- Submissions

Full Text
Psychology and Psychotherapy: Research Studys
The First Appearance of Persistent Dementia and Psychosis after a Generalized Sepsis
C Lazzari*, T Rajanna, A Nusair
Department of Psychiatry, UK
*Corresponding author: C Lazzari, Department of Psychiatry, UK
Submission: March 11, 2019Published: March 25, 2019

ISSN 2639-0612Volume2 Issue3
Short Communication
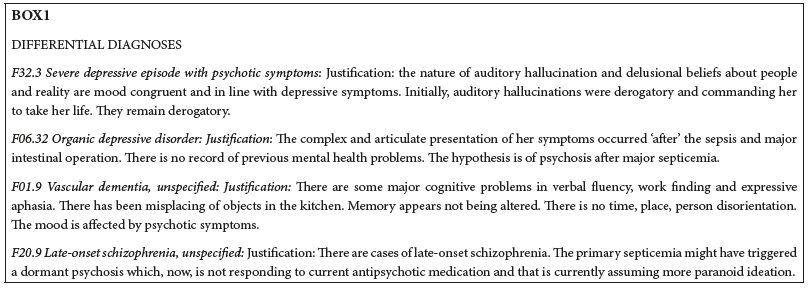
Research suggests that neuroinflammation of the brain has a role in dementia by activating glial cells which then release proinflammatory agents and lipopolysaccharide (LPS) responsible for cognitive deficits [1-3]. Other authors suggest that there is no clear evidence if neuroinflammation after generalized infection is a cause, agent, or consequence of Alzheimer’s Disease (AD) with bacterial LPS acting on neurons and microglia [4,5]. The current case study refers to a 64-year old lady who developed symptoms of dementia and psychosis a month after she was operated for a duodenal perforation resulting in pneumoperitoneum and generalized bacterial sepsis. Neuropsychiatric and clinical assessment gathered the required data. Past psychiatric history was negative, and former cognitive deficits were non-existent before the systemic inflammation. At assessment, brain Magnetic Resonance Image presented mild to moderate supratentorial small vessel disease and mild cortical and subcortical atrophy. Addenbrooke’s ACE-III total score was 74/100: Attention 18/18, Memory 18/26, Fluency 5/14, Language 20/26 and visuospatial 13/16. The cognitive impairment persisted also after the underlying depression was stabilized. The patient became doubly incontinent and started misplacing objects in her kitchen, confusing the use of familiar objects, and having difficulties in word finding. The Bristol Activity of Daily Living was 10/60. The comprehensive neurocognitive assessment resulted in good episodic memory, poor attention, misplacing objects, social phobia, and subjective memory problems with the inability to complete routine tasks. The neuropsychiatric presentation included believing that her food was poisoned, that one of her daughters was a fake, deeming that people on the road (outside her house) were making derogatory comments about her and passing her intrusive thoughts, and thought block. Passivity experiences consisted in thinking that passers-by were able to interfere with her mind or command her to harm herself. She also had auditory-commanding hallucinations to harm herself, believing deriving from people passing by her house. Other auditory hallucinations included hearing people walking on the stair of her house, hearing someone knocking on the door of her bedroom when no one was there, and tactile hallucinations as if someone was tapping on her shoulders when she was alone in her room. We posed the diagnosis of AD and psychosis. After several months, the presentation remains unchanged. The differential diagnoses (Box 1) utilizing ICD-10 (WHO, International Classification of Diseases) included a severe depressive episode with psychotic symptoms (F32.3), organic depressive disorder (F 06.32), vascular dementia (F01.9), and late-onset schizophrenia (F20.9). All these presentations might have been triggered or caused by brain inflammation targeting specific microglia or brain microcirculation hence resulting in permanent damage leading to the onset of dementia and psychosis. Therefore, the authors of the current research speculate that in the case described, systemic inflammation enduringly unlocked dementia, cognitive deficits, and psychosis [6]. The mediator of the unlocking process could be a hypothetical Alzheimer Triggering Factor linked to the microglia activated by LPS which causes a cascade of processes leading to irreversible dementia.
Figure :
References
- Bevan-Jones WR, Surendranathan A, Passamonti L, Patricia Vázquez Rodríguez P, Arnold R, et al. (2017) Neuroimaging of Inflammation in Memory and Related Other Disorders (NIMROD) study protocol: a deep phenotyping cohort study of the role of brain inflammation in dementia, depression and other neurological illnesses. BMJ Open 7(1): e013187.
- Reale M, Brenner T, Greig NH, Inestrosa N, Paleacu D (2010) Neuroinflammation, AD, and Dementia. Int J Alzheimers Dis 2010: 1-2.
- Cunnigham C, Campion S, Lunnon K, Murray CL, Woods JFC, et al. (2009) Systemic inflammation induces acute behavioural and cognitive changes and accelerates neurodegenerative disease. Biol Psychiatry 65(4): 304- 312.
- Heneka MT, Carson MJ, El Khoury J, Landreth GE, Brosseron F, et al. (2015) Neuroinflammation in Alzheimer’s diseases. Lancet Neurol 14(4): 388-405.
- Enciu AM, Popescu BO (2013) Is there a causal link between inflammation and dementia? Biomed Res Int 2013: 316495.
- Lazzari C, Rajanna T, Nusair A, Lyall J (2019) Post-infection dementia and psychosis. Proceedings of the 27th Congress of European Psychiatric Association, Warsaw, Poland.
© 2019 C Lazzari. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






