- Submissions

Full Text
Perceptions in Reproductive Medicine
Diathermy versus Scalpel in Abdominal Skin Incisions: Systematic Review
Abdelaal N*, Allakwa H, Alhalaby A and Hamdy A
Department of Obstetrics and Gynecology, Menoufia University, Egypt
*Corresponding author: Abdelaal N, Department of Obstetrics and Gynecology, Menoufia University, Egypt
Submission: December 09, 2017; Published: January 31, 2018

ISSN: 2640-9666Volume1 Issue4
Abstract
Objectives: To compare the use of diathermy versus scalpel in abdominal skin incisions to see the variations in post operative pain, incision time, incision blood loss and wound complication rate.
Background: Surgical scalpels are traditionally used for making skin incisions during abdominal surgical operations. The great evolutions in the electrosurgical devices nowadays bring an alternative method for making skin incision by the usage of diathermy skin incision.
Data Sources: Medline databases (Cochrane reviews, PubMed, Medscape, Science Direct) and all materials available in the Internet from 2011 to 2017.
Study Selection: The initial search presented 157 articles of which 8 met the inclusion criteria. The articles were randomized controlled trials compared the use of surgical scalpel versus cutting diathermy in making skin incisions during abdominal operations.
Data Extraction: If the studies did not fulfill the inclusion criteria, they were excluded. Study quality assessment included whether ethical approval was gained, eligibility criteria specified, appropriate controls, adequate information and defined assessment measures.
Data Synthesis: Comparisons were made by structured review with the results tabulated.
Findings: The studies indicated that cutting diathermy could be accepted as an alternative method for abdominal skin incisions.
Conclusion: The studies stated that, the use of diathermy in skin incision during abdominal surgical operations was associated with less blood loss and shorter incision time than the scalpel skin incision. No increase in the postoperative pain and wound complications rate reported with the use of cutting diathermy for abdominal skin incisions.
Keywords: Electrosurgery; Diathermy; Scalpel; Skin incisions
Introduction
Electrosurgery was developed in the early 1900s by the eccentric inventor Dr William Bovie and first used in clinical surgery by Harvey Cushing in 1926. It has since become an integral and evolving part of surgical practice. However, common practice by most surgeons is still to make skin incisions with a scalpel and to divide the deeper tissues with coagulation diathermy [1]. Surgical scalpels are traditionally used in making skin incisions, diathermy incisions on the contrary are less popular among the surgeons, it has been hypothesized that application of extreme heat may result in significant post operative pain and poor wound healing [2]. There has been a widespread use of diathermy for hemostasis but fear of production of large scars and improper tissue healing has restricted their usage in making skin incisions [3]. Nowadays electrodes used in making diathermy incision generate a pure sinusoidal current which produces cleavage in tissue planes without creating damage to the surrounding areas, this is one of the reasons of less damage inflicted to the tissues leading to minimal scar formation [4]. The aim of this review was to compare the use of diathermy versus scalpel in making skin incision during abdominal operations to judge the variations in post operative pain, incision time, incisional blood loss, and wound complications.
Materials and Methods
This review was performed according to the guidelines developed by the center for review and dissemination. It was used to assess the outcome of the studies. The guidance published by the Centre for Reviews and Dissemination was used to assess the methodology and outcomes of the studies. This review was reported in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses statement. An institutional review board and ethics committee approved this study.
Search strategy: we reviewed papers that compared the use of scalpel versus the use of diathermy in making skin incision during abdominal surgical operations, from Medline databases which are (Cochrane reviews, Pub Med, articles in Medscape, Science Direct) and also materials available in the Internet. We used diathermy, scalpel, electrosurgery, cold knife and skin incision as searching terms. The search was performed in the electronic databases from 2011 to 2017.
Study selection
All the studies were independently assessed for inclusion. They were included if they fulfilled the following criteria:
a) Inclusion criteria of the published studies:
b) Published in English language.
c) Published in peer-reviewed journals.
d) Randomized clinical studies that compared cutting diathermy versus scalpel for skin incisions in abdominal surgical operations were eligible for inclusion in this review.
e) If a study had several publications on certain aspects we used the latest publication giving the most relevant data.
Data extraction
Figure 1: The pyramid of evidence- based medicine

All the studies which did not fulfill the above criteria, reported without peer-review, not within national research program, all has been excluded. The studies that compared diathermy versus scalpel in skin incision but not randomized clinical trials were excluded. Also, any surgery rather than abdominal surgery were excluded from this review. The analyzed publications were evaluated according to evidence-based medicine (EBM) criteria using the classification of the U.S. Preventive Services Task Force & UK National Health Service protocol for EBM in addition to the Evidence Pyramid (Figure 1). U.S. Preventive Services Task Force:
a) Level I: Evidence obtained from at least one properly designed randomized controlled trial.
b) Level II-1: Evidence obtained from well-designed controlled trials without randomization.
c) Level II-2: Evidence obtained from well-designed cohort or case-control analytic studies, preferably from more than one center or research group.
d) Level II-3: Evidence obtained from multiple time series with or without the intervention. Dramatic results in uncontrolled trials might also be regarded as this type of evidence.
e) Level III: Opinions of the respected authorities, based on clinical experience, descriptive studies, or reports of the expert committees.
Quality assessment
The quality of all the studies was assessed. Important factors were included; study design, attainment of ethical approval, evidence of a power calculation, specified eligibility criteria, appropriate controls, and adequate information and specified assessment measures. It was expected that confounding factors would be reported and controlled for and appropriate data analysis was made.
Data synthesis
Each study was reviewed independently; obtained data were rebuilt in new language according to the need of the researcher and arranged in topics through the article. Comparisons were made by structured review. A structured systematic review was performed with the results tabulated.
Results
Table 1: Studies included in the review.
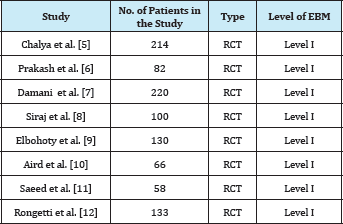
Study selection and characteristics: In total 157 potentially relevant publications were identified, 149 articles were excluded as they did not meet our inclusion criteria. A total of 8 studies were included in this review as they were deemed eligible by fulfilling the inclusion criteria (Table 1) & (Figure 1). The studies were randomized controlled trials compared the use of diathermy versus the use of scalpel in making skin incision in abdominal surgical operations in terms of: incision time, incisional blood loss, postoperative pain and wound complication rate. The studies were analyzed with respect to the study design using the classification of the U.S. Preventive Services Task Force & UK National Health Service protocol for EBM. We reviewed the following parameters in each study:
Table 2: Relation between the type of skin incision and the incision time.
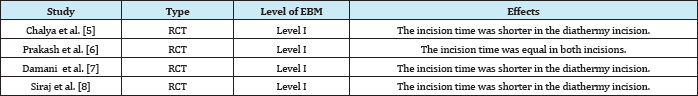
a) Effects of the type of incision on the incision time: Comparison between scalpel and diathermy incision regarding the incision time was reported in 4 studies (Table 2). The incision time was shorter in the diathermy incision in 3 studies [5-8], while it was equal in the both incisions in one study [6].
Table 3: Relation between the type of skin incision and the incisional blood loss.
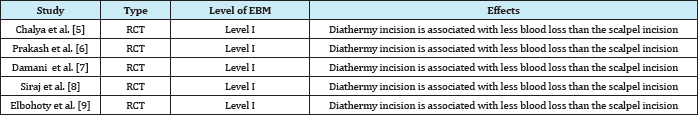
b) Effects of the type of incision on incisional blood loss: Comparison between the both type of incisions regarding the incisional blood loss was founded in 5 studies (Table 3). There was significant difference between the diathermy incision and the scalpel incision regarding the incisional blood loss in the 5 studies [5-9], the incisional blood loss was more in the scalpel incision than the diathermy incision.
Table 4: Postoperative pain in both types of skin incision.
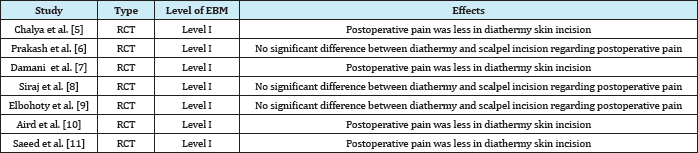
c) Effects of the type of incision on the postoperative pain: Comparison between scalpel and diathermy regarding the postoperative pain scores during the first 24 hours was found in 7 studies (Table 4). In 4 studies [5,7,10,11]; the use of diathermy was associated with decreased post operative pain, while in 3 studies [6,8,9] there was no difference between the two types of skin incision regarding post operative pain.
Table 5: Relation between the type of skin incision and the wound complications rate.
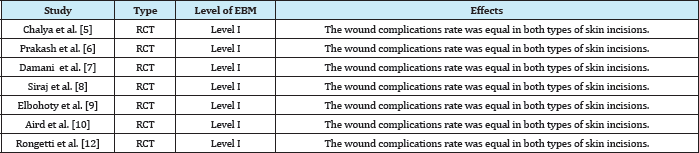
d) Effects of the type of incision on the wound complications rate: Comparison between scalpel incision and diathermy incision regarding the wound complications rate was reported in 7studies (Table 5). In the 7 studies [5-10,12], the wound complications rate were equal in both types of skin incision.
Discussion
Surgical scalpels are traditionally used in making skin incisions, diathermy incisions on the contrary are less popular among the surgeons, it has been hypothesized that application of extreme heat may result in significant post operative pain and poor wound healing because of excessive tissue damage and scarring respectively, secondly, skin incision with the use of diathermy entails increased risk of wound infections in the presence of an underlying prosthetic material [3]. Several studies have shown that diathermy is increasingly being used for making skin incisions, securing hemostasis, dissecting tissue planes and cutting .It facilitates hemostasis , reduces overall intra-operative time and lastly produce a wound that heals similarly as one created by the scalpel [4,8]. In this systematic review, we reviewed the randomized clinical trials that compared the use of scalpel versus the use of diathermy in abdominal skin incisions and published from the period of 2011 to 2017 to see the variations between the two type of incisions regarding incision time, incisional blood loss, postoperative pain and wound complications rate. A total of 8 articles were eligible to be included in this review. In these studies, scalpel incision was generally defined as an incision made through the skin, subcutaneous tissue and fascia with a scalpel. Also, cutting diathermy incision was defined as an incision made through the skin, subcutaneous tissue and fascia. Only, single study [9] in which the cutting diathermy incision started from the subcutaneous tissue after using the scalpel to incise the skin. Postoperative wound complications include all reported wound complications, these included haematoma, seroma, infection and dehiscence. The present review demonstrated that a skin incision can be made more quickly by cutting diathermy than by scalpel, with less blood loss, and no increase in the rate of wound complications or postoperative pain scores. The shorter incision time and lower blood loss are most likely explained by the fact that achieving hemostasis with a scalpel incision requires several instrument exchanges with coagulation diathermy, a disadvantage that is overcome with the use of cutting diathermy. Also, the reduction in the amount of blood loss in the diathermy incision explained by the coagulate effect of diathermy on the microcirculation of the area immediately adjoining the area of the incision [1]. As regards pain intensity, 4 studies [5,7,10,11] in this review demonstrated that diathermy incision was associated with less post operative pain than the scalpel incision; this was contradictory to another review [1] which stated that, no difference between the two types of incision regarding the post operative pain. The decreased postoperative pain in the diathermy incision may be due to the thermal effect of diathermy on the sensory nerve fibers with the subsequent disruption of transmission of nerve impulses. Cell vaporization caused by the application of a pure sinusoidal current leads to immediate tissue and nerve necrosis without significantly affecting adjoining structures [2]. On the other hand, 3 studies in our review [6,8,9] stated that no difference between the two types of incisions regarding the postoperative pain. As regards wound complications rate, in 7 studies [5-10,12], there was no significant difference between the both techniques of skin incision in term of wound complications rate. This was in contrast to previous studies [13-15] which suggested that, wounds created with diathermy have reduced tensile strength, an increased infection rate and a greater zone of wound necrosis histologically than those made with a scalpel. However, not all of these experimental studies differentiated between the use of cutting and coagulation diathermy, and the reported effects appeared to be related more to the use of coagulation diathermy [1].
Conclusion
The use of diathermy for abdominal skin incisions in this review was associated with reduced incisional blood loss and shorter incisional time than the scalpel incision. There was no difference in the wound complications rate between the scalpel and diathermy incision. Also, there was no increase in the post-operative pain with the use of cutting diathermy in abdominal skin incisions. So, the diathermy could be accepted as an alternative method for surgical skin incisions.
References
- Ly J, Mittal A, Windsor J (2012) Systematic review and meta-analysis of cutting diathermy versus scalpel for skin incision. Br J Surg 99(5): 613620.
- Chrysos E, Athanasakis E, Antonakakis S, Xynos E, Zoras OA (2005) Prospective study comparing diathermy and scalpel incisions in tensionfree inguinal hernioplasty. Am Surg 71(4): 326-329.
- Kearns SR, Connolly EM, McNally S, McNamara DA, Deasy J (2001) Randomized clinical trial of diathermy versus scalpel incision in elective midline laparotomy. Br J Surg 88(1): 41-44.
- Ayandipo OO, Afuwape OO, Irabor D, Oluwatosin OM, Odigie V (2015) Diathermy versus scalpel incision in a heterogeneous cohort of general surgery patients in a Nigerian teaching hospital. Niger J Surg 21(1): 4347.
- Chalya PL, Mchembe MD, Mabula JB, Gilyoma JM (2013) Diathermy versus scalpel incision in elective midline laparotomy: A prospective randomized controlled clinical study. East and Cent Afr J Surg 18: 71-77.
- Prakash LD, Balaji N, Sureshkumar S, Kate V (2015) Comparison of electrocautery incision with scalpel incision in midline abdominal surgery-a double blind randomized controlled trial. Int J Surg 19: 78-82.
- Damani SR, Haider S, Shah SSH (2014) Scalpel versus diathermy for midline abdominal incisions. JSP-Journal of Surgery Pakistan International 19(1): 18-21
- Siraj A, Gilani AAS, Dar MF, Raziq S (2011) Elective midline laparotomy: comparison of diathermy and scalpel incisions. Professional Med J 18: 106-111.
- Elbohoty AEH, Gomaa MF, Abdelaleim M, Abd-El-Gawad M, Elmarakby M (2015) Diathermy versus scalpel in transverse abdominal incision in women undergoing repeated cesarean section: A randomized controlled trial. J Obstet Gynaecol Res 41(10): 1541-1546.
- Aird LNF, Bristol SG, Phang PT, Raval MJ, Brown CJ (2015) Randomized double-blind trial comparing the cosmetic outcome of cutting diathermy versus scalpel for skin incisions. Br J Surg 102(5): 489-494.
- Saeed S, Ali A, Zainab S, Khan MTJ (2017) Scalpel versus diathermy of midline skin incisions: comparison of mean pain scores on second post operative day. J Pak Med Assoc 67(10): 1502-1505.
- Rongetti RL, Castro PTO, Viera RA, Serrano SV, Mengatto MF, et al. (2014) Surgical site infection: an observer-blind, randomized trial comparing electrocautery and conventional scalpel. Int J Surg 12(7): 681-687.
- Loh SA, Carlson GA, Chang EI, Huang E, Palanker D, et al. (2009) Comparative healing of surgical incisions created by the PEAK Plasma Blade, conventional electrosurgery, and a scalpel. Plast Reconstr Surg 124(6): 1849-1859.
- Vore SJ, Wooden WA, Bradfield JF, Aycock ED, Vore PL, et al. (2002) Comparative healing of surgical incisions created by a standard �bovie,� the Utah Medical Epitome Electrode, and a Bard-Parker cold scalpel blade in a porcine model: a pilot study. Ann Plast Surg 49(6): 635-645.
- Ozgün H, Tuncyurek P, Boylu S, Erpek H, Yenisey C, et al. (2007) The right method for midline laparotomy: what is the best choice for wound healing? Acta Chir Belg 107(6);682-686
© 2018 Abdelaal N. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






