A statistically significant association between educational level and ownership (x2=31.138, p< 0.001) as well as use of ITNs (x2=37.133, p< 0.001) was recorded in this study.
While ITNs ownership (36.2%) in this study was lower than that reported in a study among pregnant women by Belay and Deressa (2008) who reported ITNs/LLIN ownership of 59.0%, use of ITNs among the respondents that own ITNs in this study (74.6%) was higher than the ITNs/LLIN usage of 52.1% reported by Deressa et al. Majority 34(50.7%) of the respondents that own ITNs/LLIN in this study bought their nets at the market, 8(11.9%) bought their nets at the hospital, while 17(25.4%) got theirs free at the antenatal clinic. This is in contrast to the findings in the study by Njoroge et al. that reported free/subsidized supply by government as the main source of ITNs/LLIN by 54.6% of the respondents, 24.6% purchased theirs from the health facility, and none of the respondents bought theirs at the market. This highlights the probability of diversion of the ITNs/LLIN from the health facilities to the market in the study area.
On investigating the use of insecticide treated nets (ITNs) and factors affecting their use in malaria control among children under five years of age in Emure LGA, Ekiti State. The result shows that the knowledge on ITNs use and its benefits among parent was very high. Reasons for not using treated mosquito nets in the household; Misconceptions that ITNs/LLIN make someone sweat and that it disfigures the house. All the respondents agreed that their children slept under ITNs, which indicate that the respondents were aware on the use and benefit of ITNs. Finally, all the respondents were given ITNs free of charge by the Ekiti State Government, to reduce mosquitoes and effect of malaria among children under five years in Ekiti State.
Recommendations
Knowledge on ITNs/LLIN to caregivers especially on constant deployment and re-treatment should be enhanced.
A. Ministry of Health should seek assistance and funding to enable a free mass distribution of ITNs/LLIN to increase access in the communities
B. Government should stimulate local ITNs/LLIN industries and social market schemes so that nets are available always
C. Local health facilities should include ITNs/LLIN use issues during antenatal and postnatal clinic session.
D. Local health facilities should encourage mothers and caregivers to use ITNs/LLIN for under five years.
E. The school should teach children from the early stages about ITNs/LLIN use and its benefits.
The household needs to be responsible for their own health and that of their families, get the right tools that fight malaria, keep proper sanitation habit and prevent breeding of mosquitoes by weeding all bushes that hold stagnant water and properly dispose of refuse.
References
- Roll BM (RBM) (2010) Insecticide treated mosquito nets WHO 2001- 2010.
- Abram SB (1995) Control of communicable diseases manual. (16th edn), American Public Health Association, Washington DC, USA.
- Aribodor DN, Nwaorgu OC, Eneanya CI, Aribodor OB (2007) Malaria among primigravid attending antenatal clinics in Awka Anambra State, South Eastern Nigeria. Niger J Parasitol 28(1): 25-27.
- Aliyu AA, Alti-Mu’azu M (2009) Insecticide-treated nets usage and malaria episodes among boarding students in Zaria, Northern Nigeria. Ann Afr Med 8(2): 85-89.
- Brickmann A (1991) Malaria and health in Africa: the present situation and epidemiological trends. Trop Med Parasitol 42(3): 204-213.
- Brooker S, Guyatt H, Omumbo J, Shretta R, Ouma J (2000) Situational analysis of malaria in school-aged children in Kenya: What can be done? Parasitol Today 16(5): 183-186.
- Budy DA, Lwin S, Osika JS, Panneborg CO (2000) What should schools do about Malaria? Parasitology Today 16: 181-182.
- CDC (2007) Vector control. Nairobi, Kenya.
- Cook G, Zumia A (2003) Manson’s disease. (21st edn), Saunders, London, UK.
- DPHO (2007) District monthly report for the year 2007, Eastern Province, Kenya. In: Robert K (Ed.), PHO Igembe district, Kenya.
- Edson F, Kayombo EJ (2007) Knowledge on malaria transmission and its prevention among school children in Keyla District, South-western Tanzanian. Tanzania Health Research Bull 9(3): 207-210.
- Elzubier AG, Ansari EH, Mahgoub HE, Bella H (1997) Knowledge and misconceptions about malaria among secondary school students and teachers in Kassala, Eastern Sudan. J R Soc Health 117: 381-385.
- Fernando SD, Gunawardena DM, Bandara SS, De Silva D, Carter R, et al. (2003) The impact of repeated malaria infections on the performance of children. Am J Trop Med Hyg 69(6): 582-588.
- Fisher AA, Laing JE, Totwnsend JW (1998) Handbook for family planning operations research design. (2nd edn), Oxford University Press inc, New York, USA.
- Jane AA, William AH, Margrette SK, Feiko OK, John EG, et al. (2003) Factors affecting use of permethrin-treated bed nets during a randomized controlled trials in Western Kenya. Am J Trop Med Hyg 68 (4 Suppl): 137-141.
- Jonathan C, William GP, Seth FB, Thierry C, Nathan C, et al. (2004) Infectious diseases. (2nd edn), Elsevier Ltd, Edinburgh, UK, Vol. 2.
- Lengeler C, Cattani J, De Savigny D (1996) Net gain: A new method for preventing malaria deaths. Ottawa International Development Research Centre, WHO, Canada.
- MOH (2006) Malaria in Kenya remains a major public health problem. Message from the Director of Medical Services (Dr. James W. Nyikal) towards The Launch of the New Malaria Treatment Policy and the Scaling up of Malaria Control Interventions, Unpublished report.
- MOPHS (2007) Kenya malaria indicator survey. Division of Malaria Control, Ministry of Public Health and Sanitation, Nairobi, Kenya.
- Meru-North District Development Plan (2008) Effective management for sustainable economic growth and poverty reduction. Government Printers, Nairobi, Kenya.
- Muula AS, Misiri HE (2004) School children’s accessibility to insecticide treated bednets in peri-urban blantyre, Malawi. Afr J Health Sci 11(3-4): 98-102.
- Ndifreke EU, Abraham NG, Aniekan JE (2010) Malaria: knowledge and prevention practices among school adolescents in a coastal community in Calabar, Nigeria. African Journal of Primary Health and Care and Family Medicine 2(1): 103-104.
- Nkuo AT (2006) Environmental factors affecting malaria parasite prevalence in rural Bolifamba, South-West Cameroon. Afr J Health Sci 13(1-2): 40-46.
- Parry E, Godfey R, Mabey D, Gill G (2004) Principles of medicine in Africa (3rd edn). Cambridge University Press, Cambridge, USA.
- Pasvol G (2004) Malaria. In: Cohen J, et al. (Eds.), Infectious diseases, Elsevier Ltd, London, UK, Vol. 2.
- Roy MA, May MR (1992) Infectious diseases of human: Dynamics and control. Oxford University Press Inc, New York, USA.
- Southern Africa Malaria Control and WHO (2005) Malaria control in schools. Information for Action Leaflet. Southern Africa Malaria Update.
- World Bank (2001) Malaria at a glance
- WHO (1995) Vector Control for Malaria and other Mosquito borne Diseases. Report of a WHO study Group. Geneva, Switzerland.
- WHO (1997) Guideline on the use of insecticide-treated Mosquito nets for the prevention and control of the Malaria in Africa. WHO Division of Control of Tropical Diseases, Geneva, Switzerland, Vol. 4.
- WHO (2000) The Abuja declaration on roll back malaria by Africans heads of states and governments, Abuja, Nigeria.
- WHO (2002) Roll back Malaria initiative in Africa region. Monitoring and Evaluation Guidelines (draft) Harare, Geneva, Switzerland.
- WHO (2003) Insecticide-treated mosquito nets interventions. A manual for national control programme managers. Geneva, Switzerland.
- WHO/AFRO (2006) Roll back Malaria and the new partnership for Africa’s development: Is there potential for synergistic collaboration in partnerships? Afr J Health Sci 13(1-2): 22-27.
- WHO (2007) Facts sheets. No. 94.
- WHO (2007) Malaria prevention and control: An important responsibility of a health-promoting school. WHO, Geneva: Switzerland, Vol. 13.
© 2018Owoseni Joseph Sina. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






