- Submissions

Full Text
Orthopedic Research Online Journal
Distal Femur Fracture and its Management: A Case Report Preventing Permanent Disability
Harsh Shah1, Zeal Soni2, Hiren Shah1, Abhishek K Taraviya1, Jaydeep Patel1 And Dev Desai2*
1GCS Medical College and Hospital, Ahmedabad, India
2Smt. NHL Municipal Medical College, Ahmedabad, India
*Corresponding author:Dev Desai, Smt. NHL Municipal Medical College, Ahmedabad, India
Submission: April 05, 2024;Published: April 16, 2024

ISSN: 2576-8875 Volume10 Issue5
Abstract
Distal femur fractures are the most common injuries that have the potential for serious disability. It has a bimodal presentation affecting both elderly and young individuals. The patients classically have a history of road traffic accidents or falls. With proper diagnosis and timely treatment, it can be managed without future disability concerns. Here, we present a case of a 29-year-old male patient with a diagnosis of AO/OTA type C fracture.
Keywords: Femur fracture; Disability; Road traffic accident
Introduction
Fractures affecting the distal femur are very complex injuries that pose a challenge to every orthopaedic surgeon. These serious injuries have the potential to produce significant disability. Fractures of the distal femur accounted for 0.4% of all fractures [1]. It commonly occurs during high-velocity trauma in younger groups of patients and is frequently associated with other skeletal injuries. In contrast to this, elderly patients with severe osteopenia might sustain isolated distal femur fractures from trivial trauma. The treatment of distal femoral fractures in the last decade or two; has evolved from non-operative, conservative treatment to more aggressive, operative treatment [2]. The aim was to achieve faster bone healing and to allow early, active mobilisation of the patient and the associated joints, thereby minimising the side effects of joint stiffness and severe muscular atrophy encountered in the conservative treatments.
Clinical Presentation
A 29-year-old Indian male patient presented to the hospital with the chief complaint of left knee pain and swelling. The patient has a history of road traffic accident following which he started having these symptoms. On examination, the patient’s general condition was good. He was conscious and well-oriented to time, place and person. A nervous system examination revealed a normal Glass Glow Coma Scale (GCS) score. His pupils were bilaterally equal in size and diameter and reactive to light. Extraocular Movements (EOM) were normal. Muscle tone and strength of all 4 limbs were normal.
Diagnosis
Following X-rays and other required diagnostic tests, the patient was diagnosed with AO/OTA type 3C distal femur fracture.
Treatment
Standard anteroposterior and lateral X-rays were done. CT scan of the affected knee was done in the patient to identify intra-articular extensions of the fracture line. The patient was then classified as per AO Classification. If open fractures were encountered; thorough wash, sterile dressing, tetanus prophylaxis and antibiotics were given. Upper tibial skeletal traction was given in the patient with weights up to 3-5kg applied depending on the weight and build of the patient, and proximal displacement of the distal fracture segment. Plaster immobilisation in the patient in the form of a high aboveknee plaster slab was given. CT scan of the affected knee was done in the patient to identify intra-articular extensions of the fracture line. The patient was then classified as per AO Classification. The patient was electively posted for surgery following anaesthetic clearance.
Surgery was carried out at our tertiary care level 1 centre by one of the two senior surgeons in our unit. The patient was placed on a radiolucent table in the supine position. A single or triple bolster was used as and when required. The lateral approach, the Modified Swashbuckler approach or MIPO approach was used as deemed by the surgeon. First reduction was done with the use of k wire and clamps following which metaphyseal reduction was done and then appropriate size DFLP was selected and slid in a distal to proximal direction over the lateral aspect of the bone. A minimum of 4 screws were fixed on either side of the fracture. C arm fluoroscopy image was taken to check the fixation. Following this thorough irrigation was carried out. Drain put whenever necessary. Closure was done in layers and pressure dressing was applied above the knee brace.
In the immediate postoperative period, intravenous antibiotics were given to the patient for 5 days. A haemodynamic assessment of the patient was routinely carried out. 0.6mg subcutaneous Low Molecular Weight Heparin (LMWH) was given to prevent deep vein thrombosis. The drain was removed after 2 days. A sterile pressure dressing was carried out 6th hours after the operation and was followed at 1 and 7 postoperative days. Depending on the healing response, sutures were removed on the 12 - 14 postoperative days. The patient was encouraged to perform ankle toe mobilization and isometric quadriceps contractions 6 hours after the surgery.
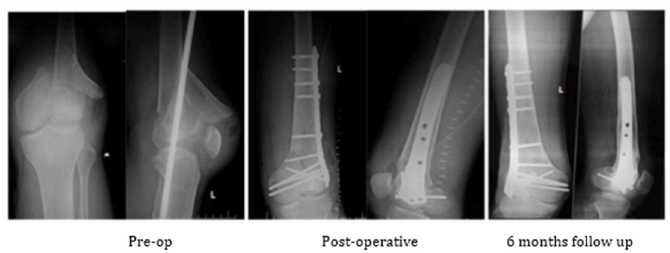
In the early phase (1-3 Weeks) active range of motion exercises were started on the 2nd day if reduction and fixation were satisfactory, if fixation was stable, with emphasis on knee extension, normal patellar mobility, control of oedema and pain. Quadriceps strengthening and hamstring stretching exercises were encouraged. Gentle hip and ankle mobilization exercises were continued. In the late phase (after 3 weeks), partial weight bearing was allowed. Full weight bearing was allowed after radiological evidence of healing. (6-12 weeks). The patient was followed up 2, 4, 8 and 24 weeks after surgery. Following that, they were advised to return for follow-up yearly. Neer’s score and Knee Society score were calculated along with radiographic assessment regularly (Figure 1).
Figure 1:
Discussion
The distal femur fractures include fractures of the supracondylar and intercondylar region of the distal femur. These are common injuries seen in young as well as elderly patients. The mechanism of injury includes both high-energy (road traffic accidents) and lowenergy mechanisms (falls). However, the most common mechanism of injury is direct trauma to a flexed knee (dashboard injuries in RTA) [3]. To avoid morbidity and mortality, proper diagnosis and treatment is needed. The treatment goals follow AO principles of anatomic reduction of the articular surface, restoration of limb alignment, length and rotation.
The distal femur ranges from the meta-diaphyseal junction to the articular surface of the knee [4]. Following fracture, different muscle groups play an important role in determining fracture position. Hamstrings and extensors shorten the fracture while the adductor magnus places the fracture into the varus position. These fractures are most commonly associated with soft tissue injuries which are difficult to diagnose. However, there is a difference of opinion regarding the timing of treatment of these concomitant injuries.
Ortho Trauma Association Classification [5]:
33A - Extra-articular
a) A1 - simple
b) A2 - metaphyseal wedge
c) A3 - metaphyseal complex
33B - Partial articular (a portion of the articular surface remains attached to the proximal shaft)
a) B1 - lateral condyle
b) B2 - medial condyle
c) B3 - coronal plane (Hoffa fragment)
33C - Complete articular (articular fragment separated from the shaft)
a) C1 – simple articular, simple metaphyseal
b) C2 – simple articular, metaphyseal comminution
c) C3 - metaphyseal and intra-articular comminution
The clinical presentation of such patients is non-specific: pain with weight-bearing, swelling and bruising, and deformity (knee looks out of place). The patient has a history of accidents or falls.
The mainstay of diagnosing fracture includes imaging. X-rays are the first step followed by a CT scan to plan treatment [6]. Contralateral femur radiographs can be taken for preoperative planning. If external fixation is to be done, then a CT is recommended after the procedure. CT Angiography is done in cases with decreased ipsilateral distal pulses.
Treatment options for distal femur fractures include: nonoperative
and operative [7]. Non-operative management includes
knee mobilisers, hinged knee braces and casts. These are reserved
for stable and minimally displaced fractures. Operative measures
include:
1) External fixation: measure for temporarily restoring and
stabilising limb length and alignment until soft tissue injuries
subside. Complications of this method include increased
infection risk, malunion, and stiffness.
2) Open reduction with internal fixation: can be done via 3
methods:
a) Blade plate and sliding barrel condylar plate [8] - for OTA
33 type A, but has bulky size
b) Condylar buttress plating [9] - for OTA type B fracture,
does not have a fixed angle device so it relies on friction between
bone-plate interface.
c) Locking plates - most commonly used and more superior.
Each screw has a fixed angle size thus, provides stability by
securing plates at multiple points.
3) Intramedullary nailing [10]: provides stability with
minimal construct and the least soft tissue and periosteum
disruption. It can be anterograde or retrograde nailing.
4) Bone cement and bone grafts: for stable fixation of
supracondylar distal femur fracture with severe osteoporosis.
Conclusion
The outcome of distal femoral fractures, like other major injuries, not only depends on bony reconstruction but also on soft tissue management. Early stable internal fixation of the fracture with meticulous soft tissue handling and immediate immobilization of the knee joint; maximises the chance for an optimal outcome after a distal femur fracture. Although the distal femur locking plate system offers several advantages in fracture management, a successful outcome requires careful pre-operative planning, precise use of biomechanical principles, and the use of the appropriate plate and screws combined with good surgical technique.
Ethical Statement
Being a case report study, there were no ethical issues and the IRB was notified about the topic and the case. Still, no formal permission was required as this was a record-based case report. Permission from the patient for the article has been acquired and ensured that their information or identity is not disclosed.
Conflicts of Interest
The authors declare no conflict of interest.
Funding and Sponsorship
None of the authors are financially interested in any of the products, devices, or drugs mentioned in this manuscript.
References
- Khan AM, Tang QO, Spicer D (2017) The epidemiology of adult distal femoral shaft fractures in a central London major trauma centre over five years. Open Orthop J 11(1): 1277-1291.
- Amin TK, Patel I, Patel MJ, Kazi MM, Kachhad K, et al. (2021) Evaluation of results of open reduction and internal fixation (ORIF) of fracture of distal end of femur with intra-articular extension. Malays Orthop J 15(3): 78-83.
- Hoit G, Khoshbin A, Poolman RW (2023) Distal femur fractures. Eidence-based orthopedics: Second Edition, pp. 595-599.
- Chang A, Breeland G, Black AC, Hubbard JB (2023) Anatomy, bony pelvis and lower limb: Femur. Stat Pearls.
- Stockton DJ. Distal femur fractures top 5 learning objectives 1) osteology & deforming forces 2) fracture classification 3) treatment options and considerations 4) surgical approaches 5) fixation options core curriculum v5.
- Leblanc KE, Herbert LM, Leblanc LL (2014) Hip fracture: diagnosis, treatment, and secondary prevention. Am Fam Physician 89(12): 945-951.
- Von Keudell A, Shoji K, Nasr M, Lucas R, Dolan R, et al. (2016) Treatment options for distal femur fractures. J Orthop Trauma 30: S25-27.
- Avate SA, Dalal S (2018) Prospective comparative study of different modalities of distal femoral fracture management. International Journal of Orthopaedics Sciences 4(3): 66-73.
- Petsatodis G, Chatzisymeon A, Antonarakos P, Givissis P, Papadopoulos P, et al. (2010) Condylar buttress plate versus fixed angle condylar blade plate versus dynamic condylar screw for supracondylar intra-articular distal femoral fractures. Journal of Orthopaedic Surgery 18(1): 35-38.
- Neradi D, Sodavarapu P, Jindal K, Kumar D, Kumar V, et al. (2022) Locked plating versus retrograde intramedullary nailing for distal femur fractures: a systematic review and meta-analysis. Archives of Bone and Joint Surgery 10(2): 141-152.
© 2024 Dev Desai. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






