- Submissions

Full Text
Psychology and Psychotherapy: Research Studys
Changes in Adaptive-Compensatory Functions in Patients with Paranoid Schizophrenia with an Affective Pattern of Non-Suicidal Auto- Aggressive Behavior in Conditions of Prolonged Social Isolation
Kravchenko IV1*, Sevrykov VT2 And Bezmenova NO3
1Department of Rehabilitation Treatment, Candidate of Medical Sciences, Clinical Pharmacologist, Psychiatrist-Psychotherapist of the Interdistrict, Russia
2Department of Forensic Medicine, Candidate of Medical Sciences, North-Western State Medical University, Russia
3Department of Dentist, Forensic Expert, Russia
*Corresponding author: Kravchenko IV, Department of Rehabilitation Treatment, Candidate of Medical Sciences, clinical pharmacologist, psychiatristpsychotherapist of the interdistrict, Russia
Submission: April 03, 2023Published: April 24, 2023

ISSN 2639-0612Volume6 Issue5
Abstract
A total of 232 patients with paranoid schizophrenia who were in conditions of long-term social isolation (prison, forced treatment) were studied. A relationship has been established between non-suicidal selfharm and leading psychopathological changes within the framework of the underlying disease in such patients. It was found that at the beginning of the development of a procedural disease, non-suicidal auto-aggression is episodic, arising impulsively, at the height of psycho-emotional experiences. In the future, non-suicidal auto-aggression acquires the character of conscious actions within the framework of a pseudo-adaptive coping strategy, the consolidation of which in the form of a dominant behavior model is prevented by increasing procedural changes in the personality.
keywordsNon-suicidal auto-aggressive actions; Coping strategy; Paranoid schizophrenia; Long-term social isolation
Introduction
Disorders of adaptive-compensatory functions in patients with paranoid schizophrenia are an integral part of a single pathopsychological process [1-5]. The depletion of personality reserves intensifies when being in conditions of prolonged social isolation, including the penitentiary system and compulsory treatment [6,7]. In this case, the number of selfdestructive forms of response increases, including the formation of non-suicidal autoaggressive behavior, or “NSAB” for short [8-16]. Its imprint on the formation of sustainable auto-aggressive behavior leaves a wide spread in places of deprivation of liberty of the socalled criminal hierarchy of values, with approval relating to the commission of non-suicidal auto-aggressive actions or abbreviated as “NSAA”. Most often, their implementation is in the nature of a protest against existing regime restrictions, and also reflects the desire to prescribe additional diagnostic procedures. To mitigate distress, patients with paranoid schizophrenia are forced to resort to the development of new forms of adaptive behavior (coping strategies). The result of such actions are changes in the cognitive, emotional and behavioral spheres in such patients [17-21]. Knowledge of the regularities in the change of adaptive functions can contribute to the improvement of therapeutic and rehabilitation measures in this group of patients.
Purpose of the study
To study the role of NSAB in relation to the leading
psychopathological changes in patients with paranoid schizophrenia
with an organoid defect in conditions of long-term social isolation.
Research method. By means of a retrospective analysis of available
medical records, 232 patients with paranoid schizophrenia who
were in conditions of long-term social isolation (prison detention,
compulsory treatment) were studied. All subjects were men aged 20
to 55 years. The average age of the subjects was 36.1±1.2 years. The
average duration of a procedural disease was 16.4±2.1 years. Type
of course of the schizophrenic process: paroxysmal-progressive. All
subjects were on antipsychotic therapy. The inclusion criteria were:
A. Compliance of the diagnosis of paranoid schizophrenia with
the criteria of the ICD-10 revision (F20.0).
B. The presence of NSAA in history, realized outside the psychotic
period.
C. Adherence to the criminal subculture declared by the subjects
themselves (the so-called “criminal attitude behavior”,
“criminal hierarchy of values”).
The clinical picture of the subjects was determined by negative procedural personality changes with severe behavioral disorders. Under the definition of “NSAA” fell a variety of actions directed against one’s health and accompanied by a violation of the integrity (functions) of organs or organ systems. However, there was no demonstration of intent to commit suicide. The concept of “criminal attitude behavior” was associated with “the steady anti-social orientation of the individual with the desire to use criminal slang, building relationships with others from the positions of the criminal hierarchy of values, flaunting the criminal past, applying specific tattoos.” The term “criminal hierarchy of values” was understood as a certain “set of rules of conduct, bearing an indisputable character (dogma), for persons identifying themselves with the criminal environment”. The first NSAAs examined were applied to themselves at the age of 14 years. Such actions were defiantly blackmailing in nature, and also served as a tool for relieving psycho-emotional stress. Such self-harm was limited to superficial cuts in the area of the shoulder, forearm, inner thigh. A retrospective analysis made it possible to attribute such actions to the prodromal period of the schizophrenic process, when the manifestation of the disease was determined by nonspecific behavioral disorders. The next stage in the implementation of self-damaging behavior was the placement of the subjects in a judicial situation, after they had committed offenses. Being at the stage of undergoing a forensic psychiatric examination, the subjects closely communicated with persons who had previously been repeatedly in places of deprivation of liberty, adopting their practical experience in the field of causing nonsuicidal self-harm.
As a result, NSAAs were distinguished by a high degree of diversity, often having a combined character: sewing up the mouth with a thread; Biting the tongue of the lips; Introduction of air into the gums; Introduction of foreign bodies into the gum cavity; Rubbing gums with local irritating agents; Chemical burns of the oral cavity and so on. Most often, their implementation was in the nature of a protest against existing regime restrictions, and also reflected the desire to avoid criminal liability. Non-suicidal selfharm was realized within the framework of the NSAB affective pattern. In this case, the NSAA wore a form of emotional release, in the here and now. There was no preparatory period, the postmorbid period was accompanied by formal criticism of what had been done. At the same time, the clinical picture of the subjects was determined by negative procedural changes in the personality in the form of an increase in aggressive tendencies, emotional coarsening, structural disorders of thinking, loss of criticism of one’s behavior. The assessment of the mental state of the examination was carried out by clinical and experimental psychological methods at the time of inclusion in the study (1 week), then at 12 and 24 weeks of the study. As an experimental psychological method, the test of Heim E. (E. Heim), adapted in the laboratory of clinical psychology of the Psychoneurological Institute Bekhterev VM [22].
Research results
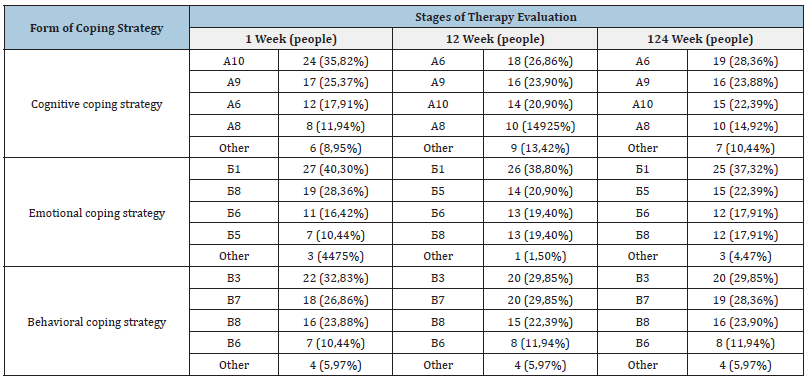
The dynamics of the development of the coping strategy in the form of NSAB in the examined individuals was associated with procedural personality changes according to the “organoid” or “pseudo-organic” type. This term is rather arbitrary, since the procedural changes detected by the clinical method were combined with truly organic changes in the neuropsychic sphere. At the clinical level, there were changes in the emotional-volitional sphere in combination with impulsivity, dysphoria, thoroughness of thinking, suspicion, and getting stuck on negative events of the past. At later stages, there were manifestations of dysmnesia, oligophasia, aprosexia of varying severity. The study of the actual dynamics of the transformation of coping strategies in the examined individuals showed the following. It has been established that the cognitive coping strategy in the form of “setting one’s own value” that dominated at the beginning among the subjects was replaced by a coping strategy in the form of “relativity”, remaining further as the leading cognitive model of coping throughout the study. The second most important cognitive coping strategy was in the form of “giving meaning”, remaining unchanged throughout the study. The leading emotional coping strategy in the subjects throughout the study remained the protest behavior model (for the majority of the subjects), as well as “submission” (for a smaller number of subjects). At the same time, the model built on openly manifested aggression underwent a change, which then transformed into the so-called “passive cooperation”. Finally, the basis of behavioral coping strategies throughout the study was formed by “active avoidance”, noted in most patients. Less common, but also remained in the same form, coping models in the form of “active avoidance”, “cooperation”, “conversion” (Table 1).
Table 1:Comparative analysis of the leading coping strategies in the examined patients.
Discussion
In the course of dynamic analysis, it was found that the basic cognitive coping strategy in most of the examined patients was the so-called “setting one’s own value”. This was reflected in an increased level of egocentrism, intolerance towards the opinions of others, the desire for authoritarian dominance in the reference group. The ongoing therapy and the growing procedural emotionalvolitional disturbances smoothed out these psychopathological manifestations, which led to an increase in the proportion of cognitive coping strategies aimed at cooperating with others, taking into account the real state of affairs, and restraining openly non-suicidal auto-aggression (coping strategies in the form of “relativity”, “giving meaning”). Among emotional coping strategies, those associated with the protest style of response against the background of dysphoric manifestations (coping strategy in the form of “aggression”, “protest”) remained dominant throughout the treatment. Subsequently, patients were forced to resort to less energy-intensive forms of protest, which led to an increase in the proportion of such emotional coping strategies as “passive cooperation”, “retreat”. The same negative (deficient) personality changes contributed to the initial formation and further consolidation of the following behavioral coping strategies: “active avoidance”, “cooperation”, “conversion”). As an illustration, we present the following clinical observation. Patient S., born in 1987 entered the St. Petersburg Specialized Psychiatric Hospital with intensive follow-up in 2022. Diagnosis: paranoid schizophrenia, episodic type of course, with a progressive defect. Heredity is burdened by the alcoholism of parents.
The second child in the family. Pregnancy, childbirth with complications in the form of cord entanglement, asphyxia. There was a delay in the development of motor skills. From an early age he was excitable, noisy, could “shout for hours”. He suffered from bedwetting until the age of 6. In kindergarten, he was easily excitable, easily got into a fight with other guys, was expelled from him for his behavior. I went to school at the age of 7, showed no interest in learning. From 7 to 10 years old I went to the boxing section. Regularly clashed with teachers, classmates and parents. He easily got into fights, while losing control of himself, “fought until they pulled him away.” He was observed by an adolescent neurologist with a diagnosis of “consequences of residual-organic lesions of the central nervous system”, did not receive drug therapy. He graduated from 9 classes, then a technical college. At the age of 14 he became addicted to alcohol and marijuana. Several times he was prosecuted for complicity in thefts, received a suspended sentence. He suffered two traumatic brain injuries received during provoked conflicts. He was released from military service due to neurological pathology. At the age of 24, he was sentenced to 6.5 years for drug dealing. In places of deprivation of liberty, from the first days he actively clashed with the administration, oppressed weaker convicts. Enjoyed authority to persons with criminal installation behavior. Repeatedly placed in a punishment cell for disobedience to regime requirements.
Repeatedly inflicted superficial self-harm of a piercing-cutting nature, swallowed foreign bodies in protest. Also, in protest, he tried to refuse to eat, sewed up his mouth with a coarse thread. In conflicts with other prisoners, he received two craniocerebral injuries. At a certain point in time, he began to complain of anxiety, depression, unwillingness to live. He claimed that he “hears a female voice that threatens to rape him.” He was examined by a local psychiatrist and sent for a forensic psychiatric examination, at which he was passive at first, suspended. With the relief of acute psychopathological symptoms, he began to reveal features of emotional instability, explosiveness, and conflict. He oppressed weaker patients, refused to comply with the requirements of medical personnel. He was discharged with a diagnosis: “Schizophrenia-like disorder on organically defective soil.” Returned to prison. Soon he again began to complain of poor sleep, low mood, tried to commit suicide. He was again sent for a forensic psychiatric examination, according to the results of which he was declared insane as suffering from paranoid schizophrenia, an episodic type of course with a growing defect. Sent to compulsory treatment with release from criminal liability. Upon admission to the hospital. Somatic status - no significant pathology; Neurological status - no significant pathology. Laboratory data: clinical blood tests, urine in dynamics without pathology. mental status consciousness is clear, oriented in place, time, own personality is correct. Contact is available. The voice is quiet, the speech is weakly modulated. Most of the time he answered questions in monosyllables. In a conversation, he is passive, lacking initiative, emotionally coarse. In statements, he is secretive, carefully selects words and expressions.
At the department, he immediately emphasized his adherence to “criminal concepts”, but he avoided the role of a criminal leader. He was distinguished by explosiveness, conflict in relation to everyday difficulties. Repeatedly demanded that the administration ease the regime requirements. He reacted impulsively to the refusal, at the height of the affectively narrowed consciousness he repeatedly inflicted superficial self-cuts in the area of the forearms. Then he complained of persistent headaches, nausea, weakness. In dynamics, impulsiveness, dysphoria, thoroughness of thinking, suspicion, and obsession with negative events of the past increased. There were atactic closures, sperrings. At later stages, there were manifestations of dysmnesia, oligophasia, aprosexia of varying severity. Under the influence of therapy and increasing cognitive impairment, the activity of protest actions was replaced by verbal threats, irritable weakness. Detected passivity in relation to the spread of the criminal hierarchy of values, but still emphasized his commitment to it. Grouped with other patients solely to resolve domestic issues, avoided participation in rehabilitation activities. There was no criticism of his condition, the committed socially dangerous act.
Conclusion
Non-suicidal auto aggression in patients with paranoid schizophrenia with an affective pattern of NSAB was inextricably linked with leading psychopathological changes within the underlying disease. At the beginning of the development of a procedural disease, non-suicidal auto-aggression is episodic, impulsive, reflecting the individual’s protest moods according to the “here and now” principle. In the future, NSAA acquires the character of conscious, planned actions that bring secondary benefits to the subjects. In fact, the NSAA formed a pseudo-adaptive coping strategy. However, the growth of procedural negative personality changes contributes to a decrease in the ability to purposeful volitional actions, which led to a decrease in the effectiveness of the implementation of this pseudo-adaptive coping strategy. Knowledge of the revealed regularities in the development of adaptive-compensatory mechanisms in patients with paranoid schizophrenia with an affective pattern of NSAB can help increase the effectiveness of therapeutic and preventive measures in this group of people.
References
- Andriopoulos I, Ellul J, Skokou M, Beratis S (2011) Suicidality in the "prodromal" phase of schizophrenia. Compr Psychiatry 52(5): 479-485.
- Edmondson AJ, Brennan CA, House AO (2016) Non-suicidal reasons for self-harm: A systematic review of self-reported accounts. J Affect Disord 191: 109-117.
- Taylor PJ, Jomar K, Dhingra K, Forrester R, Shahmalak U, et al. (2018) A meta-analysis of the prevalence of different functions of non-suicidal self-injury. J Affect Disord 227:759-769.
- Yin Y, Tong J, Huang J, Tian B, Chen S, et al. (2020) Suicidal ideation, suicide attempts, and neurocognitive dysfunctions among patients with first-episode schizophrenia. Suicide Life Threat Behav 50(6): 1181-1188.
- Álvarez MJ, Masramom H, Foguet-Boreu Q, Tasa-Vinyals E, García-Eslava JS, et al. (2021) Childhood trauma in schizophrenia spectrum disorders: Dissociative, psychotic symptoms and suicide behavior. J Nerv Ment Dis 209(1): 40-48.
- Lau S, Gunther MP, Kling S, Kirchebner J (2019) Latent class analysis identified phenotypes in individuals with schizophrenia spectrum disorder who engage in aggressive behaviour towards others. European Psychiatry 60: 86-96.
- Kirchebner J, Sonnweber M, Nater UM, Gunther M, Lau S, et al. (2022) Stress, schizophrenia and violence: A machine learning approach. Journal of Interpersonal Violence 37(1-2): 602-622.
- Mork E, Mehlum L, Barrett EA, Agartz I, Friedman JMH, et al. (2012) Self-harm in patients with schizophrenia spectrum disorders. Archives of Suicide Research 16(2): 111-123.
- Pluck G, Lekka NP, Sarkar S, Lee KH, Bath PA, et al. (2013) Clinical and neuropsychological aspects of non-fatal self-harm in schizophrenia. Eur Psychiatry 28(6): 344-348.
- Fazel S, Wolf A, Palm C, Lichtenstein P (2014) Violent crime, suicide, and premature mortality in patients with schizophrenia and related disorders: A 38-year total population study in Sweden. Lancet Psychiatry 1(1): 44-54.
- Domínguez-Baleón C, Gutiérrez-Mondragón LF, Campos-González AI, Rentería ME (2018) Neuroimaging studies of suicidal behavior and non-suicidal self-injury in psychiatric patients: A systematic review. Front Psychiatry 16(9): 500.
- Penney S, Prosser A, Simpson AIF (2018) Age onset of offending and serious mental illness among forensic psychiatric patients: A latent profile analysis. Criminal Behaviour and Mental Health 28(4): 335-349.
- Güney E, Alnıak İ, Erkıran M (2020) Predicting factors for non-suicidal self-injury in patients with schizophrenia spectrum disorders and the role of substance use. Asian J Psychiatr 52: 102068.
- Smith HP, Power J, Usher AM, Sitren AH, Slade K (2019) Working with prisoners who self‐harm: A qualitative study on stress, denial of weakness, and encouraging resilience in a sample of correctional staff. Criminal Behaviour and Mental Health 29(1): 7-17.
- René KJ, Huber DA, Kirchebner J, Sonnweber M, Gunther MP, et al. (2021) Self-harm among forensic psychiatric inpatients with schizophrenia spectrum disorders: an explorative analysis. International Journal of Offender Therapy and Comparative Criminology 67(4): 352-372.
- Rudnick A, Martins J (2009) Coping and schizophrenia: A re-analysis. Arch Psychiatr Nurs 23(1): 11-15.
- Prasko J, Holubova M, Hruby R, Latalova K, Kamaradova D, et al. (2016) Coping strategies and self-stigma in patients with schizophrenia-spectrum disorders. Patient Preference and Adherence 10: 1151-1158.
- Shah R, Grover S, Kulhara P (2017) Coping in residual schizophrenia: Re-analysis of ways of Coping checklist. Indian J Med Res 145(6): 786-795.
- Aguileta RLI, Badia RV, Usall J, Butjosa A, Ochoa S (2020) Coping strategies in first-episode psychosis: A systematic review. Early Interv Psychiatry 14(3): 252-262.
- Piotrowski P, Rymaszewska J, Stańczykiewicz B, Małecka M, Kotowicz K, et al. (2020) Stress coping strategies and their clinical correlates in patients with psychosis at various stages of illness: A case-control study. Early Interv Psychiatry 14(5): 559-567.
- Holubova M, Prasko J, Hruby R, Latalova K, Kamaradova D, et al. (2016) Coping strategies and self-stigma in patients with schizophrenia-spectrum disorders. Patient Prefer Adherence 10: 1151-1158.
- Neznanov NG, Ivanov MV (2021) Negative and cognitive disorders in endogenous psychoses: Diagnostics, clinic, therapy, MED Press-Inform Publishers, Moscow, Russia, p. 320.
© 2023 Kravchenko IV, This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






