- Submissions

Full Text
Psychology and Psychotherapy: Research Studys
Side Effects-What do we Actually know about them?
Maija Kozlovska1*, Liga Kozlovska1,2, Vija Silina1,2, Sandra Puce3, Ruta Vintere1 and Gunta Ticmane1,2
1The Rural Family Doctors’ Association of Latvia, Latvia
1The Riga Stradins University, Latvia
1Latvian Psychiatric Association, Latvia
*Corresponding author: Maija Kozlovska, The Rural Family Doctors’ Association of Latvia, Latvia
Submission: March 06, 2023Published: March 27, 2023

ISSN 2639-0612Volume6 Issue4
Abstract
In a world, there are many diseases, which spread faster, than we can imagine. By coughing just once- 20,000 viruses are spread-some of which rocket out at speeds greater than 322km per hour and might last in the air for hours [1]. Over 95% of the world’s inhabitants have health issues, with over a third having more than five disorders [2]. It is not always enough to have natural healing to get well. The help usually is treatment with pills, which are supposed to help, and cure the patient in the very best cases. However, what do we know about consequences of such treatment? I, the doctor, who believes in evidence based medicine, daily face cases, that request to be questioned about. This is the case report of two patients, looked at through the prism of side effects and morbidity-the first case contain visual perception disturbances after the use of clarithromycin, the second- hair loss after the use of atorvastatin. And the third case, involving multidisciplinary approach to an epileptic seizures and truck driving
Case 1
In 2014, there was a transitional period for my patients and me. As I left my previous work as a resident and started a new family doctor’s practice in a new, bilingual town. Those who were left, blossomed in my memory, and those who came for the first time - doubtfully met me. I still had to earn their trust. At the very start, the practice was overloaded. Patients were in need for a doctor. One day, in 2015, a young, 16 year old girl, automatically registered at my practice in 2014, came to me, complaining about cough, sore throat, and elevated body temperature [axial temperature was 38 Celsius high for 5 days] and a chest pain while coughing. Auscultation showed crepitation in both lungs. The diagnosis was clear-pneumonia. The patient recently had taken the course of amoxicillin and therefore a clarithromycin [Placid] was prescribed for the girl-250mg tablet twice a day for 7 days. The girl spoke Russian, but even through translational difficulties, she was open to contact, and while speaking to me, she looked in my eyes. So, there were no doubts, that she understood my recommendations and me. After consultation, she said farewell and left.
Two days later, she reappeared in the morning and looked very scared-the patient ran into my cabinet with words “Doctor, I am not going to take these pills anymore-I had hallucinations from them!” I asked the girl to describe how it was and what she saw or hear or felt. The description was bright-the room changed, monsters in various colours showed up, strange sounds were disturbing and a feeling of dizziness troubled the girl after taking the medicine. I said, if she felt so bad after them, the girl must not continue the medicine, and that I must report about these side effects, and the therapy should be changed instead. Unfortunately, she was so frightened, that a teen told she feels better, and is not going to use anything for now and quickly shut the door and left. So, after unsuccessful trying to contact the teen and her parents, I reported about the possible side effects. In 2018, November, the picture was not so good-a patient, aged 21, reappeared. She stated to have schizotypal disorder and showed the papers of acute hospitalization in psychiatric assistance service on May 11, 2017.
The girl did not use the prescribed medicines for her mental disorder, as they made her special intuition and dreams disappear, and this seemed weird to her. Her face was hypo-mimic, during the consultation the patient looked down to the floor or aside, expressed to feel the guilt of being the burden for her parents, but due to the defect of will power, the young woman could do nothing about the situation. She said to have no mood at all, ever, complained about feeling paranoid, agoraphobic, and claustrophobic; she could not even call on the phone to the doctor, as she feared to call and had panic attacks then. The patient had anxiety, anger with affectlike conditions and behavioural changes and had psychopathic and sociopathic features. The young woman had had problems with anger control-once a little kitty made a scratch on her arm and she almost choked the kitty to death. She said that it was not the only case when the youngster could not help but physically abuse animals. The patient had not had the sexual experience yet, still she had paranoid delusions about that all men wanted to rape her. The young woman all her life was passive smoker, and lived with her father and grandmother, had >5 times bronchitis, and once pneumonia and allergic rhinitis, visited doctor rare only when in need due to infection. Her mother breastfed her till 3 months of age, and left for Germany for good, when the girl was very little (Table 1).
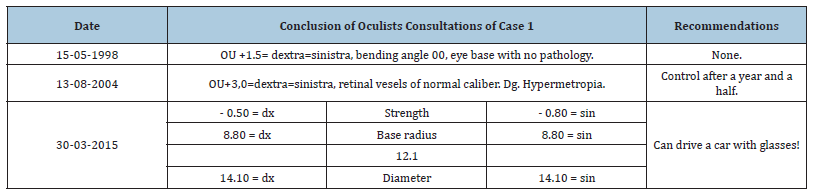
Table 1:Oculists chek-ups do not show large eye-pathologies except hypermetropia for Case1. However, in the last check up it can be seen, a specialist, being unaware of her mental state, allows a girl to drive a car.
Case 2
There are many jokes, involving patient’s excretory fluids, and how people take them to a doctor’s office. However, a doctor always must stay objective and see the scene as clear as possible. Once- 6 years ago-a 65 year old woman came to my office and took a 0,7 l large package full of hair out of her bag and when she took her cap off-I knew it was hers. The patient told she had a hair loss after the use of 40mg atorvastatin. When my surprise was gone, we got to know, that, indeed, she was one of 1,00,000 people, who had a hair loss after the use of this medicine. The use of atorvastatin was stopped immediately and after the few months, her hair had grown back.
Case 3
The Young Doctor in family medicine residency meets a young Male in consultation room. The patient presents himself as a healthy person and opens up about the necessity to gain the driver’s licence for driving with large trucks. The patient has not been very long to a doctor, so there is very little information in medical records about the young truck driver. Subjective information does not show any disturbances, and objective examination data also appear to be normal. The patient is asked to show arms, skin is light and with no signs of suicidality. The patient is asked to take some blood count, and he agrees to be examined. During the analyses, all of a sudden, the young patient [22yrs old] loses his consciousness and has epilepsy seizures. After medical help with diazepamum 5mg per so, the family doctor resident, explains, he cannot provide the patient with driver’s license and the patient needs to go to see neurologist. The person gets angry and starts to quarrel that he needs it now and otherwise he will go to other specialist who will provide him with the driver licence. This was really hard to manage the case, as the person, left the young general practitioner-unregistered due to drivers’ licence, and as there were no e-health then, he showed up and told that found a doctor, who provided him with the document he needed, unluckily for traffic participants. The patient yelled at family doctor, however, the clinical decision-making did not allow to bring the truck driver’s licence, as he yelled and left the cabinet. In the UK there was a case, when the doctor was shot with a weapon because in the E-Health there was written his diagnose of Epilepsy-there are a lot of unanswered questions about E-Health safety, doctor’s safety, patient’s safety and familial safety, and responsibility of all of them, and legislation.
Discussion
Science and clinical decision making sometimes may go separate ways. Two women with completely different stories-still both women had diseases and side effects. Case 2 was based on long term relationship, trust and compliance. Case 1 was met for the first time, received uncompleted consultation, and trust was yet to be deserved from both sides. So many questions arise from these 2 cases-we must believe our patients. Case 2 was a little bit shocking, but clear and obvious. She used the pills, noticed the problem and turned to the doctor completely relying on my competence. The patient believed it was okay to take her cap in front of me and show her hairless, also take her hair in the bag to the consultation as a proof. I knew her story for years and was doubtless. The case1, however, is not translucent and very complex. In 2004, the patient from case 1 used erythromycin; still no side effects were mentioned in her papers, even if the medicine was from the same group of antibiotics-why?
In 2014, during urinary tract infection, she said to have allergy from pills that contain cranberries only. The reaction is possible of course; however, did it actually happen? Alternatively, it might have been the exacerbations of schizotypal disorder or panic attack. Did she took her pills at all? Did she took the right ones? Why did not such questions arise when I consulted the Case 2? In November 2018, when asked about the perception disturbances after clarithromycin, she told, she remembered to have heard a woman and a man talking [different memory] and that symptoms of schizotypal disorder she had since 2010. As she remembered more auditory hallucinations it must be reconsidered, as this looks more like schizotypal disorder, or she did not remember precisely. It is known that schizophrenia and similar syndromes primarily has auditory and olfactory sensory misperception. Also visual hallucinations are common as a side effect. Neuro-ophthalmologist Bokkwan Jun, MD, PhD in Columbia, stated, that 1 of every 100 patients reports hallucinations that turn out to be related to medication. The decision making in case, when more than one disease is involved, gets complicated.
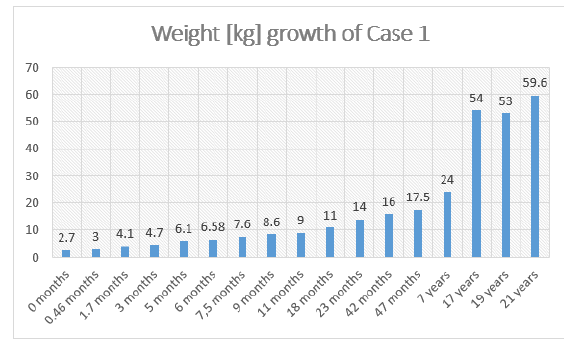
As I am no ophthalmologist, the data, if hallucinations were binocular or mono-ocular misses. However, it is known the girl had glasses and three check-ups from ophthalmologists, showing different confirmations (Figure 1). In 2004 there were data, that she might have vegetovasculardystonia due to feeling chest pain at young age [ECG was normal]. Otherwise the girl denied she had psychopathology or anything like that before. The girl was born with a small weight in natural labour [Apgar’s scale 7], however, she was breastfed only for 3 months and left by her mother in very early childhood- this also could play a role in the development of mental disease (Figure 2 & 3). On the other hand, who are we not to believe the patient? I trusted her and reported the issue, but what were the consequences? What if she had visual hallucinations after the medicine and schizotypal disorder exacerbation? If my report was true, it could help somebody. If it was not true- someday it might be a matter of life for some patient.
Figure 1: Doctors should be aware of hindsight bias-no matter how long they know the patient, what is his or hers health condition or what stigma circles around, as this bias can influence doctor’s decision-aking process and create “knew-it-all-along” effects..
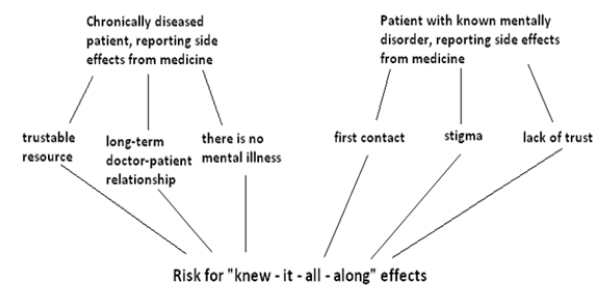
Figure 2:
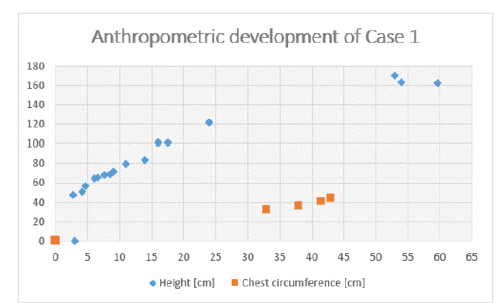
Figure 3: The small birth weight of Case 1 and lack of long term breastfeeding, also lack of mother in her life and long-lasting passive smoking by her father inside the room might promote the development of mental health due to hypoxia.
Conclusion and food for thoughts. Family doctors and doctors
of the world have a lot to consider
A. How many times do we actually report the side effects and
how we evaluate the picture? How strong it makes Evidence
based medicine? What happens to the use of medicine later in
the world?
B. Where does our responsibility start? When patient
presents with side effects, a special approach is needed and
guidelines are needed to be established and introduced.
C. Patients with acute diseases and those that are met for
the first time by doctor have to have longer consultations and
need more time and effort to evaluate and examine their actual
health condition.
D. Patients with chronic conditions are at risk to be seen
as predictable by a doctor, even though there has not been
evidence or it was little to predict it- a special approach is
needed to avoid knew-it-all-along effects [hindsight bias].
E. What happens to medical approach to a child in
transitional age or period? In 30-03-2015 the ophthalmologist
allowed a girl to drive a car for the first time with mental
disorder. The state needs more resources to provide everyone,
who wishes a driver’s license a psychiatric evaluation, even
if he or she is not seen by psychiatrist regularly or has not
been hospitalized in psychiatric assistance service. Obtaining
driver’s license must never be formal-epileptic seizures and
truck driving must be evaluated especially well, the same is
with psychiatric conditions. A family doctor must have access to
such information in case of providing driver’s license without a
psychiatrist [which is allowed in Latvia, if you know the patient
for 6 months and more].
F. Why is it harder to believe a patient with mental disorder/
neurological? Even being as objective as possible, the doctor
can be unaware of that, doctor and/or patient enters into the
stigmatization zone of mental disorder. The strongest biases
are those that are provided by experts, as experts believe in
them themselves [3,4].
G. Much more research is needed to look at the problem
from all angles more deeply, educate doctors, who report the
side effects of medicines, and leave patients safe and healthy.
References
- https://www.livescience.com/3686-gross-science-cough-sneeze.html
- Global Burden of Disease Study 2013 Collaborators (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: A systematic analysis for the Global Burden of Disease Study 2013. The Lancet 386(9995): 743-800.
- FitzGerald C, Hurst S (2017) Implicit bias in healthcare professionals: A systematic review. BMC Med Ethics 18(1): 19.
- Yaylaci S, Temiz T, Bestemir A, Genc AB, Demir MV (2015) Clarithromycin related visual hallucinations. Med J DY Patil Univ 8(4): 574.
© 2023 Maija Kozlovska, This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






