- Submissions

Full Text
Orthopedic Research Online Journal
Open Elbow Fracture Dislocation with Ipsilateral Shoulder Fracture Dislocation: A Case Report and Literature Review
Albert Tang*, Hassan Abbasi and Christopher Jenkins
Department of Orthopaedics, Manchester Foundation Trust, United Kingdom
*Corresponding author:Albert Tang, Department of Orthopaedics, Manchester Foundation Trust, United Kingdom
Submission: October 06, 2023;Published: October 17, 2023

ISSN: 2576-8875 Volume10 Issue4
Abstract
Ipsilateral fracture dislocation of the shoulder and elbow is a rare injury. This is usually caused by high-energy trauma injurie such as motor vehicle accidents or falls from height. We reported a case of a 64-year-old female with an ipsilateral fracture dislocation of the shoulder and elbow. A positive outcome was achieved through closed reduction of the elbow joint followed by the shoulder joint, in combination with internal fixation. The purpose of this case report is to describe an extremely rare injury and to emphasise the importance of maintaining a high index of suspicion in such cases.
Case Presentation
A 64-year-old female presented to the emergency department after sustaining injuries to her left shoulder and elbow. The patient tripped over her own feet whilst under the influence of alcohol. The patient sustained an ipsilateral fracture dislocation of the shoulder and elbow. It was noted that there was a 3-4cm wound on the anteromedial aspect of her left elbow. There was also reported no sensation in the ulnar nerve distribution.
Investigations
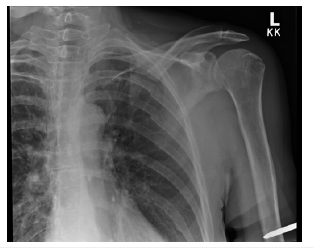
1. X-rays of the left shoulder and elbow (at initial presentation): left shoulder dislocation with fractures at the proximal humerus (Figure 1); left elbow dislocation with fractures seen at the radial head, ulnar coronoid process (Figure 2)
Figure 1:

Figure 2:

2. CT of the left elbow (day 2 post-presentation) - confirmed radial head and notch, ulnar coronoid process fractures, elbow dislocation is seen (Figure 3 & 4)
Figure 3:

Figure 4:
Treatment
The patient was initially managed in the emergency department. The elbow dislocation was successfully reduced under conscious sedation. The shoulder remained dislocated despite numerous manipulation attempts. The elbow wound was thoroughly washed with normal saline and dressed appropriately. The patient was placed in an above elbow backslab for the elbow injury and a collar and cuff for the shoulder injury. The patient reported no sensation in the ulnar nerve distribution.
The patient was subsequently taken to theatre two days postinjury for a wound washout and closure for the left elbow open wound and manipulation under anaesthesia of the left shoulder under general anaesthesia. The elbow wound was thoroughly washed with six litres of normal saline and betadine. The left shoulder dislocation was reduced and deemed to be stable postreduction. The patient was placed in an above elbow backslab for the elbow injury and a collar and cuff for the shoulder injury.
CT of the left elbow was done one day post-surgery (day three post-injury) for surgical planning. The images revealed the elbow had re-dislocated. The patient was taken back to theatre on that day for manipulation under general anaesthesia and application of an external fixator. Two pins were applied in the humerus and ulna respectively. The shoulder joint remained congruent throughout. The patient continued to report no sensation in the ulnar nerve distribution.
The patient returned to theatre thirteen days later for removal of external fixator, open reduction and internal fixation with radial head replacement, lateral ligament repair and ulnar nerve decompression. The patient was discharged twenty-three days post-injury.
Outcome and Follow-Up
The patient was reviewed in the fracture clinic two weeks postsurgery. The backslab was removed and commenced on elbow range of motion exercises with ligament protection instruction. The patient continued to report no sensation in the ulnar nerve distribution. The patient is still under regular review and a nerve conduction study is planned should the sensation do not return.
Discussion
Joint dislocations are very frequent injuries with the incidence of shoulder dislocation and elbow dislocation reported at 24 and 5.2 per 100,000 person-years respectively [1]. However, Ipsilateral dislocation of the shoulder and elbow is a rare injury with a handful of cases being reported in the literature in the past thirty years. These are usually caused by high-energy trauma injuries such as motor vehicle accidents or falls from height. Ipsilateral fracture dislocation of the shoulder and elbow is an even rarer injury. We were only able to identify one previous case in our literature search through PubMed and Google Scholar. Behr et al. [2] reported a case of ipsilateral fracture dislocation of the shoulder and elbow. They concluded that successful outcome generally occurs with closed reduction of elbow dislocation followed by shoulder dislocation.
They added closed reduction of the dislocations in conjunction with appropriate fracture management can result in a positive outcome. It is important to maintain a high index of suspicion of concomitant injuries [3].
Conclusion
Ipsilateral fracture dislocation of the shoulder and elbow is a rare injury. A positive outcome can be achieved through closed reduction of the elbow joint followed by the shoulder joint, in combination with internal fixation. It is important for clinicians to maintain a high index of suspicion of concomitant injuries.
References
- Prada C, Romero L, Espinosa A (2019) Ipsilateral elbow and shoulder dislocation: a case report. J of Shoulder and Elbow Surgery 28(7): 232-237.
- Behr I, Blint A, Trenhaile S (2013) Ipsilateral fracture dislocation of the shoulder and elbow: A case report and literature review. J Clin Orthop Trauma 4(4): 204-209.
- Meena S, Saini P, Rustagi G, Sharma G (2012) Ipsilateral Shoulder and Elbow Dislocation: A Case Report. Malaysian Orthopaedic Journal 6(1): 43-45.
© 2023 Albert Tang. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






