- Submissions

Full Text
Psychology and Psychotherapy: Research Studys
Psychological and Psychiatric Aspects of Chronic Pain
Nelson Hendler*
Professor of Neurosurgery and Psychiatry, USA
*Corresponding author: Nelson Hendler, Professor of Neurosurgery and Psychiatry, USA
Submission: December 20, 2020 Published: February 18, 2020

ISSN 2639-0612Volume3 Issue3
Keywords
Severe chronic pain produces; Consistent psychological; Sociological responses in a patient; Regardless of pre-existing; Co-existing psychiatric disease
Introduction
Pain is a poorly understood component of medicine. Despite the fact that pain is one of the most common reasons a patient seeks medical assistance, there is limited understanding of this process. Pain often produces a great deal of anxiety for patient, because it signals that something is wrong within the body. This is further complicated and compounded by the fact that pain is a totally subjective experience. There is no way to accurately and consistently measure pain. However, one of the first questions most physicians ask a patient is “How much pain do you have?” This inanity has been perpetuated by the advent of the most useless of all medical assessments which is an attempt to quantify this subjective experience-the fifth vital sign. Nowadays, a physician asks a patient “How much pain do you have on a scale of one to ten?” and then dutifully records the answer.
Review
More often than not, the physician says, “How could you be having that much pain?” in incredulous tones. Thereafter, a contest ensues, with the patient trying to convince a physician how much pain he or she suffers, and the physician offer dismissing the complaints. Often, the physician-patient exchange focuses on the severity of pain, which has no diagnostic value, in counter distinction to useful information, such as the location of the pain, the type of pain (throbbing, sharp, dull etc.) and what makes it better or what makes it worse. This type of exchange is even more complicated if a psychologist is involved in the care of the patient. Most psychologists have little or no medical training, and thereby follow the normal course of action in medicine, if the only tool you have is a hammer, everything begins to look like a nail.” This statement is not intended to cast aspersions on psychologists. It merely described the harsh reality that in medicine you do not find something unless you look for it. This is further compounded by clinicians who do not even know a medical problem exists.
Therefore, since you do not know of the existence of a problem, you would never look for it. If these antecedent statements seems unduly arrogant, please consider how many people in the medical community are familiar with the medical diagnoses of cluneal nerve entrapment, [1], rotatory subluxation [2] odontoid fracture [3], pyrifomis syndrome [4], Hashimoto’s thyroiditis [5], neuropathies due to Lymes disease and syphilis [6], tarsal tunnel syndrome [7], thoracic outlet syndrome [8,9], Eagle’s syndrome [10], facial pain due to Sjoren’s syndrome [10], glossopharyngeal neuralgia [10], cervical angina [11], C2 entrapment syndrome [12], slipping rib syndrome [8], anteriolysthesis [13], retrolysthesis [13], and internal disc disruption [14], to name a few of the most often overlooked medical disorders. Compounding these commonly missed disorders, how many physicians would know the correct medical test needed to document the presence of these disorders? Therefore, it is incumbent on any clinician involved in the evaluation of chronic pain patients to be an expert medical diagnostician. Without that approach, it is easy to fall into the trap of blaming the patient for not getting well, instead of addressing the issue of misdiagnosis. The best way to study pain is to evaluate a normal response to pain, and then determine if patient deviates from this expected norm. This rationale is applied to medicine in general, since students study anatomy, so they can recognize what normal tissue looks like, in order to appreciate what is abnormal, when they study pathology.
Moreover, studies of pain must be longitudinal, meaning that the patient must be studied over a period of time in order to track the impact of pain on their life, rather than being seen for only one instance, and drawing conclusions from a single exposure. This is especially true in the case of chronic pain, since the psychological response to acute pain is distinct from the response to chronic pain [15]. Another flaw in the study of pain is the failure of physicians recognize that medical disease and psychological disturbance exists on two separate independent axes [16,17]. Physicians want to know if a patient has a valid complaint of pain. Earlier research is flawed, because it said if a patient has coexisting pain and depression, the cause of the pain is the depression- a depressive equivalent-rather than examining the reverse relationship [18,19]. Researchers never looked at the effect of pain over time. Researchers have to study a normal response to appreciate an abnormal response.
Otherwise, medical students couldn’t appreciate what is pathological, without first understanding what normal is [20]. Interestingly, chronic pain patients offer a recognizable pattern of responses to pain over time. By studying this normal longitudinal response, any deviation from the normal would be considered pathological. Normal chronic pain patients (those without any pre-existing psychological conditions) go through 4 stages of responses, remarkable similar to the 5 stages a patient experience when dying [21]. This is a normal response to chronic pain, and has been described by the author since 1982, in various publications [16,22,23]. The four psychological stages of chronic pain are reproduced here.
The acute stage- 0-2 months
At the initial onset of pain, a patient expects to get well, so no psychological changes are evident. Psychological testing, such as the Minnesota Multiphasic Personality Inventory (MMPI) is normal.
The sub-acute stage-2-6 months
The patient has anxiety and somatic concerns develop. They are wondering why they are not getting well. MMPI scales 1 and 3 are elevated. These scales are labeled hypochondriasis and hysteria, but they have not yet become depressed. This leads to the MMPI profile of elevated scales 1 (hypochondriasis) and 3 (hysteria) with a normal scale 2 (depression)-the so-call “Conversion V.”
The chronic stage 6 months-8 years
Patient are depressed, because they are not getting well. They begin to recognize that they may never recover from their chronic pain condition. The MMPI has elevated scale 2, which is the depression scale, more so than scales 1 and 3. If a physician looked at the scoring of the MMPI they would see an inverted V, the so-called “neurotic triad.” This has been called a “pain neurosis” by Blumer [24], a “pain prone patient” by Engel and Pilling [18,25], a “depressive equivalent” by Engel and Anslett [18,19], and more disparagingly a “ low back loser” by Sternbach [26].
The sub-chronic stage-3-12 years
In this stage, the patient resets goals. This process of adaptation leads to normalization of the MMPI, with only scales 1 & 3 elevated, (hypochondriasis and hysteria), and the absence of depression. These four stages, described above, represent the normal response to chronic pain [16, 22,23]. This type of response was observed to occur in over 15,000 patients evaluated by this author. This baseline, normal response to chronic pain, is the response against which all other responses to chronic pain should be judged. More succinctly stated, if a patient does not get depressed after three years of chronic pain, then this is abnormal. However, if they remain depressed after twelve years, this is not a normal response
What are the Questions about Chronic Pain? Does the Patient have a Valid Complaint of Pain?
There are many variables to take into consideration. Pre-existing psychopathology, resultant psychopathology, negative tests, positive tests that do not correlate with the anatomical complaint of pain, (i.e. the patient may have a L5-S1 disc on MRI, but clinically the experience pain in top of thigh, which is compatible with a L2-L3 disc), all influence the diagnostic process. If the response to pain is normal, believe the patient, not the normal medical tests, and keep looking for a source of the pain which would lead to diagnosis. While this seems like an obvious statement, research from a number of physicians at Johns Hopkins Hospital documents the fact that chronic pain patients are misdiagnosed 40% to 80% of the time [27-29]. In specific disorders, such as fibromyalgia, complex regional pain syndrome (CRPS), and sequela of electric shock or lightning strikes, the misdiagnosis rate ranges from 71% to 97% [5,28,30], People with pre-pain psychiatric illness can also get medical illness. This is not conversion. A simple way to conceptualize this is presented in Figure 1.
Figure 1: The independence of organic problems and psychological problems [17].

Patients can have both psychiatric disease and organic pathology co-existing. Schizophrenics get brain tumors, and hysterics get disc disease. Psychiatric disease does not confer an immunity on the patient against getting a medical disease. A physician should treat each patient as if they have organic pathology and give patient the benefit of the doubt. In order to help a physician, conceptualize a framework for evaluating chronic pain patients, a team physician at the chronic pain treatment center at Johns Hopkins Hospital developed four broad psychological categories of chronic pain patients [22].
Objective pain patient
These are patients with a good pre-morbid adjustment, objective medical findings, and who go through the 4 stages of the response to chronic pain described above. Research has found that 87%-94% of all chronic pain patients fall into this category.
Exaggerating pain patient
Poor pre-morbid adjustment, minimal findings, and absence of depression. These patients are not malingering, but merely exaggerating a minimal medical finding, to manipulate a situation. An example would be a patient with a histrionic personality disorder, with a bulging disc. Between 6% to 13% of all chronic pain patients fall into this category.
Affective or Associative pain patients
A patients with a poor pre-morbid adjustment, no objective findings and very difficult to manage by medical or psychiatric means. Hysterical scoliosis, organic brain syndrome, and malingering would fall into this category. These are rare patients, and account for less than 1% of all chronic pain patients.
Undetermined pain patient
A patient with a good pre-morbid adjustment, a normal response to chronic pain, but no abnormal medical testing. This patient warrants a more extensive medical evaluation. This is not malingering. There is a fifth category, which is a mixed objective-exaggerating pain patient: These patients have a poor pre-morbid adjustment, a definite organic basis for their complaint of pain, but their poor personality adjustment is superimposed upon the normal response to pain, so that they become real management problems. They are not faking. They are not malingering. However, these are the patients who a doctor dreads managing. Therefore, they often get assigned a psychiatric diagnosis, and care is shifted to a psychiatrist, even though there is a real organic basis for their complaint of pain. It often is incumbent on a psychiatrist to wade through the obscuring psychiatric difficulties to uncover the medical issue.
Psychological testing for chronic pain patients
Ronald Melzack, PhD is E. P. Taylor Professor of Psychology at McGill University and research director of the Pain Clinic at the Montreal General Hospital. Dr. Melzack, with his colleagues at McGill University, developed the McGill-Melzack pain test, which measures the subjective pain experience using 3 categories of word descriptors: sensory, affective and evaluative. The test also contains an intensity scale and other items to describe pain [31]. The test was designed to provide a quantitative measure of pain, so it can be used to measure improvement. There is no research correlating the results of this test with the presence or absence of organic pathology. Despite this effort, the severity of pain has no diagnostic value, and only limited clinical value. Often, it engenders conflict between patient and doctor. The typical exchange reflects this problem. A patient says, “I have horrible pain, which is unbearable” and displays an ingrown toenail. The doctor looks at the toenail and says “That doesn’t look too bad to me. You can’t be having that much pain.” When the quantification of pain leads to decisions about the potency and quantity of narcotics to be prescribed, the potential for acrimonious discussions is obvious. The Minnesota Multiphasic Personality Inventory (MMPI) is a self-administered test, with choices of answers which are only true or false. There are 566 questions to the test. The test was developed to determine personality types in individuals, i.e. manic depressive, schizophrenic, hysteric, depressive, obsessive, hypochondria, etc. [32]. A new version of the MMPI, the MMPI II, is now in use [33].
Sample questions from the MMPI are:
“I like mechanics magazines-True or False?”
“I hear voices and don’t know where they are coming from-True or False?”
“I have more pain than most of my friends-True or False?”
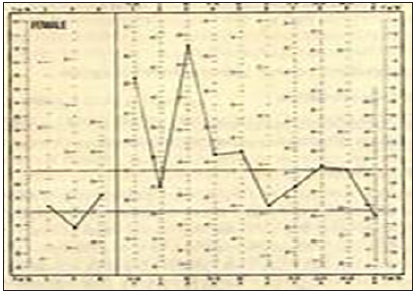
From these answers, the test predicts personality types, and then from personality types said it could predict if a patient had real pain. However, there are there are very few articles in the medical literature which attempt to correlate findings on MMPI scales with medical findings. These articles show that there is no correlation, nor predictive value to the MMPI [34-37]. Many of the early stage chronic pain patients were called conversion reactions by researchers [38]. They based these conclusions on the elevated scales of 1 and 3 (hysteria and hypochondriasis), of the MMPI, and the absence of the elevation of scale 2 (depression). This formed the so called “Conversion V” because the graph of the scales has a V in it when plotting the first three scales (Figure 2).
Figure 2: A Conversion ‘V‘ plotted on the MMPI. Note that scales 1 and 3 (Hy and Hs) are in the abnormal range and are higher than scale 2 (D), which is in the normal range.
However, as pain progresses over time, depression begins to emerge. This is an important concept. Most researchers report the MMPI is a measure of personality traits, and the test results do not change over time [39]. Nothing could be further from the truth. The chronic stage of chronic pain changes the MMPI profile, with scale 2 (depression) becoming abnormally high, and both scales 1 and 3 remaining elevated [16]. In Figure 3 Pilling, Engel, Sternback and others, based on their misunderstanding of the four stages of pain and the MMPI, labeled these chronic pain patients as a “Pain prone patient,” “depressive equivalent,” “pain neurosis,” or “low back loser” [18,19,24-26]. The researchers use these pejorative terms because they had groups of patients with abnormal MMPI findings and no abnormalities on medical testing. Therefore, they all concluded that the patients were using chronic pain as a way of getting attention, because of their underlying psychological abnormalities. They did their patients, and medicine in general, a great disservice.
Figure 3: A “neurotic triad” graph on MMPI. This is so-called because scales 1,2 and 3 are elevated to an abnormal level, with scale 2 (depression) being more elevated than scale 1 and 3 (Hy and Hs).
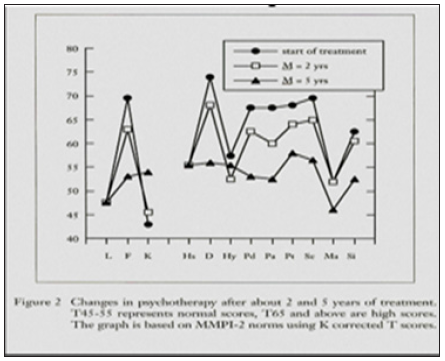
The theory states that the MMPI doesn’t change over time, since it measures personality characteristics, or personality traits. However, research by Gordon and Fishbain [33,40], clearly illustrates that the MMPI does change over time. Researcher claim the MMPI can tell if a patient is faking their pain or not, based on MMPI score. This is an erroneous statement, since the MMPI in a person who has chronic pain will change as the depression changes, giving a “Conversion V” in the early and late stages, and a “Neurotic triad” (elevated depression scale) during the chronic stage. Both of these are normal responses to chronic pain. Hagedorn [41] and his colleagues followed 50,000 patients for 25 years. This is the only prospective study on MMPI ever done. They all received the MMPI when they first entered the Mayo Clinic system. Of these 50,000 patients, 68 of them had back surgery. Hagedorn found no difference in pre-surgery MMPI between those who did do well or didn’t do well with surgery. The MMPI is not consistent in predicting the presence or absence of organic pathology. Not one single scale ever correlates, consistently, with the presence or absence of organic pathology [34-37]. It can be safely said that the MMPI has no predictive ability, nor has the ability to determine whether or not a patient has a valid complaint of pain or is faking. Aaron Temkin Beck, professor emeritus in the department of psychiatry at the University of Pennsylvania. is widely regarded as the father of cognitive therapy.
His Beck Depression Inventory (BDI, BDI-II) is a 21-question multiple-choice self-report inventory, one of the most widely used instruments for measuring the severity of depression [42]. Depression can be thought of as having two components: a) the affective component (e.g. mood) and b) the physical or "somatic" component (e.g. loss of appetite). The BDI-II reflects this and can be separated into two subscales. The purpose of the subscales is to help determine the primary cause of a patient's depression. The development of the BDI represented a shift in health care professionals' view of depression from a Freudian, psychodynamic perspective, to one guided by the patient's own thoughts or "cognitions". The BDI was developed to provide a quantitative assessment of the intensity of depression. It can monitor changes over time, and track improvement of depression and even risk of suicide [42]. Depression from chronic pain does not come without consequences. Chronic pain patients commit suicide at a higher rate than the general population. White males with pain complete suicide at a rate twice as high than the general population. White females with pain complete suicide at a rate three times higher than the general population.
White males with pain, involved in workers’ compensation litigation complete suicide at a rate three times higher than the general population. Therefore, any threats of suicide from a chronic pain patient must be taken seriously. Worse yet, suicide attempts are not gesturing. So, it is of upmost importance to monitor depression in chronic pain patients [43-46]. The SCL-90-R has 90 items. It takes 12-15 minutes to administer. The SCL-90 was developed by Len Derogaitis, PhD at Johns Hopkins Hospital. It has nine scores along primary symptom dimensions: somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism These are personality states, which differ from traits [47,48]. States change over time, which can be measured by the SCL-90, unlike the MMPI, which measures traits, which theoretically don’t change over time. However, research has proven that the MMPI scales do change over time, so its stated reliability is suspect [47,48]. Physicians at Johns Hopkins Hospital recognized the limitations of the MMPI. Therefore, in the 1970’s they decided to develop their own test to meet their needs and answer their questions.
The neurosurgeons wanted to know if a patient complained of pain was the pain valid. So, a team of physicians, led by the psychiatrist at the Chronic Pain Treatment Center of Johns Hopkins Hospital, developed a test to answer this question. The pain validity test is available on the Internet, at www.MarylandClinicalDiagnostics.com or www.DiagnoseThePains.com. This test is able to validate pain, by predicting the presence or absence of organic pathology. It allows a physician to improve diagnostic accuracy and serves as a screening tool to help get an accurate diagnosis. There are 9 multi-authored articles about the Pain validity test, involving 794 patients [49-57]. The test has 32 questions and takes only 15 minutes for a patient to complete the self-administered test. A clinician can obtain results in 5 minutes after the test is completed. It is available in English and Spanish at
www.MarylandClinicalDiagnostics.com or www.DiagnoseThePains.com.
Based on the recent publication on the Internet version of the test, it can predict who will have an abnormality on the correct objective medical tests with 95% accuracy, and the pain validity test can predict who will not have abnormalities or only mild abnormalities with 85%-100% accuracy [55]. The pain validity test can assess the validity of the complaint in the chronic pain patient, regardless of pre-existing or co-existing psychological problems, which is far better than the MMPI. It adheres to the precept that the development of pain is independent of personality traits, unlike MMPI research. The self-administered version is available at www.MarylandClinicalDiagnostics.com. The research results of the pain validity test provide objective medical information. The pain validity test found that 87% to 94% of chronic pain patients score as an objective pain patient on the pain validity test [49-55]. However, of these objective pain patients, 40%-80% are misdiagnosed [27,29,30].
Figure 4: Scattergram comparing the pain validity test score to the severity of abnormalities on objective medical testing.
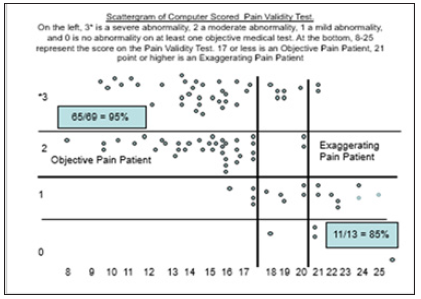
Please refer to the Scattergram in Figure 4 which is from a recently published article about the Pain validity test, which is the Internet based version of the test [53]. The severity of a medical abnormality on objective medical testing was score as a 0, meaning no abnormalities, 1 meaning mild abnormalities, 2 meaning moderate abnormalities, and 3 meaning sever abnormalities. These are represented by the left-hand vertical column. Objective pain patients score between 0 to 17 points on the pain validity test. They have a 95% chance of having moderate or severe abnormalities on at least one objective measure of organic pathology, such as EMG nerve conduction studies, root blocks, facet block, provocative discograms, MRI, CT, etc. Exaggerating patients score 21 points or greater. The mixed objective-exaggerating chronic pain patients score between 18-20 points. The pain validity test can identify and predict the patients who will not have medical abnormalities with 85% accuracy. Only 6%-13% of patients are exaggerating chronic pain patients. Medical articles prove that the MMPI has no predictive medical capabilities. Insurance companies often claim that the MMPI does detect fraud but can’t prove it. In fact, in a number of cases, the MMPI has been disallowed in court, especially in Florida [58,59]. On the other hand, the Pain validity test always has been admitted as evidence in 9 states in over 30 cases [60].
Overused Terms
The psychiatric and medical literature is filled with terms which are ill-defined, or improperly used. Clearly, there is a need for precision in any research study, and precision begins with the proper definition of terms. The Diagnostic and Statistical Manual IV (DSM IV) of the American Psychiatric Association makes an effort to standardize these terms. Conversion reaction is defined as an unconscious manifestation of a physical problem (usually visible) without an organic basis (300.11- DSM-IV). The key word in this definition is the unconscious selection of symptoms. Another important consideration is the need to select a symptom which is visible, so the patient can convey to others that they are “ill.” The incidence of conversion disorder has been relatively consistent over 50-year period of time. In 1913, Kemp found that less than 1% of the admissions to Phipps Clinic, the psychiatric wing of Johns Hopkins Hospital, were conversion reactions [61]. Fifty years later, Stephens, also from Johns Hopkins Hospital, reported that less than 2% of admissions to the Phipps Clinic were for conversion reaction [62]. Thirty years after that, Hendler, also Johns Hopkins Hospital, reported that only 3 of the 6000 (0.05%) of chronic pain patients evaluated had the diagnosis of conversion reaction [63]. Slater did a 9-year follow-up on 85 patients diagnosed as conversion hysteria at Queens Square Neurological Hospital in London [64]. Only 7/85 were confirmed as conversion. The rest were diagnosed with atypical myopathy, trigeminal neuralgia, disseminated sclerosis, dementia, thoracic outlet syndrome, epilepsy, vestibular lesions, Takayasu’s syndrome, neoplasms, schizophrenia, somatizing disorders, cord compression, and endogenous depression, which have not yet manifested at the time of the original diagnosis of conversion reaction.
From the review in the psychiatric literature and the medical literature, one can conclude that the incidence of hysterical conversion reaction is small in a general psychiatric population (1%-2% of admissions). The incidence of hysterical conversion in a chronic pain population that is properly diagnosed, is even smaller (3/6000 or .05%). Even after diagnosed with conversion reaction, there is less than a 10% chance the patient really has this, and most likely has medical disease. Conversion reactions (300.11 DSM IV) usually manifest as visible symptoms which can be recognized by another person, such as paralyzed limb, blindness, or falling. One great oversight in the DSM-IV manual was the failure to mention that the disorder does not produce distress in the patient (“La belle indifference”). Essentially, this means the patient has a problem which should be distressful to a normal individual, but they don’t seem the least bit concerned by the medical problem.
The symptoms of the conversion reaction will remit with amobarbital narcosynthesis, at adequate doses (>450mg) Hendler, a psychiatrist at Johns Hopkins Hospital and Filtzer an orthopedic surgeon at Johns Hopkins Hospital, described a case of hysterical scoliosis diagnosed by the orthopedic surgeon, which did not respond to Amytal, but responded under general anesthesia [65]. This case of hysterical scoliosis-a woman leaning to the side, without an organic basis for this, had a visible symptom, conveying to others “I am sick.” The experienced orthopedic surgeon dismissed the failure to respond to narcosynthesis and use general anesthesia to relax the patient. Apparently, the psychiatrist had not used an adequate amount of amobarbital for the initial narcosynthesis session. Under subsequent narcosynthesis sessions, the patient revealed that she had conflicts with intermarriage, which she could not resolve by speaking to her husband. Again, this is compatible with the conversion reaction, since this conflict represented an unexpressed psychological issue. Pain is a bad conversion symptom, because it is not visible, and even people with real pain have trouble convincing people they have something wrong. Clearly, scoliosis was much more visible. Malingering is defined as a conscious attempt to deceive for personal gain (316.V65.2-DSM-IV). One of the hallmarks of this diagnosis is the refusal of patients to go for tests. The other critical element of this diagnosis is the deceit, which, in contradistinction to a conversion reaction, is a willful and purposeful act. Insurance companies use detectives and functional capacity evaluations (FCE) to try to ferret out the fakers and malingerers. Unfortunately, the “common wisdom” of the insurance industry is not so wise. The insurance industry thinks that 20% to 80% of workers compensation for auto injury claimants are malingering or faking, but this is not substantiated by any clinical research. In a more precise evaluation, Hendler determined that 6% to 13% of chronic pain patients involved in litigation are malingering [66].
Pain Disorder (307.80- DSM-IV) defined as a pain for which is there is no medical explanation. A diagnosis of this type immediately raises red flags. If a physician overlooks the diagnosis, or orders an incorrect test, he or she will not have a medical explanation for the pain complaint which the patient has. Therefore, instead of blaming the physician for the failure of diagnosis, it is much more convenient to blame the patient. Indeed, a group of physicians from Johns Hopkins Hospital that published a series of research articles, documenting that 40% to 80% of chronic pain patients are misdiagnosed [27-29]. For specialized disorders, like complex regional pain syndrome (CRPS), survival after electrical shock or lightning strike, or fibromyalgia, the misdiagnosis rate ranges from 71% to 97% [5,28,30]. Somatoform Disorder (300.81- DMM-IV) defined as a cluster of 4 pain, 2 GI, 1 sexual and 1 pseudo-neurological symptoms without medical diagnosis. The same cautionary note as found in “pain disorder” can be applied to this diagnosis. Depressive Equivalents were more fully explained above. The theory behind this so-called “diagnosis” was that if depression and pain coexist at the same time, the patient was having difficulty expressing their depression, and resorted to pain as an explanation for why they were not functioning. More careful research has dispelled this erroneous cause-and-effect relationship, and proved quite the reverse, i.e., chronic and persistent pain, by the sixth month, will cause depression, and depression which could last as much as eight years.
There is one disturbing trend which appears in the medical literature. It seems that when a physician cannot diagnose a patient or does not understand the cause of the patient’s pain, the doctor has a tendency to blame the patient for the problem or accuse the patient a faking or malingering. This is particularly true in patients with coexisting or pre-existing psychological problems. Therefore, as before, it is essential to understand what a normal response to pain is. Also, the physician has to apply logic to his or her interpretation of data. Just because two events correlate with one another does not mean that they are related in the cause-effect fashion. This is particularly true if a physician is studying a group of patients only on a “slice of time” basis, i. e. not following the patients longitudinally. As an example, researchers studied patients admitted to Mensana Clinic. This study was performed longitudinally on chronic pain patients. The study reported that patients are not depressed and then get pain, but rather they get pain and, after six months, as the result of the pain, they get depressed [37]. At the time these patients were initially seen, 77% of the chronic pain patients were depressed, as confirmed by Beck scores. However, the researchers asked questions about past experience with depression, and found 89% had never been depressed before the onset of their pain [37]. So even though there was a high correlation between patients with depression in patients with chronic pain, when examined in a single period of time, when researchers studied the population longitudinally, the cause- effect relationship emerged. This research points out the flaw in the research by physicians, who described “depressive equivalents” in patients with both depression and chronic pain [18,19]. The ascribed the pain as being caused by depression. However, quite the reverse is true. If one critically evaluates the diagnostic criteria in DSM-IV for somatoform disorder, pain disorder, and depressive equivalents, which is “Pain without a medical explanation.” then a poor medical work-up lead to these DSM “diagnoses,” it is apparent that these diagnoses use circular logic. The diagnoses become self-fulfilling prophecies, i.e. if you can’t determine the correct medical diagnosis in the patient than the patient obviously doesn’t have a medical diagnosis, and it must be a psychiatric diagnosis. Nothing could be further from the truth. These diagnoses offer an excuse for sloppy medicine. The insurance industry has for years over-estimated the prevalence of faking and malingering in their claimants [66].
Despite objective evidence, insurance companies feel 20%-80% of their claimants are faking [66]. In reality, the real reason their claimants are not returning to work is due to the prevalence of misdiagnosis in chronic pain patients [66]. In fact, Elaine Howle, the auditor for the State of California, reports that the $30,000,000 a year spent to detect fraud in workers’ compensation cases in the State of California, is not cost effective [67]. Clearly, the cause for failure to return to work is misdiagnoses, not fraud. There are other uses for the pain validity test. In light of the recent concerns about opioid overuse, the pain validity test can be used to detect drug seeking behavior, in patients who have minimal medical issues but look for narcotics, or who absolutely fake their complaints of pain. The pain validity test can be used to detect the drug seeking patients with 95% accuracy [57]. If a clinician utilizes the results of the pain validity test in conjunction with rational pharmacological application, which allows a physician to prescribe effective non-narcotic medication for chronic pain patients, [68], there is a chance to reduce the overuse of narcotics. In fact, when this system was applied to a group of patients at Mensana Clinic, in combination with accurate diagnosis, the use of narcotics was reduced 89% [37]. The other predictive application of the pain validity test was determining who would have abnormalities at the time of surgery. The Pain validity test was able to predict, with 94% accuracy, who would have abnormalities at the time of surgery.
Conclusion
- The current methods of assessing chronic pain are not cost effective, and not accurate.
- Misdiagnosed patients cost insurance companies much more than fraudulent cases.
- The Pain validity test is a reliable method for predicting and detecting organic pathology regardless of co-existing or pre-existing psychological problems.
- Psychological care alone has not been documented as effective in chronic pain patient treatment.
- Depression is caused by chronic pain, not the reverse.
- Any clinician should demand Evidence Based Medicine proof of efficacy of treatment.
See www.MarylandClinicalDiagnostics.com or www.DiagnoseThePains.com for access to the Pain validity test.
References
- Long DM (2018) Why 40%-80% of chronic pain patients are misdiagnosed and how to correct that. In: Hendler N (Ed.), Nova Science Publishers, New York, USA.
- Hendler N (2018) Why 40%-80% of chronic pain patients are misdiagnosed and how to correct that. Nova Science Publishers, New York, USA, pp. 216-217.
- Hendler N (2018) why 40%-80% of chronic pain patients are misdiagnosed and how to correct that. Nova Science Publishers, New York, USA, pp. 217-218.
- Hendler N (2018) Why 40%-80% of chronic pain patients are misdiagnosed and how to correct that. Nova Science Publishers, New York, USA, pp. 219-220.
- Hendler N, Romano T (2016) Fibromyalgia over-diagnosed 97% of the time: Chronic pain due to thoracic outlet syndrome, acromo-clavicular joint syndrome, disrupted disc, nerve entrapments, facet syndrome and other disorders mistakenly called fibromyalgia. Anesth Pain Med 1(1): 1-7.
- Hendler N (2018) Why 40%-80% of chronic pain patients are misdiagnosed and how to correct that. Nova Science Publishers, New York, USA p. 140.
- Gracia BE, Gadea SJ, Celis LC, Gadea SE, Bellmunt PA, et al. (2019) Dimensional changes of the tibial nerve and tarsal tunnel in different ankle joint positions in asymptomatic subjects. J Foot Ankle Surg 58(6): 1129-1133.
- Hendler N, Gallagher W, Laynee L (2019) Missed diagnoses associated with rear-end collisions. Clin Ex Orth 1(1).
- Koschorke EL, Hendler N, Koloony L, Kraus H (1990) Tips on hard to manage pain syndromes. Patient Care pp. 104-118.
- Hendler N (2017) Facial pain from various sources-diagnoses and differential diagnoses. Dent Oral Craniofac Res 3(5): 1-5.
- Sussman W, Makovitch SA, Merchant SH, Phadke J (2015) Cervical angina: An overlooked source of noncardiac chest pain. Neurohospitalist 5(1): 22-27.
- Long D, Davis R, Speed W, Hendler N (2006) Fusion for occult post-traumatic cervical facet injury. Neurosurg Q 16(3): 129- 134.
- Hendler N (2018) Why 40%-80% of chronic pain patients are misdiagnosed and how to correct that. Nova Science Publishers, New York, USA, pp. 220-221.
- Hendler N (2018) Why 40%-80% of chronic pain patients are misdiagnosed and how to correct that. Nova Science Publishers, New York, USA, pp. 201-202.
- Wise T, Hall W, Wong O (1982) Chapter 2: Factors determining the acute pain response, in diagnosis and treatment of chronic pain. In: Hendler N, Donlin L, Wise T (Eds.), Wright-PSG, Boston, USA, pp. 9-22.
- Hendler N (1982) Chapter 1: The four stages of pain, in diagnosis and treatment of chronic pain. In: Hendler N, Donlin L, Wise T (Eds.), Wright-PSG, Boston, USA, pp. 1-8.
- Hendler N, Talo S (1989) Chapter 2: Chronic pain patients versus the malingering patient, in current therapy of pain. In: Kathy F, Richard P (Eds.), BC Decker, Inc., Toronto, Philadelphia, USA, pp. 14-22.
- Engel GL (1959) Psychogenic pain and the pain prone patient. Am J Med 26: 899-918.
- Anstett RE, Poole SR (1982) Depressive equivalents in adults. Am Fam Physician 25(3): 151-156.
- Hendler N (1997) Chapter 2: Psychological and psychiatric aspects of pain, in neurosurgical management of pain. In: Richard N, Robert L (Eds.), Springer-Verlag: New York, USA.
- Ross KE (1975) On death and dying. Bull Am Coll Surg 60(6): 15-17.
- Hendler N (1981) Chapter 3: The four categories and basis of their formulation, in diagnosis and non-surgical management of chronic pain. Raven Press, New York, USA, pp. 12-15.
- Hendler N (1984) Depression caused by chronic pain. J Clin Psychiatry 45(3 Pt 2): 30-38.
- Blumer D (1975) Psychiatric considerations in pain. In: Rothman R, Simeone R (Eds.), WB Saunders Co., Philadelphia, USA.
- Pilling LF, Brannick TL, Swenson WM (1967) Psychologic characteristics of psychiatric patients having pain as a presenting symptom. Can Med Assoc J 97(8): 387-394.
- Sternbach RA, Murphy RW, Akeson WH, Wolf SR (1973) Chronic low back pain: Characteristics and management of the low back loser. Postgrad Med 53: 135-138.
- Dellon AL, Andronian E, Rosson GD (2009) CRPS of the upper or lower extremity: Surgical treatment outcomes. J Brachial Plex Peripher Nerve Inj 4(1): 1-7.
- Hendler N (2002) Differential diagnosis of complex regional pain syndrome. Pan Arab Journal of Neurosurgery pp. 1-9.
- Hendler N, Bergson C, Morrison C (1996) Overlooked physical diagnoses in chronic pain patients involved in litigation. Psychosomatics 34(6): 494-501.
- Hendler N (2005) Overlooked diagnoses in chronic pain: Analysis of survivors of electric shock and lightning strike. J Occup Environ Med 47(8): 796-805.
- Melzack R (1975) The McGill pain questionnaire: Major properties and scoring methods. Pain 1(3): 277-299.
- Repko GR, Cooper R (1985) The diagnosis of personality disorder: A comparison of MMPI profile, million inventory, and clinical judgment in a worker’s compensation population. J Clin Psychol 41(6): 867-881.
- Gordon RM (2001) MMPI/MMPI-2 changes in long-term psychoanalytic psychotherapy. Issues in Psychoanalytic Psychology 23(1-2): 59-79.
- Hendler N, Mollett A, Viernstein M, Schroeder D, Rybock J, et al. (1985) A Comparison between the MMPI and the 'Mensana clinic back pain test’ for validating the complaint of chronic back pain in women. Pain 23(3): 243-251.
- Hendler N, Mollett A, Viernstein M, Schroeder D, Rybock J, et al. (1985) A Comparison between the MMPI and the 'Hendler back pain test' for validating the complaint of chronic back pain in men. The Journal of Neurological & Orthopaedic Medicine & Surgery 6(4): 333-337.
- Hendler N, Mollett A, Talo S, Levin S (1988) A comparison between the Minnesota multiphasic personality inventory and the 'Mensana clinic back pain test' for validating the complaint of chronic back pain. J Occup Med 30(2): 98-102.
- Hendler N (1988) Validating and treating the complaint of chronic back pain: The Mensana clinic approach. Clin Neurosurg 35: 385-397.
- Leavitt F (1985) The value of the MMPI conversion 'V' in the assessment of psychogenic pain. J Psychosom Res 29(2): 125-131.
- Merskey H (1972) Personality traits of psychiatric patients with pain. J Psychosom Res 16(3): 163-166.
- Fishbain DA, Cole B, Cutler RB, Lewis J, Rosomoff HL, et al. (2006) Chronic Pain and the measurement of personality: Do states influence traits? Pain Med 7(6): 509-529.
- Hagedorn SD, Maruta T, Swanson RC (1984) Pre-morbid MMPI profiles of low back pain patients: Surgical successes versus surgical failures. Pain 18: S258.
- Green KL, Brown GK, Hyman JS, Cha J, Steer RA, et al. (2015) The Predictive validity of the beck depression inventory suicide item. J Clin Psychiatry 76(12): 1683-1686.
- Fishbain DA (1999) The association of chronic pain and suicide. Semin Clin Neuropsychiatry 4(3): 221-227.
- Fishbain DA (1996) Current research on chronic pain and suicide. Am J Public Health 86(9): 1320-1321.
- Fishbain DA (1995) Chronic pain and suicide. Psychother Psychosom 63(1): 54-55.
- Fishbain DA, Goldberg M, Rosomoff RS, Rosomoff H (1991) Completed suicide in chronic pain. Clin J Pain 7(1): 29-36.
- Derogatis LR, Rickels K, Rock AF (1976) The SCL-90 and the MMPI: A step in the validation of a new self-report scale. Br J Psychiatry 128: 280-289.
- Derogatis LR, Melisaratos N (1983) The brief symptom inventory: An introductory report. Psychol Med 13(3): 595-605.
- Hendler N, Mollett A, Viernstein M, Schroeder D, Rybock J, et al. (1985) A Comparison between the MMPI and the 'Mensana clinic back pain test' for validating the complaint of chronic back pain in women. Pain 23(3): 243-251.
- Hendler N, Mollett A, Viernstein M, Schroeder D, Rybock J, et al. (1985) A Comparison between the MMPI and the 'Hendler back pain test' for validating the complaint of chronic back pain in men. The Journal of Neurological & Orthopaedic Medicine & Surgery 6(4): 333-337.
- Hendler N, Mollett A, Talo S, Levin S (1988) A comparison between the Minnesota multiphasic personality inventory and the 'Mensana clinic back pain test' for validating the complaint of chronic back pain. Journal of Occupational Medicine 30(2): 98-102.
- Hendler N (1988) Validating and treating the complaint of chronic back pain: The Mensana clinic approach. In: Black P, Alexander E, Barrow D (Eds.), Clinical Neurosurgery. Williams and Wilkins: Baltimore, USA 35: 385-397.
- Hendler N, Viernstein M, Gucer P, Long D (1979) A preoperative screening test for chronic back pain patient. Psychosomatics 20(12): 801-808.
- Hendler N, Cashen A, Hendler S, Brigham C, Osborne P, et al. (2005) A multi-center study for validating the complaint of chronic back, neck and limb pain using the Mensana clinic pain validity test. Forensic Examiner Summer 14(2): 41-49.
- Hendler N, Baker A (2008) An Internet questionnaire to predict the presence or absence of organic pathology in chronic back, neck and limb pain patients. Pan Arab Journal of Neurosurgery 12(1): 15-24.
- Davis R, Hendler N, Baker A (2016) Predicting medical test results and intra-operative findings in chronic pain patients using the on-line pain validity test. Anesthesia & Critical Care: Open Access 5(1): 00174.
- Hendler N (2017) An Internet based questionnaire to identify drug seeking behavior in a patient in the ed and office. J Anesth Crit Care Open Access 8(3): 00306.
- Butcher JN, Arbisi PA, Atlis MM, McNulty JL (2003) The construct validity of the lees-haley fake bad scale. Does this scale measure somatic malingering and feigned emotional distress? Arch Clin Neuropsychol 18(5): 473-485.
- Sims DC (2007) The myth of malingering: Is it the truth or a lie? The Plaintiff Magazine pp. 1-4.
- https://www.slideshare.net/DiagnoseMyPain/pvt-used-in-court-in-word
- Kemp S (1913) Conversion reactions in hysteria. Am J of Insanity 34(3): 45-61.
- Stephens J, Kamp M (1962) On some aspects of hysteria: A clinical study. J Nerv and Mental Disease 134: 305-315.
- Hendler N (1981) Chapter 10-exaggerated pain caused by personality disorder: The histrionic personality versus the hysterical neurosis. In diagnosis and non-surgical management of chronic pain. Raven Press, New York, USA, pp 64-79.
- Slater E (1965) Diagnosis of hysteria. Br Med J 1(5447): 1395-1399.
- Hendler N, Filtzer D, Talo S, Panzetta M, Long D (1987) Hysterical scoliosis treated with amobarbital narcosynthesis. The Clinical Journal of Pain 2: 179-182.
- Hendler N (2013) An internet based expert system to control workers compensation costs documented by outcome studies. Anaesthesia, Pain & Intensive Care 17(2): 166-170.
- Howle E (2004) California does a poor job of combating worker’s comp fraud in workers compensation report, 15(11): 206.
- Hendler N (2018) Medication treatment of chronic pain without opioids, scimaze. Anaesth Pain Management 1: 101.
© 2020 Nelson Hendler, This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






