- Submissions

Full Text
Psychology and Psychotherapy: Research Studys
Iatrogenic Transmission of AIDS in Pakistan: A Review of the Situation
Samina Rafique1*, Mariyam Waseem1 and Ushna Ahmad2
1Bahauddin Zakariya University, Pakistan
2Nishtar Institute of Dentistry, Pakistan
*Corresponding author: Samina Rafique, Bahauddin Zakariya University, Pakistan
Submission: November 17, 2022Published: December 16, 2022

ISSN 2639-0612Volume6 Issue2
Abstract
Recently Pakistan has been identified as a country with a concentrated epidemic of HIV/AIDS. The latest report by UNAIDS has placed Pakistan on a list of 11 countries with the highest prevalence rates of HIV/ AIDS. Whereas in other countries, the incidence of HIV/ AIDS is decreasing, there has been a disturbing upsurge in the disease in Pakistan. The number of registered cases escalated from 3325 in March 2010 to a huge 49,584 by December 2021. Sexual mode of spread accounts for 45.10% of the cases, while transfusion of contaminated blood or blood components and unsafe injection practices have been identified as the main source of the outstanding, along with certain other factors. The recent outbreak of AIDS in a small district of Sindh province where 80% of the victims were kids has been linked to the transfusion of polluted blood. There is a paucity of healthy volunteer blood donations in the country and unfortunately, many injection drug users are found to be professional blood donors. Inadequacy of screening of the donated blood thus makes the environment favorable for the spread of HIV. Blood safety legislations exist but are not implemented properly. Moreover, the stigma associated with the disease prohibits the sufferers from accessing diagnostic services or disclosing their HIV status. Serious policy measures and strict implementation, along with community mobilization and involvement are required to control the spread of lethal infection and support patients living with HIV.
Keywords:AIDS; Unsafe injection; Unscreened blood transfusion; Iatrogenic transmission
Abbreviations:AIDS: Acquired Immune Deficiency Syndrome, ART: Anti-Retroviral Treatment, HIV: Human Immune Deficiency Virus, IDU: Injection Drug Users, FSW: Female Sex Worker, MSM: Men having Sex with Men, MSW: Male Sex Worker, MTC: Mother To Child, PLHIV: Patient Living with HIV, PPTCT: Prevention of Parent To Child Transmission, TGSW: Transgender Sex Worker
Introduction
Modern medicine, in spite of its progress, still struggles to combat HIV and AIDS effectively. According to the United Nations joint program on HIV/AIDS (UNAIDS), currently there is a gigantic number of 33.2 million adults and children living with HIV/AIDS. The highest number of patients is reported from sub-Saharan Africa. South Asia is second in the list. Injection drug users are the key population spreading infection among the general population through needle sharing and unprotected sex [1].
State of affairs in Pakistan
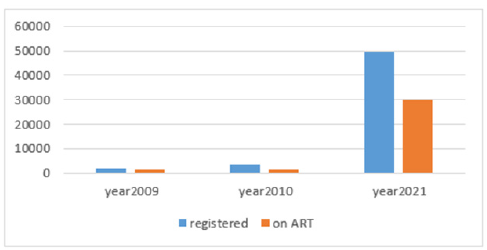
Previously Pakistan was identified as a high-risk, low prevalence country but by the mid-2000s there was a concentrated epidemic among key populations which is defined as the prevalence in traditional risk groups (injection drug users) exceeding 5% [2]. In 2009, UNAIDS Pakistan and NACP (national AIDS control program) assessed that there were around 98000 (79000-120000) HIV (Human Immune Deficiency Virus) cases in Pakistan, with an overall general population prevalence of less than 0·05 % [3]. Nevertheless, the epidemic is growing at an alarming speed and a decade later, in 2019, the total estimated number of PLHIV (Patients Living with HIV) escalated to 1,90000, with 1,30000 adult males, 53,000 females above 15, and 6100 children (0-14 years), with an overall prevalence of 0.2% in the adult population [4]. However, it is of urgent concern to note that this is not the summit yet; the latest estimation of PLHIV has heightened to a gigantic 0.24 million in 2021 [5]. This upsurge is plotted in Figure 1. The figure shows that the total number of registered HIVpositive cases by NACP reached 49584 by December 2021. Among the registered cases, 29626 (59·77%) are on ART (Antiretroviral treatment) in 51 ART centers all over the country. Out of these 7,056 (27.8%) are injection drug users. The reasons behind this disturbing upsurge are manyfold. Vastly prevalent poverty [6] low level of literacy [7] the rising number of drug addicts, low condom use rates [8,9] striking power imbalances in men and women [10] frequent and risky injection practices among IDUs (Injection drug users) [11] labor migration and lack of a robust surveillance system to check the HIV positive individuals [8] are the serious risk factors but careless transfusion of inadequately screened blood [12] and re-use of syringes or needles in formal and informal health care settings [13] are important elements that put the country in danger of facing a rapid spread of HIV.
Figure 1: Upsurge of AIDS cases in the last decade in Pakistan.
High-risk population
Like other Asian countries, IDUs epitomize the prime group driving the epidemic, along with TGSWs (Transgender Sex Workers), MSM (Men having Sex with Men), MSWs (Male Sex Workers), and FSWs (Female Sex Workers [8]. National surveillance statistics show the prevalence of AIDs among IDUs may vary from 15% to 50% in many cities including Faisalabad (52.5%), D.G. Khan (49.6%), Gujrat (46.2%), Karachi (42.2%) and Sargodha (40.6%), respectively [8].
Spill into general population
As in other countries, the disease is not confined to IDUs now but is spilling into the general public through the bridging populace [14]. In Pakistan, though HIV infection rates amid FSWs are not very high (at 2.2%), there is evidence of sexual interaction between FSWs and IDUs, and also between IDUs and other key populations (HSW, MSM, and MSW) [7,15-17]. Given the overlay between IDUs and at-risk sexual networks, the rising HIV prevalence among IDUs places commercial sex workers and their clients at an elevated risk level, along with spouses of IDUs (IBBS report 2016-17 revealed that 37.7% of IDUs were married). Similarly, a study about FSWS [18] revealed that 64.3% of them were married and 39.5 % of male sex workers showed bisexual behavior [2].
Therefore, in addition to key populations, bridging populations comprising spouses/intimate partners of IDUs, MSWs, FSWs, and MSM has become an ominous threat. The analogous linking populations have been identified in neighboring countries like China and India as well [19,20]. The situation becomes more grievous by the fact that condom use with non-paying sex partners is found to be very low. (4.1% and 10.9% in male and female sex workers respectively) The consistent use of condoms was slightly higher with paying sex partners. (38% and 8.6% in FSW and MSW respectively) [8]. Similarly low regular use of a condom (13.1%) was found in HSW [17]. All these factors make HIV transmission in Pakistan mostly heterosexual (52.5%) [2]. Research carried out by NGO Nai Zindgi in Punjab [21] discovered the occurrence of up to 15% of HIV in spouses and female partners of male IDUs. A national study [22] encompassing antenatal clinics in 2011 exhibited a prevalence of .05% among pregnant women.
Iatrogenic transmission (Blood transfusions aiding the enemy)
The situation of HIV in Pakistan is indeed complicated and precarious as the spectrum of the disease in the country comprises multiple modes of transmission (Figure 2). Heterosexual mode of spread accounts for 52.55% of the cases [3,23]. Among other sources of infection, iatrogenic transmission from unsafe healthcare practices, and poor infection prevention and control have been identified as major contributory factors [24]. Among these, transfusion of contaminated blood and blood products attain the most important position. Indeed the first reports of HIV in Pakistan in 1987 incriminate contaminated blood transfusions [25] which are now estimated to contribute 11.73% of the disease burden [26]. The studies have revealed that many of the IDUs act as paid blood donors [11,23] in a country with inadequate blood screening facilities. In a review of the blood safety system in Pakistan Zaheer et al. [27]. described that the blood transfusion service in Pakistan is not properly organized. Blood collection, screening, storing, and transfusions all are provided by blood banks that operate both in the public and private sectors. Numerous nonprofit blood donation organizations are also functioning to meet the demand of specific target groups such as thalassemia patients. All these providers lack coordination and there is no uniform standard of services, resulting in the suboptimal selection of donors and inadequate screening. Although blood safety legislation has been approved between 1997-2004 but are never implemented properly [28]. As a consequence, TTIs (Transfusion transmissible infections) including HIV remain an imminent threat to the recipients. According to WHO data of 2011 seroprevalence of HIV among blood donors was estimated to be 0.01% [29] while a study from Islamabad (Capital of Pakistan) estimated the prevalence of HIV up to 06% [30] among the donors. Ehsan H et al. [31] in a systematic review of studies conducted from 2010-2020 showed a paucity of healthy blood donation practices in Pakistani society along with an inadequate screening of high-risk donors. Still another study from Karachi [32] showed that only 55% of the blood banks could screen blood for HIV. An even worst situation can be expected in smaller towns and villages in this regard.
Figure 2: Diverse routes of spread of AIDS in Pakistan.
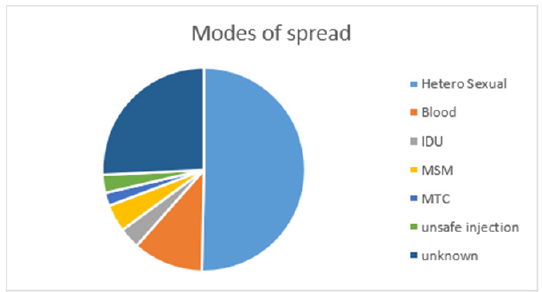
Another important contributing factor toward the prevalence of HIV/AIDS already described is unsafe injecting practices in formal and un-formal health care settings [13,24]. The illegal medical practice by unqualified and unauthorized persons (quacks) adds to the gravity of the situation. These quacks fill the gap in health care services and cater to a large portion of the population at a low cost, hence are accepted by the locals [33]. During an outbreak of AIDS in the Larkana district of Sindh province in April 2019, researchers discovered that 56.6% of the HIV-positive children reported receiving more than 10 injections in the past six months and 72.7% of HIV-positive kids had a transfusion in the same period [34]. In an article in Daily Times, Hina Javaid reported that two other outbreaks of HIV in Pakistan, (Gujrat, Punjab 2008 and Sargodha Punjab 2019) had an affirmative association with unsafe injection practices involving the re-use of syringes or needles and other surgical material [35]. From a recent survey in Pakistan, researchers estimated that 38% of surveyed physicians likely reused syringes [36]. All modes of transmission are graphically presented in Figure 2 which depicts that IDUs and MSM contribute 3.5%, and 4.5% of the cases respectively. Whereas mother-to-child transmission is responsible for 2.2% of the cases [23]. Male circumcision with unsterilized blades, nose, and ear piercing with dirty needles, and multiple uses of a single razor at barbers’ shops are some other factors contributing towards the spread of the disease [36]. Barber shops have been recognized as a potential threat to HIV spread in other countries as well [37,38]. All these factors are responsible for changing the geographic trend of the epidemic, which, unluckily, is expanding from major urban cities and provincial capitals to smaller cities and towns. Although national adult HIV prevalence in the general population remains under 0.1%, it may have been underestimated.
Stigma
The general public in Pakistan has not yet recognized or accepted the threat of HIV [39]. Being a conservative and religious society, there is stigma linked with HIV, as most people believe that diseased persons are involved in immoral activities such as extramarital sexual relationships, homosexuality, or intravenous (IV) drug use [40,41]. People try to avoid PLHIV for fear of contracting the disease. This is predominantly due to a lack of knowledge about the disease [42]. The fear of rejection by society stops people with risky behaviors from accessing HIV testing or revealing their HIVpositive status. A study conducted at workplaces across major cities of Pakistan revealed that 65% of the respondents were fired from their job and 29% were forced to resign after they disclosed their HIV-positive status [43]. Hence there is an imminent need of studying the psychosocial aspects of disease and disseminating knowledge about patterns of spread [44].
Response
Pakistan is struggling with the deadly disease despite its limited resources. NACP is working in collaboration with international funding agencies. 50 ART centers have been established all over the country in the public sector where free treatment is provided to PLHIV. 11 PPTCT centers have also been made in large cities but there are obstacles to finding the most effective approaches to reaching HIV-positive pregnant women, therefore the total number of registered mothers is low as compared to the national estimates. The UNAIDS (United Nations Program on HIV/AIDS) country progress report for Pakistan 2018 pointed out that since the decentralization of the Ministry of Health to the provinces in 2010, the HIV response has weakened because of poor coordination among different departments of health systems. The report also highlighted defects in reporting HIV cases and disparities in HIV interventions, possibly due to a lack of serious attitude by health officials. Moreover, lack of effective community engagement, challenges such as access to HIV services, social stigma and discrimination, lack of community and social support, and sexual and gender-based violence need urgent attention.
Conclusion and suggestions
A lot is being done at the government level to combat and
limit the explosion of HIV/AIDS but certain measures need to be
amplified such as
i. Increasing the testing of spouses of the male key
population to increase the uptake of pregnant mothers for
effective PPTCT.
ii. There should be a targeted district model approach with
a special focus on districts with high prevalence among the key
population.
iii. Strict rules and regulations about BTS in the country
iv. Strict monitoring of medical practice all over the country
especially in remote areas.
v. Awareness in the public about the mode of transmission
through print and electronic media.
vi. Advertisement of testing and ART centers.
vii. The Federal government support for the nonstop
provision of testing kits and ART.
The effective control of the problem demands engagement, participation, and awareness at the community level, amelioration of social stigma and discrimination, and provision of community and social support to PLHIV.
References
- Rodrigo C, Rajapakse S (2009) Current status of HIV/AIDS in south Asia. Journal of Global Infectious Diseases 1(2): 93-101.
- Country progress report UNAIDS (2014) The national AIDS control program. Ministry of National Health Services.
- (2022) UNGASS (United Nation General Assembly Special Session). Pakistan Report 2010.
- Pakistan country data (2020). HIV/AIDS Data Hub for Asia.
- National AIDS control program, Ministry of Health, Government of Pakistan, Pakistan.
- (2021) Multidimensional poverty in Pakistan. UNDP in Pakistan.
- https://www.statista.com/statistics/572781/
- (2021) 2nd Generation HIV/AIDS surveillance in Pakistan. IBBS Round V report 2016-17.
- Emmanuel F, Salim M, Akhtar N, Arshad S, Reza TE (2013) Second-generation surveillance for HIV/AIDS in Pakistan: Results from the 4th round of integrated behavior and biological survey 2011-2012. Sex Transom Infect 89(3): 23-28.
- Integration of Human Rights into HIV & AIDS.
- Shah SA, Altaf A, Mujeeb SA, Mujeeb SA, Memon (2004) An outbreak of HIV infection among injection drug users in a small town in Pakistan: Potential for national implications. Int J STD AIDS 15(3): 209.
- Khan AA, Khan A (2010) The HIV epidemic in Pakistan. J Pak Med Assoc 60(4): 300-307.
- Zakir ZM, Qureshi S, Zakir R, Rana S (2013) Unsafe injection practices and transmission risk of infectious diseases in Pakistan: Perspective and practices. Pakistan Vision 14(2): 27-51.
- (2008) Redesigning AIDS in Asia: Crafting an effective response. Report of the commission on AIDS in Asia, Oxford University Press, New Delhi, India.
- Reza T, Melesse DY, Shafer LA, Salim M, Altaf A, et al. (2013) Patterns and trends in Pakistan's heterogeneous HIV epidemic. Sexually Transmitted Infections 89(Suppl 2): 4-10.
- Haque N, Zafar T, Brahmbhatt H, Imam G, Ul Hassan S, et al. (2004) High-risk sexual behaviors among drug users in Pakistan: Implications for prevention of STDs and HIV/AIDS. International journal of STD & AIDS 15(9): 601-607.
- Khan AA, Rehan N, Qayyum K, Khan A (2008) Correlates and prevalence of HIV and sexually transmitted infections among Hijras (male transgenders) in Pakistan. International Journal of STD & AIDS 19(12): 817-820.
- (2007) Mapping networks of female sex workers in kothikanas and private homes, NACP, Canada‐Pakistan HIV/AIDS Surveillance Project.
- Choi KH, Gibson DR, Han L, Guo Y (2004) High levels of unprotected sex with men and women among men who have sex with men: A potential bridge of HIV transmission in Beijing, China. AIDS Education and Prevention 16(1): 19-30.
- Paranjape RS, Challacombe SJ (2016) HIV/AIDS in India: An overview of the Indian epidemic. Oral Diseases 22(1): 10-14.
- Nai Zindagi (2022) The hidden truth. PACP, Punjab, India.
- (2022) National AIDS control program antenatal sero-surveillance for HIV/AIDS in Pakistan 2012.
- Bhurgri Y (2006) HIV/AIDS in Pakistan. J Pak Med Ass 56(1): 1-2.
- Rabold EM, Ali H, Fernandez D, Knuth M, Schenkel K, et al. (2021) Systematic review of reported HIV outbreaks, Pakistan, 2000-2019. Emerging Infectious Diseases 27(4): 1039-1047.
- Khanani RM, Hafeez A, Rab SM, Rasheed S (1988) Human immunodeficiency virus-associated disorders in Pakistan. AIDS Research and Human Retroviruses 4(2): 149-154.
- Haq I, Ullah R, Din M, Ahmad S, Anwar F, et al. (2020) Unrecognized HIV infection in asymptomatic volunteer blood donors at district Peshawar, Khyber Pakhtunkhwa, Pakistan. New Microbes New Infect 35: 100685.
- Zaheer HA, Waheed U (2014) Blood safety system reforms in Pakistan. Blood Transfusion 12(4): 452-457.
- Zaheer HA, Waheed U (2014) Legislative reforms of the blood transfusion system in Pakistan. Transfusion Medicine 24(2): 117-119.
- (2011) WHO global database on blood safety. Summary report 2011.
- Waheed U, Hasan SI, Wazeer A, Zaheer HA (2016) The status of blood safety in Islamabad, Pakistan. Annals of PIMS ISSN 1815: 2287.
- Ehsan H, Wahab A, Shafqat MA, Sana MK, Khalid F, et al. (2020) A systematic review of transfusion transmissible infections among blood donors and associated safety challenges in Pakistan. Blood 11: 405-420.
- Luby S, Khanani R, Zia M, Vellani Z, Ali M, et al. (2006) Evaluation of blood bank practices in Karachi, Pakistan and the government's response. Health Policy Plan 15(2): 217-22.
- (2018) Country progress report Pakistan. UNAIDS.
- Mir F (2020) Abstract 10626. International AIDS conference.
- Hina J (2021) The mystery of unsafe injections in Pakistan. Daily Times, Pakistan.
- Khan A, Altaf A, Qureshi H, Orakzai M, Khan A (2020) Reuse of syringes for therapeutic injections in Pakistan: Rethinking determinants. Eastern Mediterranean Health Journal 26(3): 283-289.
- Mubarak N, Hussain I, Raja SA, Khan TM, Zin CS (2020) HIV outbreak of Ratodero, Pakistan requires urgent concrete measures to avoid future outbreaks. J Pak Med Ass 70(8): 1475-1476.
- Arulogun OS, Adesoro MO (2009) Potential risk of HIV transmission in barbering practice among professional barbers in Ibadan, Nigeria. Afr Health Sci 9(1): 19-25.
- Nath B, Kumari R, Midha T, Vaswani ND, Lekhwani S (2013) Profession of Barbering: Unexplored issue in HIV/AIDS. Clin Epidimol Glob Health 1(2): 67-73.
- Rai MA, Warraich HJ, Ali SH, Nerurkar VR (2007) HIV/AIDS in Pakistan: The battle begins. Retrovirology 4(1): 22.
- Saif S Shehzad S (2020) Urdu translation and adaptation of the HIV stigma scale in Pakistani injectable drug users with HIV. J Pak Med Ass 70(3): 505-510.
- Ahmed A, Saqlain M, Umair MM, Hashmi FK, Saeed H, et al. (2021) Stigma, social support, illicit drug use, and other predictors of anxiety and depression among HIV/AIDS patients in Pakistan: A cross-sectional study. Front Public Health 9: 745545.
- Abrar N, Ghouri AM (2010) AIDS/HIV knowledge, attitude and beliefs of adolescents of Pakistan. Health Economics Evaluation Methods Journal 16(2): 275-285.
- Bashir S (2011) HIV/AIDS stigma at the workplace: Exploratory findings from Pakistan. Sahara J 8(3): 156-616.
© 2022 Samina Rafique, This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






