- Submissions

Full Text
Perceptions in Reproductive Medicine
Is “Unconsummated Marriage” Still an Appropriate Term? A Snapshot of Reality
Silvaggi M1*, Michetti PM1,2, Rossi R1, Fabrizi A1,3, Tripodi F1 and Simonelli C1,4
1Institute of Clinical Sexology of Rome (ISC), Italy
2Department of Urology, Sapienza University of Rome, Italy
3Tor Vergata University of Rome, Italy
4Department of Psychology, Sapienza University of Rome, Italy
*Corresponding author: Silvaggi M, Institute of Clinical Sexology of Rome (ISC) via Savoia 78, 00198 Rome, Italy
Submission: September 18, 2017; Published: November 13, 2017

ISSN: 2640-9666Volume1 Issue2
Abstract
The most shared definition of Unconsummated Marriage (UM) refers to "the failure to perform successful sexual intercourse at the beginning of the marriage. UM usually occurs in the first few nights of marriage and so it is frequently referred to as "honeymoon impotence” or "wedding night impotence”. In the Middle-Eastern (MES) and Western (WS) societies, sexuality follows different patterns in terms of meaning and rules. Moreover the evolution of societies all around the world created new contexts and kinds of relationship. This could hamper a correct taxonomy of such sexual dysfunction where a social variable seems crucial.
Aim: To analyze and review data on UM all around the world, to understand if in different societies it refers to the same situation.
Method: A review of published literature on UM from 1970 to date, was conducted.
Results: Substantial difference emerged from MES to WS. In MES, sexuality is allowable only in marriage, while in WS sexuality and relationship are not strongly linked. This could suggest that the term "marriage” is unable to cover the phenomenon in such different countries. Moreover, the average time before the consultation, causal attribution and prevalence are very different in Western and Middle Eastern countries.
Conclusion: We found that the term "first attempts dysfunction” could be better used to describe male, female or both difficulties related to ignorance about sexuality or state/performance anxiety. On the other hand over the individual category of sexual dysfunctions, we suggest a new term as "Unconsummated relationship”, where individual difficulties toward sexuality are involved creating a couple's dysfunction.
Keywords: Unconsummated marriage; Honeymoon impotence; White marriage; Vaginismus; Infertility
Introduction
The expression Unconsummated Marriage (UM) or white marriage [1] arises from the legal and religious texts as a cause of annulment of the marital link for Catholics. This concept gave priority to the reproductive aspects of sexuality and was used in a derogatory way (to refer to the sexual life of the couple). Nowadays the most shared definition refers to UM as the failure to perform successful sexual intercourse at the beginning of the marriage [2]. It usually occurs in the first few nights of marriage and so it is frequently referred to as "honeymoon impotence" or "wedding night impotence" [3]. As shown in Table 1, we found different definition of what is known as UM and their differences reflect in some way the cultural context where such definitions are used.
Table 1: Definitions of UM.
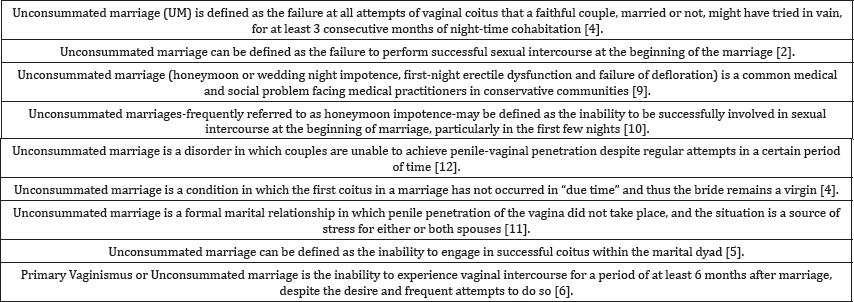
These definitions are very different each other, some of them do not consider the marriage as needed [4] others take it for granted [2,5,6] and suppose the bride is virgin [7-9]; someone refer to a minimum time of three or six months [5,6], others to a few nights [10]; someone indicates the male as responsible of UM [9], while others indicate the woman or the couple [5,6]; Raham et al. [11] consider the necessity that there is stress for one of the two or the couple to identify UM, while Zargooshi [7] underlines the "due time” to have the first intercourse. In Eastern scientific literature, we found a few studies using the term "UM”, more in Indian area in case of Vaginismus [5], while in case of male difficulties terms like "newly weds Erectile Dysfunction” or "honey moon Erectile Dysfunction” are used [12,13]. In African scientific literature we did not find any study about UM.
Moreover, this condition appears to show great internal variability depending on the etiology, duration and cultural context in which it occurs; also within the same cultural system we can see very different beliefs and needs toward sexuality. In some areas of Western societies, for instance, where there is more cultural isolation or strong traditional religious beliefs, sexuality follows strict roles, while in some Middle-Eastern cities we can see that sexuality is more and more independent from traditional beliefs and law. Furthermore, all around the world we live in multicultural societies. In Western countries live many people of Middle Eastern and Eastern culture, with their habits and traditions, and in the Eastern and Middle Eastern societies, Western values and habits are often transmitted and disseminated by the mass media. For these reasons, clinicians are exposed to sexual problems not always according to the dominant culture in their environment. Therefore, it seems that more specific terminology on UM and/or difficulties in achieving firsts sexual intercourses, is needed.
Aim
The aim of the present study is to provide a spread collections of data on UM and Honeymoon Impotence, in order to understand if these terms in different societies refers to the same condition and if these terms are suitable in clinical setting all over the world. Whether-as expected-a different pattern of conditions will emerge, a further aim is to recognize specifiers of the different conditions and to identify the most accurate terms to classify them. It might improve the communication among researchers from different areas of the world and promote a better knowledge and skills sharing.
Method
A review of published literature on UM from 1970 to date, was performed using Pubmed psychinfo and Psycharticles.
Cultural aspects in UM
In, Middle-Eastern or Western societies sexuality follows very different patterns in terms of meaning and roles. Sharp cultural discrepancies between these societies, like conservatism, religion, and feudal social structures were claimed to be responsible of UM [12]. However the evolution of the societies all around the world created new contexts and kinds of relationship. People experiencing sexual difficulties front very different situations with respect to the geographical area, social level and cultural system where they live.
UM seems to be very common in the conservative Middle- Eastern societies and in the developing countries, where couples are strongly prevented by religious rules and cultural taboos from sexual experiences before wedding [2,14]. Zargooshi [7] suggests that in societies in which there is large opportunity for premarital coitus, UM is extremely rare. This is in sharp contrast to conditions in countries like Iran, where sex before marriage is considered scandalous and it is an insult to family honor. In many cases, especially in rural areas, this can involve the subsequent murder of the woman by her family, and most of those escaping this fate are then considered anyway unsuitable for marriage [15].
Although we do not have any quantitative research about rising of sex activity before marriage in Middle-Eastern society, we know that the norms about the acceptability of sex activity before marriage are changing in some way, and that this change may be due to the effect of globalization on family, culture, peers, media and economic status that are underlined as social factor on pre-marriage sexual activity [16]. According to this point of view about globalization and modern life style, and observing people with sexual dysfunction, Ozdemir [12] found high rates of nonconsummation despite their modern way of living in big cities, far from conservative life-styles, and that was in contrast with the reports in the literature. The Author suggested that being residents in Istanbul (86%), belonging to high-income groups (97% medium or high level of income), and a minor rate of being housewives (23%) did not appear to make a big difference.
In Western cultures, where marriage is not the only way of access to sexuality, it is still possible to observe some difficulties at the first intercourse in new relationships or more in "one night stand” situations. These difficulties are favored by a certain ignorance about sexuality, not attributable in these cases to the laws and limits of the society where these people live, rather to their personal attitudes and psychological difficulties toward sexuality [17]. Moreover, although there is not a psychological pressure from their families to have sex, very often we see young people experiencing sexual difficulties when forced by the media and peer to have sex even if they do not feel ready for it, or when the situation is uncomfortable. Furthermore, even if they can have privacy and intimacy, the increasing frequency of comments on social networks about sexual experiences, could make them feel always under the eyes of their target community that pushes them to be sexually active and that discredits those who do not achieve such goal. These conditions, combined with myths about sexuality, conveyed by mass media and porn, favor the appearance of sexual difficulties then in males are often Erectile Dysfunction (ED) and Premature Ejaculation (PE) and in females Genito Pelvic Penetration Pain Dysfunction (GPPPD) with risk of secondary Vaginismus onset, or Arousal and/or Orgasmic Disorders, while for both we can expect a decrease in sexual desire and avoidance of sexual behavior. Then it seems that in UM cases, personal difficulties are reinforced by specific characteristics of the society where people live (eg., sexual script, legal aspects or traditions).
So, in both cultural systems we found risk factors able to lead the onset of sexual difficulties that may hinder the intercourse. With respect to pressure to solve the problem, a difference between modern or traditional societies emerges. In fact, within traditional societies, like Orthodox Jewish, wedding ceremonies often function as symbolic consent for physical intimacy between individuals expected to have minimal or non-existent premarital sexual experience. One such society, Orthodox Judaism, takes a step beyond permission and openly expects new brides and grooms to engage in sexual intercourse on the first night of marriage or soon thereafter, despite stringent norms forbidding premarital physical contact. Any delay for more than several weeks in consummating a marriage is seen as problematic and worthy of rabbinic or professional attention. Muslims too expect new brides and grooms to engage in sexual intercourse on the first night of marriage or soon thereafter, despite stringent norms forbidding premarital physical contact. Any delay of more than a few weeks in consummating a marriage is seen as problematic and worthy of professional attention [8].
This social pressure is very different for Western countries, where sexuality is a couple's issue, and it could be the reason we see such differences in UM's time to consultation [18]. The fact that there has not been any publication on UM from sub-Saharan Africa could be a reflection of lack of awareness among the general population and the health care providers too. It may also be due to the fact that in some communities there are culturally acceptable and sanctioned mechanisms of resolving such problems without exposing the concerned individuals [19].
Etiology and comorbidity
Usually, the spouses had no intercourses with penetration before marriage, neither with the mate nor with other previous partners [12]. Lifelong Vaginismus has been traditionally reported as the leading cause, linked to secondary male ED [7,20], but also ED is in turn a leading cause for UM [16]. In these patients, ED has often psychogenic origin [21] and it may be primary or secondary to Vaginismus [22]. Kaplan [20], who first discussed extensively the UM topic, believes that female sexual dysfunction, particularly Vaginismus, could be considered as primum movens in this couple sexual problem. In these cases, as a result of repeated failures in an attempt to penetration, the man often develops an ED, which can perpetuate even after the Vaginismus has been successfully treated [23,24]. Despite the link between UM and individual sexual dysfunctions some authors from non Middle-Eastern societies (Italy and Argentine), suggest that UM is an independent clinical entity that should be differentiated from the individual etiology of the case (such as Vaginismus, phobias, or Erectile Dysfunction) for its proper treatment [25].
Most of authors refer that the underlying psychosexological cause in UM is sexual anxiety, which shows up as coital phobia, Vaginismus, Dyspareunia, ED, and ante portam Premature Ejaculation [3,7,9,10,18,25-32]. Ribner & Rosenbaum [18]; Bardan [9]. Anxiety gets involved in both members of the couple and should be treated and solved accordingly [32].
Michetti et al. [17] suggest that in UM there is no unique responsible gender: both husband and bride can report in personal history a difficulty in the sexual sphere. Moreover, UM should not be considered the result of sexual dysfunctions that start at the beginning of the marriage, but the matching of individual difficulties.
Middle-Eastern authors reported some cultural specific risk factors as: misconception about pain and bleeding and breaking the hymen for a female virgin; the responsibility of breaking the hymen and performing intercourse for the male [33]; shocking change from forbidden physical contact to intercourse-obligation [34]; couple's urge to consummate in the wedding night, living in the same house with the family [9]; poor knowledge about sexuality, social pressure to consummate and proof [35]; homosexual orientation with no desire to have sex with women including their bride.
Moreover, Bardan [9] and Zargooshi [7] underlined some worldwide risk factors like performance anxiety, fear of sexual failure and fear of being rejected by the partner. In particular, rejection by an intimate partner is a salient fear for individuals with high social anxiety and/or Social Anxiety Disorder (SAD), since feelings of closeness to a partner can serve as an indicator of one’s social inclusion and acceptance [36]. Individuals with high social anxiety might fear and feel compelled to limit the development of intimacy in their relationships for a number of self-protective and relationship-protective reasons. Individuals with high social anxiety and SAD avoid self-disclosure (e.g., Meleshko & Alden [37]; Sparrevohn & Rapee [38]) and have difficulty in expressing personal beliefs, intentions and preferences to their intimate partners for fear of being rejected or abandoned [39-41]. This pattern of interpersonal difficulties is spread in Western societies and appears as an important risk factor for UM because highly socially anxious individuals tend to fear rejection [42].
Previous research (e.g., Sparrevohn & Rape [38]; Bodinger et al. [43]) has demonstrated that socially anxious individuals report lower satisfaction with various aspects of their relationships, including lower sexual satisfaction, in comparison to non-anxious individuals. Moreover a good communication about sexuality within the couple is related to a better intimacy and sexual satisfaction [39,44].
In Western and Middle-Eastern or Eastern societies people feel social pressure about their sexuality resulting in different forms of social anxiety. In Western cases, pressure is caused by myths from mass media and need to be at any time sexually active for men and sexually seductive and "ready” for women, while in Middle-Eastern or Eastern societies pressure seems to come from religious and social restriction and rules around sexuality [7]. Moreover, although around the world we can find very different cultural context and relationship pattern where sexual intercourse is socially allowed, we can observe that social anxiety [45], poor knowledge about sexuality, poor sexual experience, pressure to have an intercourse as soon as possible and lack of privacy and poor sexual communication and intimacy are worldwide risk factors for sexual dysfunctions, able to prevent a sexual intercourse never had before. Moreover the anticipation of failure based on past experience seem to be a frequent maintaining factor [46].
Prevalence
There are no recent available statistics about UM in the Western medical literature. The lack of information is either because it is not a recognized entity in disease taxonomy or because it is sometimes erroneously classified as Hypoactive Sexual Desire Disorder (HSDD) sexual phobia, or similar [12]. Establishing the frequency of UM is difficult because it can last over variable time spans and also because many couples avoid consultation. One is the reluctance of the couples to admit the problem due to their feelings of guilt, shame, or inadequacy, which causes a conflict between their needs to seek help and to conceal their difficulty [25,28,47].
Western data are very rare; Kinsey (1953), in a survey that took into account a significant amount of cases, pointed out that approximately 2% of couples are incapable of consummating the intercourse [25]. In Middle-Eastern UM appears to be a significant problem with a prevalence from 8 to 24%of the sexual and andro- gynecological visits [2,3,35,48].
Comparing such different conditions some question emerge about the relevance of marriage in this condition. While Ozdemir [12] noted that in their sample majority of woman was married (93%) in Argentinean study [25] only 49% was married, 10% was engaged (non cohabiting) and 30% was in cohabitation. Then, a marriage seem not needed worldwide to identify a couple's dysfunction as UM. Moreover, in Western studies on lifelong Vaginismus, only a part of the women were married. For example in a Canadian study [49] only 27% of women with lifelong Vaginismus was married and 33% had no relationship at all. Considering the cultural context observed in literature, we can suppose that in Middle-Eastern societies those cases should be diagnosed as cases of UM, and this difference and the lower social pressure about couple's intimacy could explain part of such different prevalence rating.
Duration of UM
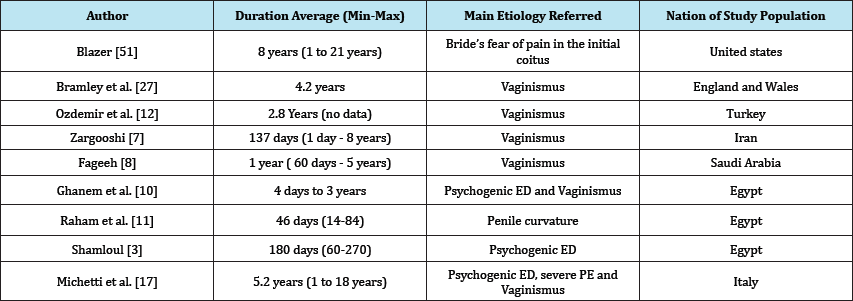
In Michetti et al. [17] UM observed cases had a longer lifetime in respect to Middle-Eastern cases. It could depend on a different cultural context: while in Eastern societies parents have a strict control on sexual activity and time for procreation after marriage, in Western societies this issue remains mainly under the control of the couple; therefore the couple calls for help later. Referring to the call for help, the predominance of female initiative agrees with the literature data about all kinds of sexual dysfunctions [50]. Anyway, we found short or long time duration in both cultural systems and the difference seems related to different patient characteristics and kind of sexual dysfunctions. In fact, as shown in Table 2, where the main etiology is Vaginismus the duration is longer, while where the sexual dysfunction is male ED or PE the time to consult is shorter [51-53].
Table 2: Duration and main etiology referred of UM..
Discussion
A substantial difference emerged from our research between Middle-Eastern and Western societies in terms of sexual roles and laws about sexuality. In Middle-Eastern societies, sexuality is allowed only in marriage, while in Western society people can get a relationship with or without sexuality for the whole life or have sexuality with or without a relationship. This could suggest that in "Unconsummated Marriage" expression, the term "marriage" is unable to cover the phenomenon in such different countries. Moreover, the mean time to consultation in Middle-Eastern societies is more likely to be from one day to a few and to have a male etiology, while in Western societies the time is around five years, with a female or both shared etiology. Therefore the term "Honeymoon" in the expression "Honeymoon Impotence" seems not always appropriate because of the duration time and the term "Impotence" could be not appropriate because of the exclusion of female etiology. However, these differences are not strictly linked to cultural differences and seem not able to create specific sexual dysfunctions.
In fact, we can also find in Western society a sexual dysfunction arising because of social pressure to have an intercourse as soon as possible and in Middle-Eastern society a UM because of individual or couple's avoidance of sexuality after marriage. So it seems that the cultural system where the dysfunction emerge is not reliable as a marker of different dysfunctions that make the intercourse impossible. Then, we think UM is not still an adequate term, because it does not distinguish very different situations such as psychogenic ED or Ante portam PE in first night of marriage - due to poor knowledge, strong pressure and lack of privacy - from Vaginismus, Dyspareunia or male sexual dysfunctions due to severe psychological impairment or medical conditions. The term UM is inadequate to include new forms of relationship like cohabitating or non cohabiting couples and then it does not permit a comparison between same sexual dysfunctions from different cultural systems.
Conclusion
Separate different situations
We purpose to distinguish between two different situations:
a. "Honeymoon impotence" where time to consultation is short (less than 6 months) and sexual difficulty is most often a male ED or a severe PE. Here there is a strong pressure to consummate as soon as possible and lack of knowledge emerge as environment limit to sexuality.
b. "Unconsummated marriage" where time to consultation is longer (6 months or more) and sexual difficulty is male, female or both shared. Here pressure to consummate as soon as possible is not a main issue and lack of knowledge emerge as individual avoidance of the issue during life.
A new terminology
Instead of UM, the term "Unconsummated Relationship" could be useful to describe all over the world a relation were sexual intercourse never succeeded after a 6 months period of attempts and where a social pressure is not relevant and privacy is guaranteed. In cultural systems where marriage is mandatory to have sex, it is obvious that "relationship" means "marriage". "First attempts dysfunction" could be a useful term to describe the impossibility to perform an intercourse because of social-cultural pressure to have an erection and then an intercourse as soon as possible, with the aim to be "integrated" in the society. In cultural systems where marriage is mandatory to have sex, it is obvious that "first attempts" means "honeymoon" and "bride defloration". Other conditions should be diagnosed as individual sexual dysfunction with current parameters. This could help scientific community to understand how our different clinical data refer to similar realities.
References
- Abraham G, Pasini W (1974) Introduction a la Sexologie Medicale. Payol, France.
- Usta MF, Erdoğru T, Tefekli A, Köksal T, Yücel B, et al. (2001) Honeymoon impotence: psychogenic or organic in origin? Urology 57(4): 758-762.
- Shamloul R (2006) Management of honeymoon impotence. J Sex Med 3(2): 361-366.
- Waynberg J (1994) Guide pratique de sexologie medicale. Paris: SIMEP, France, pp. 93-99.
- Promodu K, Shanmughadas KV, Bhat S, Nair KR (2007) Penile length and circumference: An Indian study. Int J Impot Res 19(6): 558-563.
- Farnam F, Janghorbani M, Raisi F, and Merghati-Khoie E (2014) Compare the effectiveness of PLISSIT and Sexual Health Models on women’s sexual problems in Tehran, Iran: A randomized controlled trial. J Sex Med 11(11): 2679-2689.
- Zargooshi J (2008) Male sexual dysfunction in unconsummated marriage: long-term outcome in 417 patients. J Sex Med 5(12): 28952903.
- Fageeh WM (2011) Different treatment modalities for refractory vaginismus in Western Saudi Arabia. J Sex Med 8(6): 1735-1739.
- Badran W, Moamen N, Fahmy I, El-Karaksy A, Abdel-Nasser TM, et al. (2006) Etiological factors of unconsummated marriage. Int J Impot Res 18(5): 458-463.
- Ghanem H, El-Dakhly M, Shamloul R (2008) Alternate-day tadalafil in the management of honeymoon impotence. J Sex Med 5(6): 1451-1454.
- Zahran AR, Abdeldaeim HM, Fouda K, Elgebaly OF(2012) Congenital penile curvature presenting as unconsummated marriage. Repair by 16-dot plication with subjectively reported patient and partner satisfaction. Arab J Urol 10(4): 429-433.
- Ozdemir O, Simsek F, Ozkardes S, Incesu C, Karakoc B (2008) The Uncosummated marriage: its frequency and clinical characteristics in a sexual dysfunction clinic. J Sex Marital Ther 34(3): 268-279.
- He Q, Yang JR, Liu LF (2009) Efficacy of sildenafil on erectile dysfunction of newly-weds. Andrologia 41(6): 348-351.
- Malik MA, Iqbal Z, Ashraf N, Javed SH, Ahmed I (2009) Phosphodiesterase Inhibitor (Sildena-fil) in the Management of Honey Moon Impotence. Int J Nephrol Urol 1(2): 103-107.
- Lauman EO, Paik A, Rosen C (1999) Sexual dysfunction in the United States. Prevalence and predictors. JAMA 281(6): 537-544.
- Ghatrifi D, Ghatrifi R (2013) Based on experiences of students, social factors are one of the most important reasons of pre marriage sexual activity in Iran. Proceedings from the 21st Congress of the World Association for Sexual Health 339. Journal of Sexual Medicine 10(suppl 5): 277-422.
- Michetti PM, Silvaggi M, Fabrizi A, Tartaglia N, Rossi R, et al. (2014) Unconsummated marriage: can it still be considered a consequence of vaginismus? Int J Impot Res 26(1): 28-30.
- Ribner DS, Rosenbaum TY (2005) Evaluation and Treatment of Unconsummated Marriages among Orthodox Jewish Couples. J Sex Marital Ther 31(4): 341-353.
- Lema VM (2014) Unconsummated marriage in sub-Saharan Africa: case reports. Afr J Reprod Health 18(3): 159-65.
- Kaplan HS (1974) The New Sex Therapy. Brunner/Mazel, USA.
- Crowe M, Jones M (1992) Sex therapy: the successes, the failure, the future. Br J Hosp Med 48(8): 474-479.
- Binik YM (2010) The DSM diagnostic criteria for vaginismus. Arch Sex Behav 39(2): 278-291.
- Fisher WA, Eardley I, McCabe M, Sand M (2009) Erectile dysfunction (ED) is a shared sexual concern of couples II: association of female partner characteristics with male partner ED treatment seeking and phosphodiesterase type 5 inhibitor utilizations. J Sex Med 6(11): 31113124.
- Conaglen JV, Conaglen HM (2009) The effects of treating male hypogonadism on couples' sexual desire and function. J Sex Med 6(2): 456-463.
- Gindin LR, Resnicoff D (2002) Unconsummated Marriages: A Separate and Different Clinical Entity. J Sex Marital Ther 28(Suppl 1): 85-99.
- Kaplan HL, Sadock BJ (1995) Normal human sexuality and sexual and gender identity disorders. In: Kaplan HL, Sadock BJ (Eds.), Normal human sexuality and sexual and gender identity disorders.
- Bramley HM, Brown J, Draper KC, Kilvington J (1983) Non-consummation of marriage treated by members of the Institute of Psychosocial Medicine: a prospective study. Br J Obstet Gynaecol 90(10): 908-913.
- Duddle M (1977) Etiological factors in the unconsummated marriage. J Psychosom Res 21(2): 157-160.
- Addar MH (2004) The unconsummated marriage: Causes and management. Clin Exp Obstet Gynecol 31(4): 279-281.
- Ellison C (1968) Psychosomatic factors in the unconsummated marriage. J Psychosom Res 12(1): 61-65.
- Lomax-Simpson JM (1960) Unconsummated marriage in women. Medical World 221-224.
- 32. Nabil Mhiri M, Smaoui W, Bouassida M, Chabchoub K, Masmoudi J, et al.(2013)Unconsummated marriage in the Arab Islamic world: Tunisian experience. Sexologie 22(3): e71-e76.
- Sungur MZ, Günduz AA (2014) Comparison of DSM-IV-TR and DSM-5 definitions for sexual dysfunctions: critiques and challenges. J Sex Med 11(2): 364-373.
- Shalev O, Baum N, Itzhaki H (2013) "There's a Man in My Bed”: The First Experience of Sex Among Modern-Orthodox Newlyweds in Israel. J Sex Marital Ther 39(1): 40-55.
- Zargooshi J (2000) Unconsummated marriage: clarification of aetiology;treatment with intracorporeal injection. BJU Int 86(1): 75-79.
- Leary MR (2001) Social anxiety as an early warning system: A refinement and extension of the self-presentational theory of social anxiety. In: Hofman SG, DiBartolo PM (Eds.), From social anxiety to social phobia: Multiple perspectives. Allyn & Bacon, USA, pp. 321-334.
- Meleshko KGA, Alden LE (1993) Anxiety and self-disclosure: Toward a motivational model. J Pers Soc Psychol 64(6): 1000-1009.
- Sparrevohn RM, Rapee RM (2009) Self-disclosure, emotional expression and intimacy within romantic relationships of people with social phobia. Behav Res Ther 47(12): 1074-1078.
- Kashdan TB, Volkmann JR, Breen WE, Han S (2007) Social anxiety and romantic relationships: The costs and benefits of negative emotion expression are context-dependent. J Anxiety Disord 21(4): 475-492.
- Keltner D, Haidt J (1999) Social functions of emotions at multiple levels of analysis. Cognition & Emotion 13(5): 505-522.
- 41. Keltner D, Kring AM (1998) Emotion, social function, and psychopathology. Review of General Psychology 2(3): 320-342.
- Davila J, Beck JG (2002) Is social anxiety associated with impairment in close relationships? A preliminary investigation. Behavior Therapy 33(3): 427-446.
- Bodinger L, Hermesh H, Aizenberg D, Valevski A, Marom S, et al. (2002) Sexual function and behavior in social phobia. J Clin Psychiatry 63(10): 874-879.
- Descutner CJ, Thelen MH (1991) Development and validation of a Fear- of-Intimacy Scale. Psychological Assessment 3: 218-225.
- Montesi JL, Conner BT, Gordon EA, Fauber RL, Kim KH, et al. (2013) On the Relationship Among Social Anxiety, Intimacy, Sexual Communication, and Sexual Satisfaction in Young Couples. Arch Sex Behav 42(1): 81-91.
- Hope DA, Heimberg RG, Turk CL (2010) Managing social anxiety: A cognitive-behavioral therapy approach (2nd edn), Oxford University Press, USA.
- Sadock VA (1999) Normal human sexuality and sexual and gender identity disorders. In: Sadock BJ, Sadock VA (Eds.), Comprehensive textbook of psychiatry (7th edn), Lippincott Williams & Wilkins, USA, pp. 1600-1601.
- El-Meliegy A (2004) A retrospective study of 418 patients with honeymoon impotence in an andrology clinic in Jeddah, Saudi Arabia. Europ J Sexol 13: 1-4.
- Cherner RA, Reissing ED (2013) A Comparative Study of Sexual Function, Behavior, and Cognitions of Women with Lifelong Vaginismus. Arch Sex Behav 42(8): 1605-1614.
- Perelman MA (2003) Sex coaching for physicians: combination treatment for patient and partner. Int J Impot Res 15: S67-S74.
- Blazer JA (1964) Married virgins-Studies of unconsummated marriages. Journal of Marriage Family 26: 213-214.
- David SR, Rosenbaum TY (2005) Evaluation and Treatment of Unconsummated Marriages among Orthodox Jewish Couples. Journal of Sex & Marital Therapy 31(4): 341-353.
- Williams, Wilkins (1995) Chapter 21: Comprehensive Textbook of Psychiatry (6th edn), Baltimore, Maryland, Vol 2, pp. 1295-1360.
© 2017 Silvaggi M, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






