- Submissions

Full Text
Perceptions in Reproductive Medicine
Maternal Profile, Assisted Reproductive Technology, and Perinatal Health Indicators
José Manuel Terán*
Department of Biology, Madrid Autonomous University, Spain
*Corresponding author: José Manuel Terán, Department of Biology, Faculty of Sciences, Madrid Autonomous University, c/Darwin, 2, 28049 Madrid, Spain
Submission: September 20, 2017; Published: December 13, 2017

ISSN: 2640-9666Volume1 Issue3
Abstract
Birthweight and its different classifications are related to different health problems later in life. Although the underlying mechanisms affecting birthweight are not well understood, one of the most interesting social factors affecting birthweight is age at maternity, although it is not possible to analyse age at maternity without analysing both level of education of the mother and the maternal occupation. In the last decades, age at maternity has increased in developed countries, increasing the number of mothers who are older than 35 years old and older than 40 years old, with a parallel increase of mothers who are highly educated and with high-income occupations. The delay of age at maternity is demonstrated to increase the prevalence of negative pregnancy outcomes as low birthweight (LBW) or small for gestational age (SGA), and is related to higher number of pregnancies by assisted reproductive technology (ART), fact that could partly explain higher number of multiple births. Nevertheless, higher-income occupation and higher level of education are related to better pregnancy outcomes. A simple directed acyclic graph is drawn to give an example of the possible relationships among age at maternity, multiple birth, and assisted reproductive technology and pregnancy outcomes.
Keywords: Age at maternity; Multiple birth; Birthweight; Small for gestational age; Large for gestational age; Low birthweight; Assisted reproductive technology
Introduction
Birthweight is an important perinatal health indicator related to neonatal and infant mortality (Wilcox, 2001). Further, different classifications of birthweight such as LBW (weight at birth under 2,500 grams), macrosomia (weight at birth upper than 4,000 grams), small for gestational age (SGA: birth weight for gestational age under 10th percentile of a weight for gestational age reference), and large for gestational age (weight at birth upper than 90th percentile) are related to health later in life [1]. Although the effect of birthweight and its different classifications on health in advanced stages of human life are day by day well understood, primary causes and aetiology of the different classifications of birthweight are not. Among aetiology of LBW, macrosomia, SGA and LGA, it is possible to discern between genetic factors such as genetic variants or sex of newborn, socioeconomic factors such as level of education, occupation, and socioeconomic status of the parents, and maternal- foetal factors such as age at maternity, parity, type of birth (vaginal or by Caesarean section-CS-), multiple gestation or origin of the mother. Regarding to genetic factors, Andersson et al. [2] and Yaghootkar & Freathy [3] showed a significant association among different loci, birthweight, and different adult phenotypes as type 2 diabetes, adult height, and adult blood pressure. With respect to socioeconomic factors, recent studies showed an association among higher qualified workers, higher income and higher educational level with higher mean birthweight and lower prevalence of LBW [4,5]. On maternal-foetal factors, both newborns from young and advanced age mothers, primipara mothers, newborns by CS delivery, and newborns from multiple gestation are more likely to have LBW [6].
Discussion
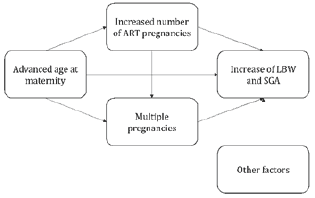
In the last decades, the reproductive behaviour has been changing. Age at maternity has increased in developed countries, increasing the number of mothers who are older than 35 years old and older than 40 years old. The effects of the delayed age at maternity suppose high prevalence of LBW [7]. Further, if age at maternity is accompanied by an increase in the number of pregnancies by assisted reproductive technology (ART), due to this delay in age at maternity, it could be possible to expect a higher increase in the prevalence of LBW and SGA. This possible increase in the prevalence of these indicators could be due to the increased risk of having multiple pregnancies due to ART when multiple embryos are transferred. Nevertheless, singletons born by ART show also higher risk of being LBW or SGA when compared with naturally conceived singletons [8], so, is the increase of pregnancies by ART the factor that could explain the increase of the prevalence of LBW or SGA? Or, could be the delay of age at maternity one of the main factors that increase these indicators? Both questions could be answered with the following directed acyclic graph (DAG), in which an increased number of ART pregnancies could be explained by an increase in the age at maternity, both factors affect both number of multiple births and these three risk factors increase the number of LBW and SGA. Nevertheless, this DAG is only an example of one of the possible relationships among ART and advanced age at maternity (Figure 1).
Figure 1: Hypothetical DAG illustrating relationships among advanced age at maternity, ART and perinatal outcomes.
On the other hand, maternal profile have been changing in developed countries to mothers highly qualified (university level education), and to mothers with higher-income occupations, maternal characteristics that contribute to decrease the prevalence of LBW, SGA [9].
Conclusion
The opposite trends of delaying age at maternity-increasing prevalence of LBW and SGA-, and the increasing number of women with higher occupation and level of studies-decreasing prevalence of LBW and SGA- lead researchers to investigate the effect and relationships among these risk factors, such as ART pregnancies, advanced age at maternity, number of multiple births, and protective factors as higher-income occupation higher qualification on the labour outcome.
References
- Bukowski R, Davis KE, Wilson PW (2012) Delivery of a small for gestational age infant and greater maternal risk of ischemic heart disease. PLoS One 7(3): e33047.
- Andersson EA, Pilgaard K, Pisinger C, Harder MN, Grarup N, et al. (2010) Type 2 diabetes risk alleles near ADCY5, CDKAL1 and HHEX-IDE are associated with reduced birthweight. Diabetologia 53(9): 1908-1916.
- Yaghootkar H, Freathy RM (2012) Genetic origins of low birthweight. Curr Opin Clin Nutr Metab Care 15(3): 258-264.
- Juárez S, Revuelta Eugercios B (2013) Socioeconomic differences in low birthweight: revisiting epidemiological approaches. Rev EspInvestig Sociol 144: 73-96.
- Varea C, Terán JM, Bernis C, Bogin B, Gonzalez-Gonzalez A (2016) Is the economic crisis affecting birth outcome in Spain? Evaluation of temporal trend in underweight at birth (2003-2012). Ann Hum Biol 43(2): 169182.
- Kramer MS (1987) Determinants of low birthweight: methodological assessment and meta-analysis. Bull World Health Organ 65(5): 663-737.
- Astolfi P, Zonta LA (2002) Delayed maternity and risk at delivery. Paediatr Perinat Epidemiol 16(1): 67-72.
- Sazonova A, Kallen K, Thurin-Kjellberg A, Wennerholm UB, Bergh C (2011) Obstetric outcome after in vitro fertilization with single or double embryo transfer. Hum Reprod 26(2): 442-450.
- Wilcox AJ (2001) On the importance--and the unimportance--of birthweight. Int J Epidemiol 30(6): 1233-1241.
© 2017 José Manuel Terán. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






