- Submissions

Full Text
Perceptions in Reproductive Medicine
Perceptions of Preconception/Interconception Health among Women of Low Socioeconomic Status: Differences by Hispanic Ethnicity
Audra Gollenberg* and Kim Fendley
Shenandoah University, USA
*Corresponding author:Audra Gollenberg, 1460 University Drive, Gregory Hall, Shenandoah University, Winchester, VA 22601, USA
Submission: August 06, 2018;Published: August 10, 2018

ISSN: 2640-9666Volume2 Issue3
Abstract
Background: Maximizing women’s and men’s health prior to pregnancy may reduce the likelihood of adverse pregnancy outcomes including infant mortality, in part because many women recognize their pregnancy late in the first trimester. Low-income women and those without insurance may be at greatest risk for adverse pregnancy outcomes and may be difficult to reach for preconception care. This study aimed to measure the perceptions of preconception health and pregnancy preparation among women of low socioeconomic status.
Methods: Bilingual interviewers recruited and interviewed women of reproductive age (18-40 years) at three agencies that serve a low-income population. Women were asked about how they prepared for their past pregnancies, perceptions of preconception health, as well as recent health behaviors. Qualitative data were transcribed and analyzed thematically and categorized by type of pregnancy preparation.
Results: N=174 women were recruited for the study. Most were non-Hispanic White (42%) or Hispanic (43%) and did not have health insurance (54%). A majority of women (54%) did not prepare for their past pregnancies, and among those who did prepare, “financial” preparation was the most common (13%). Two and a half-times as many Hispanic women (p=0.02) felt no control over getting pregnant as compared to non-Hispanic women, despite having a similar proportion using contraception. Fewer Hispanic women reported using alcohol, tobacco, or marijuana than non- Hispanic women in the pre/interconception period (p=0.01).
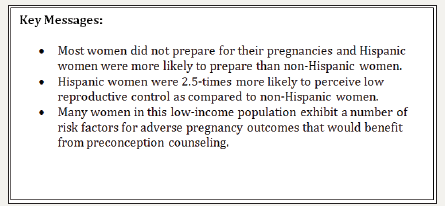
Conclusion: It is important to assess the knowledge, perceptions and health behaviors of underserved populations when designing preconception health promotion programs targeted at these groups (Figure 1).
Figure 1: Key messages.
keywords: Preconception health; Pregnancy preparation; Reproductive health
Introduction
Preconception health (PCH) first gained attention in the 1960s but finally gained traction decades later when the Centers for Disease Control and Prevention (CDC) began recommending health care practitioners integrate PCH into routine care [1]. Since this time many preconception health promotion programs have been initiated for behavior change and have had some success [2,3].
Maximizing women’s and men’s health prior to pregnancy may reduce the likelihood of adverse pregnancy outcomes including infant mortality as behavioral changes made during pregnancy may be too late to be effective [4]. Further, many women continue their unhealthy risk factors into their pregnancies such as caffeine intake, cigarette smoking, alcohol drinking as well as insufficient vitamin use and exercise which may increase the risk for adverse outcomes [5,6].
Specific PCH guidelines encourage women to create and maintain a reproductive life plan; cease illicit drug and tobacco use and limit alcohol use; exercise and eat a healthy diet; consult with a doctor about medication; take a multivitamin with folic acid; ensure vaccinations are up to date; monitor health problems such as diabetes; avoid exposure to environmental toxins; and track family health history [1]. Despite recommendations from the CDC, many women do not prepare for their pregnancies according to these guidelines. Infant mortality rates remain higher in the US as compared to peer nations and marked disparities exist between racial/ethnic groups [7]. As such, the CDC has called for increased consumer awareness and the use of social marketing to better engage all consumers in maximizing PCH for couples [1]. However, it is still unclear how best to package and deliver preconception care for maximum benefit in diverse groups [8].
Further, low-income women and those without insurance may be at greatest risk for adverse pregnancy outcomes and may be difficult to reach for preconception care [9,10]. These women are also at higher risk of unintended pregnancy and of risk factors associated with adverse pregnancy outcomes [9,11]. Research on the perceptions of preconception health among low-income populations is sparse thus necessitating further examination [12,13]. Hispanic women in particular often face socioeconomic disadvantages and have been found to have psychosocial and behavioral risk factors for adverse pregnancy outcomes [14]. The Hispanic population is expected to be the largest minority group by the year 2050 based, in part, on their high fertility and immigration rates [15]. Further, non-English speaking Hispanic women are often left out of medical research studies due to the language barrier making it difficult to better understand their medical needs [16].
In order to develop effective preconception health promotion programs, it is important to gauge the interest and perceptions of high-risk populations. This study aimed to measure the perceptions of preconception health and pregnancy preparation among women of low socioeconomic status with comparisons by Hispanic ethnicity. We hypothesized that most of the women did not prepare for their pregnancies according to PCH guidelines and that planning and health behaviors would differ by age, ethnicity and education.
Methods
From January to April 2017, trained, bilingual interviewers recruited women of reproductive age at three agencies that serve a low-income population: the Free Medical Clinic of Northern Shenandoah Valley, the Special Supplemental Program for Women, Infants and Children, and Healthy Families in Winchester, VA. Eligibility criteria included age 18-40 years and ability to read and write English or Spanish. Women then signed informed consent documents followed by a 15-20min interview. Participants received a Walmart gift card and a gift bag full of information on health resources in the area. The Institutional Review Board at Shenandoah University approved the methodology and procedures.
Perceptions of preconception health and health behaviors were assessed via interview. Women were asked about preconception healthcare, if they felt control over getting pregnant, contraception use, and related questions. To assess if and how women prepared for pregnancies, we asked an open-ended question to allow women to interpret this behavior in their own way. If the respondent provided an answer that indicated she did not prepare for the pregnancy, she was classified as a non-planner, whereas all other responses to this question were coded thematically. They were also asked about multivitamin use, exercise, alcohol, tobacco and marijuana use in the past week. Sociodemographics such as age, race/ethnicity, marital status, health insurance, and number of past pregnancies were also accessed via self-report.
A trained team member entered interview data into a database and a second team member verified this. Bilingual interviewers translated the Spanish interviews. A single researcher completed thematic coding of the qualitative data followed by discussion and analysis of identified themes by two researchers in order to reach agreement. Statistical analysis was completed using SAS University Edition (https://www.sas.com). Where appropriate, quantitative data were tabulated as frequency counts and percentages and chisquare tests were used to test for statistical significance.
Patient involvement
A previous community-based participatory research project with partners in the community informed the design and development of this project.
Results
Table 1:Sociodemographic factors of participant population.
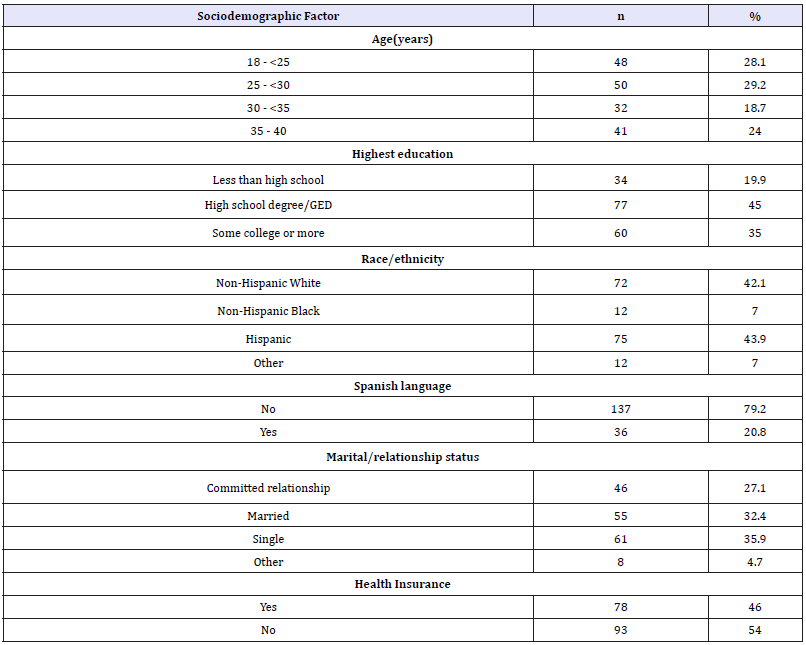
Table 2:Preconception/interconception health factors by hispanic ethnicity.
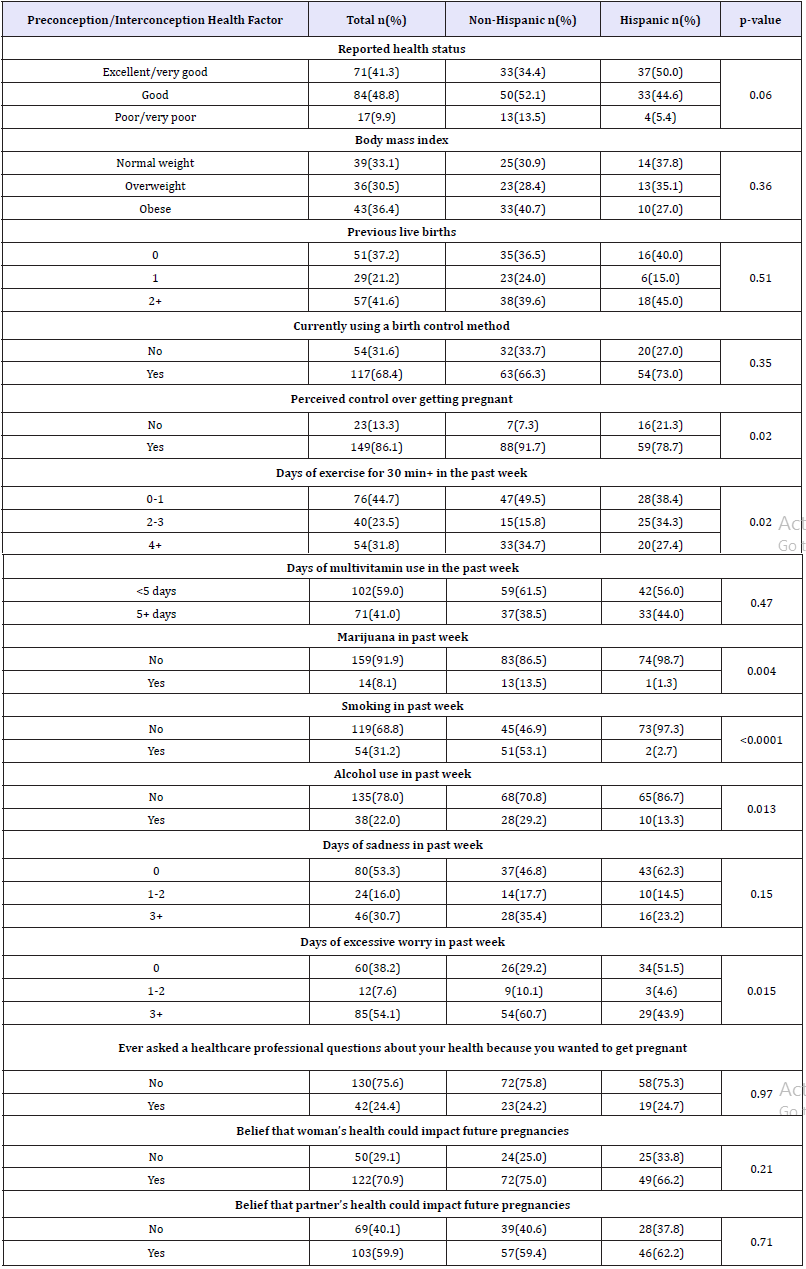
The study team enrolled n=174 women. Most women were < 30 years of age and had a high school education or less (65%) (Table 1). Most women identified as non-Hispanic White (42.1%) or Hispanic (43%) and did not have health insurance (54%). Next we examined preconception health factors by Hispanic ethnicity (Table 2). Nearly 10% of women reported having poor or very poor health status and this was more prevalent among non-Hispanic women vs. Hispanic women (13.5% vs. 5.4%; p=0.06). A relatively high proportion of women were either overweight (30%) or obese (36%), and this differed non-significantly between Hispanic (27% obese) and non-Hispanic women (40% obese; p=0.36). Sixty-eight percent of women were using some form of contraception and the proportion was similar between Hispanic and non-Hispanic women. Moreover, nearly 2.5-times as many Hispanic women perceived no control over getting pregnant (21%) as compared to non-Hispanic women (8%; p=0.02).
The distributions of multiple preconception/interconception health behaviors differed by Hispanic ethnicity. Non-Hispanic women were more likely to exercise 1 day/week or less (49.5 vs. 38.5%) but were also more likely to exercise 4+ days/week (34.7 vs. 27.4%; p=0.02). Use of marijuana (p=0.004), cigarettes (p< 0.0001), and alcohol (p=0.013) were all less prevalent among Hispanic women vs. non-Hispanic women, whereas regular use of multivitamins was similar between these groups. Approximately 1/3 of the women reported feelings of sadness 3+ days of the week and this proportion did not differ by Hispanic ethnicity. However, reported days of excessive worry were more prevalent among non- Hispanic women vs. Hispanic (p=0.015).
Approximately ¼ of the respondents reported asking a healthcare professional questions because they wanted to get pregnant, and the proportions were similar between Hispanic and non-Hispanic women. Seventy-one percent of women believed their current health could impact future pregnancies, and this differed slightly between Hispanic (66%) and non-Hispanic women (75%; p=0.22). A lower percentage of women responded that their partner’s health could impact future pregnancies (60%) and the distribution was similar when compared by Hispanic ethnicity.
Next we analyzed pregnancy preparation behaviors according to Hispanic ethnicity (Table 3). Approximately 1/3 of the women (n=54) had no prior pregnancies, whereas n=119 women had prior pregnancies. Of these women, 56% (n=67) had not prepared for at least some or all of these pregnancies. These women used phrases such as “I didn’t have a plan,” “I was unprepared” or “The pregnancy was not planned” (Figure 2). A higher proportion of Hispanic women reported some preparation for their pregnancies as compared to non-Hispanic women (40% vs. 23%, p=0.01). When comparing the most prevalent types of preparation, financial/job preparation was the most common (13.3%) followed by nutrition/ vitamins (11.6%). Only seven women (4.1%) specifically identified “health” as an important factor in preparing for pregnancy. A greater proportion of Hispanic women specifically reported focusing on nutrition/vitamins as compared to non-Hispanic women (17% vs. 7%; p=0.01).
Figure 2:Qualitative phrases regarding no pregnancy preparation.
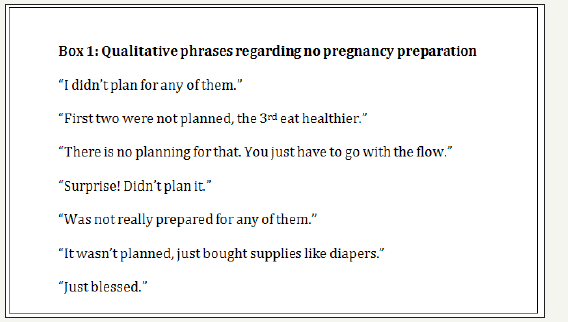
Table 3:Preconception/interconception preparation behaviors for prior pregnancies by hispanic ethnicity.
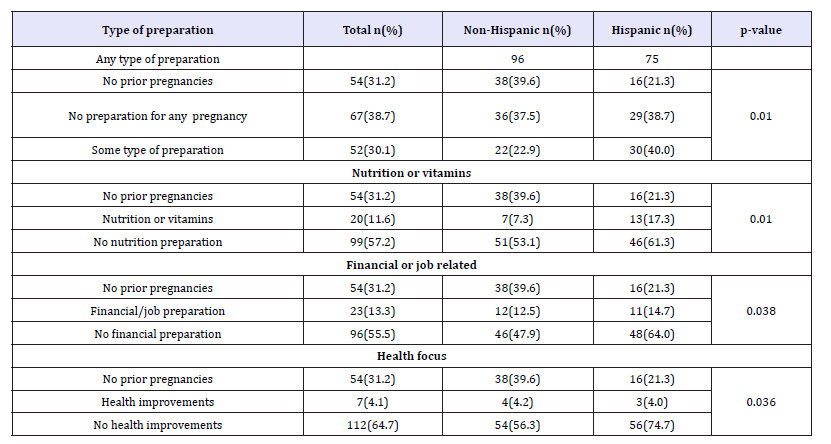
Table 4:Bivariate associations of demographic factors and pregnancy preparations.
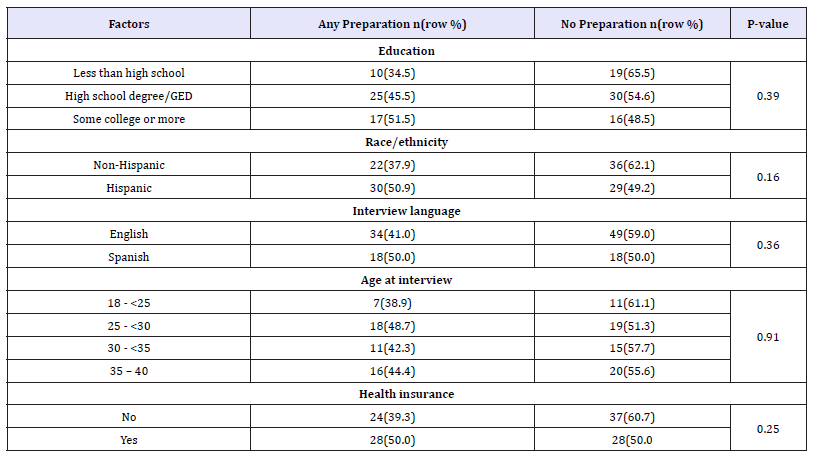
Finally, we analyzed sociodemographic differences between women who identified as preparing for their pregnancies vs. those who did not among those with prior pregnancies (Table 4). While these differences were not statistically significant due to the smaller sample size with prior pregnancies, there were some trends worth noting. Less educated women were less likely to prepare for their pregnancies. For example, 65% of those with less than a high school education did not prepare for their pregnancies vs. 55% of those with a high school education and 48.5% of those with some college or more (Table 4). Non-Hispanic women were less likely to prepare for their pregnancies as compared to Hispanic women (62% vs. 49.2% did not prepare for their pregnancies, p=0.16). Women without health insurance were less likely to prepare for their pregnancies as compared to women with health insurance (60.7% vs. 50%, p=0.25).
Discussion
In this exploratory study assessing the perceptions and behaviors related to preconception health among women of low socioeconomic status, we observed that the majority of women did not prepare for their past pregnancies according to PCH guidelines and they exhibited a number of risky behaviors that could lead to adverse pregnancy outcomes. In addition, we identified a number of differences in preconception health status between Hispanic and non-Hispanic women that may inform the design and delivery of preconception health programs targeted at these groups. In light of the growing emphasis of promoting preconception health to improve both maternal and infant outcomes, we identified a number of factors that may be amenable to preconception counseling in this high-risk population.
Past research has suggested there is a “lack of culture” related to preparing for pregnancy, especially among lower socioeconomic populations [13] and this agrees with the observations in this study. Despite most women having a general knowledge of preconception health recommendations [12,17], many reproductive-aged women still exhibit risky behaviors or health issues that could increase the risk of poor pregnancy outcomes [5,18,19] given the high number of unintended pregnancies in the US [9]. Since many women recognize their pregnancies mid-late into the first trimester, it is imperative to maximize women’s health prior to pregnancy and avoid waiting until prenatal care is initiated to maximize health [20]. In our study, we observed that a majority of women did not prepare for their pregnancies and among those who did plan, the most common way to plan was through financial means, consistent with another study in a similar population [21]. Only 4% of the women specifically mentioned “health” when preparing for pregnancy, suggesting that the concept of preconception health is not well-known in this population. More promotion of the concept of pregnancy preparations as well as preconception health may help this population better take control of risky behaviors and/or poor health prior to conception.
We observed 31% of the population smoked, 22% used alcohol, and 8% used marijuana in the past week. Further, 1/3 of the women experienced sadness on 3 or more days of the week and 54% had excessive worry on 3 or more days of the week. These results are consistent with the social determinants of health of living at/or near the poverty line and with past research in low-income populations [18]. Preconception counseling may help mitigate the adverse effects of substance use, psychosocial stressors, and poor mental health prior to pregnancy in this population. Visits to the healthpromoting agencies are opportunities for healthcare providers to assess and counsel women on these risk factors and how they may impact future pregnancies [22].
In terms of perceptions of preconception health, 13% perceived they did not have control over getting pregnant and this was 2.5-times more common among Hispanic women. This disparity warrants further examination; furthermore, ideally all women would perceive a high level of reproductive control through the development of a reproductive life plan. Those with less than a high school education who indicated no preparation for pregnancy (66%) and Hispanic women who perceive no control over getting pregnant (21%) could perhaps benefit from this assistance. Further, 68% were using some form of contraception, a number relatively consistent with similar populations [23,24]. It is not entirely clear why some women did not feel in control of their reproductive capacity, even among women who reported using some form of contraception. In some cases, their partners may not agree with their use of contraception, or they don’t fully understand their function [23]. Past studies have suggested that some low education populations leave reproduction to faith or chance or believe that it is a natural event [21,25].
We also observed that 29.1% of respondents agreed that their health would not impact future pregnancies while 40% agreed that their partner’s health would not impact future pregnancies. This finding is one that should be replicated in future studies; however, it may suggest that preconception counseling may be needed with this population. A lack of understanding and/or awareness of how various women’s and men’s health factors may influence future pregnancies warrant public health promotion. Some past studies have found a high level of awareness of the importance of maximizing preconception health when asked directly about this concept (90%) [17], whereas we observed a lower proportion (4%) who recognized this concept, albeit through an open-ended question about preparing for pregnancy. More research is needed to clarify how best to inform the population and raise awareness of the importance of improving both men’s and women’s preconception health.
An important limitation to the current study is the self-reported nature of the information collected on perceptions of preconception health and health behaviors. We cannot rule out over- or underreporting on certain types of health behaviors, such as exercise and smoking, for example. However, our rates of health behaviors are similar to what others have reported [11,18] suggesting the rates of false reporting may be minimal or similar to what others have reported.
We sought to engage a population of low socioeconomic status. To minimize participant burden, we did not ask questions on household income. Therefore, it is possible that some participants may fall outside this demographic. However, we recruited our participants at three locations serving specifically low-income populations. It is also worth noting that our participants were women who were seeking help through various health-promoting agencies, thus they may represent a more health-conscious segment of this low-income population.
Our study had the statistical power to compare Hispanic and non-Hispanic populations by their health behaviors and perceptions. A limitation is that distinct Hispanic populations are inherently diverse in their origins, health status and behaviors [26,27]. But we were not able to directly assess these differences. Further, we had very few African-American (n=12) or “other” (n=12) racial/ethnic groups in our study thus limiting our ability to better understand preconception health factors of these groups.
Despite these limitations, our study had several strengths in its design. We were able to conduct over 170 interviews with an underserved population. By involving bilingual interviewers, we were able to include a sizable sample of Spanish-speaking women, a population that is often overlooked in biomedical research. Finally, we addressed a research question that has sparse data available, especially in low-income and Hispanic populations who could benefit tremendously from health promotion programming.
In conclusion, there are many public health implications related to this research. First, it is critical to consider the knowledge, perceptions and health behaviors of underserved populations when designing targeted health promotion programs because such programs must be culturally sensitive and meet women at their current stage of change. Second, many reproductive-aged women exhibit risk factors that may influence maternal/infant health and it is important to address these concerns prior to conception to realize the best outcomes possible. Finally, many women do not realize the connection between poor health and future pregnancy outcomes such that preconception counseling may be an effective means at raising awareness in at-risk populations.
Acknowledgment
Funding for this project was obtained from a Faculty-Student Collaborative Grant from Shenandoah University awarded to A. Gollenberg and K. Fendley. We acknowledge the involvement of over a dozen students in assisting with this research project.
References
- Johnson K, Posner SF, Biermann J, Cordero JF, Atrash HK, et al. (2006) Recommendations to improve preconception health and health care- -United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep 55(RR-6): 1-23.
- Elsinga J, de Jong PLC, Pal-de Bruin KM, Cessie S, Assendelft WJ, et al. (2008) The effect of preconception counselling on lifestyle and other behaviour before and during pregnancy. Women’s health issues 18(6 Suppl): S117-S125.
- Hillemeier MM, Downs DS, Feinberg ME, Weisman CS, Chuang CH, et al. (2008) Improving women’s preconceptional health: findings from a randomized trial of the Strong Healthy Women intervention in the Central Pennsylvania women’s health study. Women’s health issues 18(6 Suppl): S87-S96.
- Mason E, Chandramouli V, Baltag V, Christiansen C, Lassi ZS, et al. (2014) Preconception care: advancing from important to do and can be done to is being done and is making a difference. Reproductive health 11(Suppl 3): S8.
- Anderson JE, Ebrahim S, Floyd L, Atrash H (2006) Prevalence of risk factors for adverse pregnancy outcomes during pregnancy and the preconception period--United States, 2002-2004. Maternal and child health journal 10(6): 575.
- Lassi ZS, Imam AM, Dean SV, Bhutta ZA (2014) Preconception care: caffeine, smoking, alcohol, drugs and other environmental chemical/ radiation exposure. Reproductive health 11 (Suppl 3): S6.
- MacDorman MF, Matthews TJ, Mohangoo AD, Zeitlin J (2014) International comparisons of infant mortality and related factors: United States and Europe, 2010. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 63(5): 1-6.
- Lassi ZS, Dean SV, Mallick D, Bhutta ZA (2014) Preconception care: delivery strategies and packages for care. Reproductive health. 11(Suppl 3): S7.
- Finer LB, Zolna MR (2014) Shifts in intended and unintended pregnancies in the United States, 2001-2008. American journal of public health 104(Suppl 1): S43-48.
- Mohllajee AP, Curtis KM, Morrow B, Marchbanks PA (2007) Pregnancy intention and its relationship to birth and maternal outcomes. Obstetrics and Gynecology 109(3): 678-686.
- Dott M, Rasmussen SA, Hogue CJ, Reefhuis J (2010) Association between pregnancy intention and reproductive-health related behaviors before and after pregnancy recognition, National Birth Defects Prevention Study, 1997-2002. Maternal and Child Health Journal 14(3): 373-381.
- Harelick L, Viola D, Tahara D (2011) Preconception health of low socioeconomic status women: assessing knowledge and behaviors. Women’s health issues: official publication of the Jacobs Institute of Women’s Health 21(4): 272-276.
- Tuomainen H, Cross-Bardell L, Bhoday M, Qureshi N, Kai J (2013) Opportunities and challenges for enhancing preconception health in primary care: qualitative study with women from ethnically diverse communities. BMJ open 3(7).
- Laraia BA, Siega-Riz AM, Gundersen C, Dole N (2006) psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr 136(1): 177-182.
- Zambrana RE, Carter PO (2001) Health data issues for Hispanics: implications for public health research. J Health Care Poor Underserved 12(1): 20-34.
- Frayne SM, Burns RB, Hardt EJ, Rosen AK, Moskowitz MA (1996) The exclusion of non-English-speaking persons from research. J Gen Intern Med 11(1): 39-43.
- Coonrod DV, Bruce NC, Malcolm TD, Drachman D, Frey KA (2009) Knowledge and attitudes regarding preconception care in a predominantly low-income Mexican American population. American journal of obstetrics and gynecology 200(6): 686.e1-7.
- Ayoola AB, Sneller K, Ebeye TD, Dykstra MJ, Ellens VL, et al. (2016) Preconception Health Behaviors of Low-Income Women. MCN the American journal of maternal child nursing 41(5): 293-298.
- D’Angelo D, Williams L, Morrow B, Cox S, Harris N, et al. (2007) Preconception and interconception health status of women who recently gave birth to a live-born infant--Pregnancy Risk Assessment Monitoring System (PRAMS), United States, 26 reporting areas, 2004. Morbidity and mortality weekly report Surveillance summaries 56(10): 1-35.
- Dean SV, Lassi ZS, Imam AM, Bhutta ZA (2014) Preconception care: closing the gap in the continuum of care to accelerate improvements in maternal, newborn and child health. Reproductive health 11(Suppl 3): S1.
- Borrero S, Nikolajski C, Steinberg JR, Freedman L, Akers AY, et al. (2015) it just happens: a qualitative study exploring low-income women’s perspectives on pregnancy intention and planning. Contraception 91(2): 150-156.
- Klerman LV, Jack BW, Coonrod DV, Lu MC, Fry-Johnson YW, et al. (2008) the clinical content of preconception care: care of psychosocial stressors. American journal of obstetrics and gynecology 199(6 Suppl 2): S362- 366.
- Garces PIC, Altarac M, Scarinci IC (2008) Contraceptive knowledge and use among low-income Hispanic immigrant women and non-Hispanic women. Contraception 77(4): 270-275.
- Sangi-Haghpeykar H, Ali N, Posner S, Poindexter AN (2006) Disparities in contraceptive knowledge, attitude and use between Hispanic and non-Hispanic whites. Contraception 74(2): 125-132.
- Mazza D, Chapman A (2010) Improving the uptake of preconception care and periconceptional folate supplementation: what do women think? BMC public health 10: 786.
- Freeman G, Lethbridge CM (2006) Access to health care among Hispanic or Latino women: United States, 2000-2002. Advance data 368: 1-25.
- Hajat A, Lucas JB, Kington R (2000) Health outcomes among Hispanic subgroups: data from the National Health Interview Survey, 1992-95. Advance data 310: 1-14.
© 2018 Audra Gollenberg. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






