- Submissions

Full Text
Orthopedic Research Online Journal
A Single, Same-Day Procedure Using Multiple PRP Formulations to Treat Complex Knee Pathologies. A Case Report
Peter A Everts1,2* and Luga Podesta3
1Chief Scientific Officer and Program Director Research & Educational Division Gulf Coast Biologics, Fort Myers, USA
2Professor Max-Planck University, Ortho Regen Group, Brazil
3Medical Director and Owner Regenerative Sports Medicine & Orthopedics, Naples, USA
*Corresponding author:Peter A Everts, Chief Scientific Officer and Program Director Research & Educational Division Gulf Coast Biologics, Fort Myers, USA
Submission: December 13, 2023;Published: December 20, 2023

ISSN: 2576-8875 Volume10 Issue4
Abstract
A broad range of musculoskeletal disorders (MSK) require tissue repair strategies, including osteoarthritis (OA), ligament, tendon, and soft tissue pathologies. Sports medicine and orthopedic practices have increasingly utilized autologous ortho biological cellular preparations to improve function, facilitate tissue repair, and reduce pain. Ortho biologic preparations include platelet-rich plasma (PRP), bone marrow concentrates, and adipose tissue concentrates, prepared at point-of-care.
Introduction
PRP ortho biological preparations are composed of a wide variety of cells, including platelet growth factors, cytokines, molecules, and signaling cell [1]. After being administered in specific diseased microenvironments, they can modulate and influence many other resident cells [2]. One of the most notable advantages of PRP is its autologous nature, with some devices presenting a variety of innovative and high-quality preparation methods [3]. As a non-autologous biologic, PRP applications are regarded as safe, with no known systemic adverse effects, other than pain and swelling following treatment.
A so-called “one-size-fits-all” and basic PRP preparation approach should be abandoned as a standard to treat MSK pathologies [4]. PRP variables and formulations, Neutrophil-Poor (NP-PRP) and Neutrophil-Rich PRP (NR-PRP) bioformulations, with varying platelet dosages should be employed based on pathoanatomic conditions and tissue types. Here we present a case study that illustrates the clinical feasibility of using multiple tissue specific PRP platelet dosing and bioformulation strategies simultaneously to treat a patient with multiple knee pathologies, in the same treatment session.
Case Report
A 61-year-old male (PE), with multiple right knee pathologies, following an active sport history at younger age, was treated in a specialized nonsurgical orthopedic sports medicine institution by a dual board-certified physician (LP). The MRI revealed: a complex posterior horn meniscus tear extending from articular surface to peripheral capsular margin; an intact medial collateral ligament with medially bowed with stripping of proximal tibial attachment, and diffusely thickened fibers; mild OA medial compartment with joint space narrowing; moderate diffuse chondromalacia anterior medial condyle; a mucoid degenerative, thickened, ACL. A personalized PRP treatment plan was created based on the above pathology findings.
Procedure preparation
Intake, with informed consent.
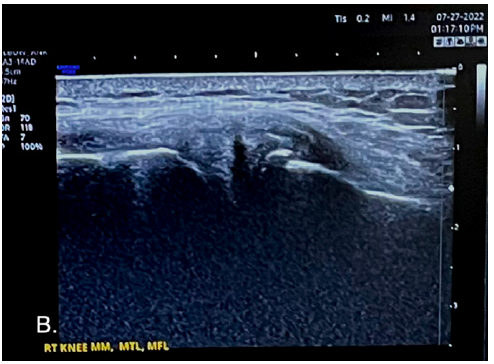
1. Ultrasound scanning of the knee joint structures (Figure 1, demonstrates the extruding medial meniscus tear and MCL).
Figure 1:Ultrasound image of an extruding medial meniscus from the right knee with a complex tear, with MCL laxity.
2. Following ultrasound scanning the number of
pathoanatomic injections, the relevant injection volumes, and
the individual PRP platelet dose and bioformulation were
determined. A total of 7, intra articular and soft tissue injections
were anticipated.
3. Baseline CBC analysis was performed. The baseline
platelet concentration was used to determine the total whole
blood volume to extract to prepare the various PRP injectates
and formulations; a total blood volume of 108ml was calculated
to be sufficient.
4. Regional right adductor canal and geniculate nerve blocks
were administered.
5. The peripheral anticubital vein was cannulated with a
17G NIPRO fistula needle, harvesting a total of 120ml sodium
citrate anticoagulated whole blood.
6. The blood was processed using two 60ml 2-spin PRP
devices (PurePRP-SP®, EmCyte Corporation, Fort Myers FL,
USA). Figure 2 is the aspect of both PRP devices, containing NRPRP
and NP-PRP formulations.
Figure 2:NP-PRP (A) and NR-PRP (B) preparations following a 2-spin centrifugation process (Pure-PRP-SP®, EmCyte Corporation, Fort Myers FL, USA).
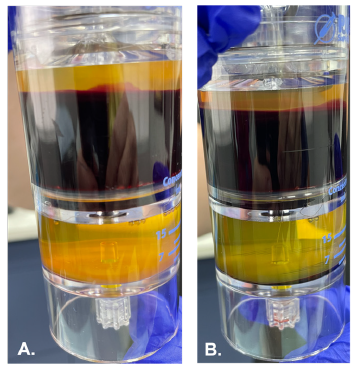
7. Final PRP processing steps produced 7ml of NR-PRP and 5ml of NP-PRP. PRP volumes were aseptically transferred in 4 injection syringes. Cellular validation details are shown in Table 1.
Table 1:CBC data from whole blood, NP-PRP, and NRPRP.

Treatment procedure
Following the nerve blocks, the patient was prepared for the individual injections. Ultrasound scanning preceded each individual injection to visualize the injection target and needle trajectory. The ultrasound probe was used in both short and long axis (when appropriate) during the entire PRP injection. After assessing the entry point, each skin entry point was prepared using aseptic precautions.
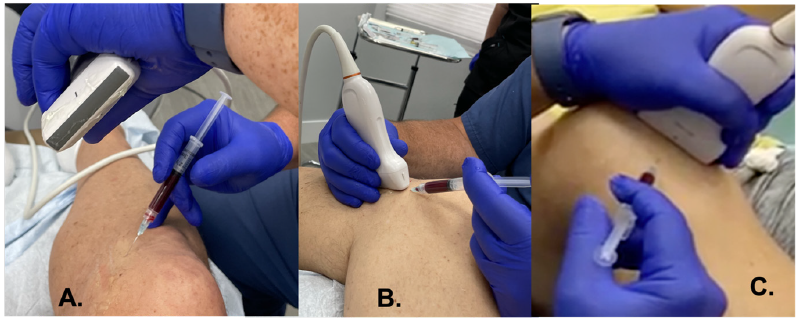
Knee injections (Figure 3)
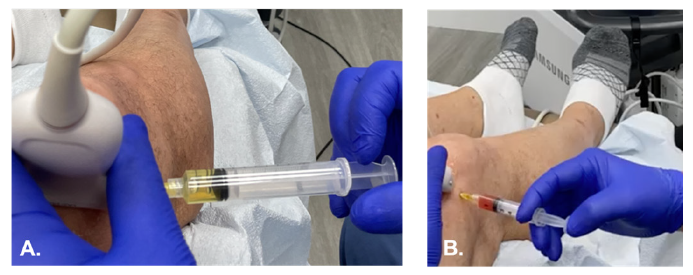
1. Right knee joint cavity: first 9ml of synovial fluid was extracted, the needle remained in situ and 4.5ml of NP-PRP was injected intra-articular and peri-articular synovial capsule (Figure 4A & 4B).
Figure 3:Schematic presentation of the 4-skin entry point PRP injections to inject 7 different tissue structures. 1: Intra articular NP-PRP; 2: medial meniscus, meniscus femoral ligament, and meniscus tibial ligament; 3: MCL; 4: ACL.
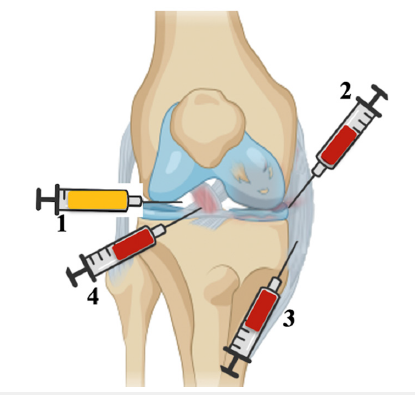
Figure 4:Supra-patellar technique for effusion evacuation (A), followed by NP-PRP injection (B).
2. The medial meniscus tear, meniscus femoral ligament,
and meniscus tibial ligament were injected with a total of 2.4ml
NR-PRP.
3. The medial collateral ligament was injected with 2.1ml of
NR-PRP.
4. Both ACL insertions were injected with a total of 2.0ml
NR-PRP.
A total of 7, articular and soft tissue, injections (Figure 5) and a synovial fluid extraction were performed under direct ultrasound imaging, using 4 skin entry points. The injection volumes of the various tissue structures were meticulously recorded to precisely calculate the delivered platelet dose per tissue structure. The entire treatment procedure went without any complications, or adverse events.
Figure 5:Representation of soft tissue injections.
Post treatment care
A heated gel pack was applied to the knee joint immediately following the procedure for 15 minutes to provide procedural pain relief. A medial unloader brace (Ösur One X Medial Unloader Brace®, Irvine CA, USA) was fitted to be worn for 14 days. A heat pack protocol was used four to six times per day, for 15 minutes at a minimum interval of two hours. As a result, significant pain relief was achieved. No NSAIDs or opioids were permitted, only Tylenol 500mg if necessary.
Post treatment follow up
Figure 6:Evolution of the meniscus and MCL healing following ortho biological PRP therapy, at follow up after 14-months. The middle image is after 11 weeks of the intervention.
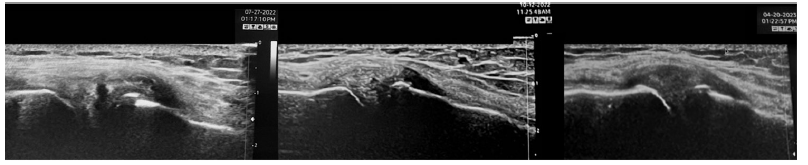
After 11 weeks following the ortho biological intervention, the patient underwent a functional and ultrasound examination. An evaluation of the ultrasound image before and after the procedure revealed that the meniscus tear is almost completely healed, with a better collagen organization from the MCL. At fourteen-month follow-up found the patient to be relatively symptom free and with good function, although inflammatory markers will gradually rise, since intra-articular PRP applications are not a cure-all treatment for osteoarthritis. The decision was made to inject a maintenance dose of NR-PRP. In Figure 6, a comparison of the pre-PRP ortho biological treatment with the 14 months post PRP ortho biological treatment, including the 9-month post treatment image.
Discussion
Within the field of ortho biological procedures, PRP therapies have become an important autologous biological therapeutical instrument, as devices and preparation protocols have evolved greatly during the last decades. Specifically, an unyielding awareness of the wide variety of ortho biologic PRP products on the market, avoiding delusion of a “one size fits all” approach with a single type of PRP applicable to all patients has contributed immensely to more consistent positive outcomes.
PRP treatments are generally proven effective since they assist the body’s innate healing abilities in regenerating peripheral tissues that are degenerative or defective. A multidimensional, tissue-specific repair approach, incorporating platelet dosing and bioformulation strategies, can optimize the full complexity of the natural healing response through biological cell signaling in all types of MSK tissue structures and microenvironments, ultimately leading to consistent clinical outcomes because the pathoanatomic structures have been functionally restored.
References
- Everts P, Onishi K, Jayaram P, Lana JF, Mautner K (2020) Platelet-rich plasma: New performance understandings and therapeutic considerations in 2020. Int J Mol Sci 21(20): 7794.
- Andia I, Maffulli N (2019) New biotechnologies for musculoskeletal injuries. The Surgeon 17(4): 244-255.
- Magalon J, Brandin T, Francois P, Degioanni C, Lucille DM, et al. (2021) Technical and biological review of authorized medical devices for platelets-rich plasma preparation in the field of regenerative medicine. Platelets 32(2): 200-208.
- Everts PA, Mazzola T, Mautner K, Randelli PS, Podesta L (2022) Modifying ortho biological PRP therapies are imperative for the advancement of treatment outcomes in musculoskeletal pathologies. Biomedicines 10(11): 2933.
© 2023 Peter A Everts. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






