- Submissions

Full Text
Orthopedic Research Online Journal
Fracture Related Infections in Closed Trauma; Current Clinical and Microbiological Profile
Ateaze Chrisantus Formelah1*, Guifo Marc-Leroy1, Kikah Ndifor Ernest1, Tsiagadigui Jean Gustave1, Muluem Olivier Kennedy1, Ngo Yamben Marie Ange1, Ibrahima Farikou1 and Gonsu Kamga Hortense2
1Department of surgery and specialties, Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Cameroon
2Department of Microbiology, Hematology, Parasitology and Infectious Disease, Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Cameroon
*Corresponding author:Ateaze Chrisantus Formelah, Department of surgery and specialties, Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Cameroon
Submission: June 26, 2023;Published: July 11, 2023

ISSN: 2576-8875 Volume10 Issue4
Abstract
Background: Fracture Related Infection (FRI) in closed trauma here is considered as any deep or organ/space surgical site infection and/or osteomyelitis which occurs following an internal fixation of a closed fracture. FRI in closed trauma is a serious and invalidating illness characterised by a high rate of treatment failures and often requires long periods of treatment and hospital admission, leading to temporary impairment and at times long lasting disability or even permanent handicaps. The present study was realised to determine the epidemiological and susceptibility profile of bacterial isolates of FRI in closed trauma in our milieu.
Method: A prospective cohort study was carried out from November 2020 to May 2021 in four reference hospitals of Yaoundé. All patients diagnosed with FRI in closed trauma amongst fractured cases treated by internal fixation were recruited, socio-clinical information was taken, and clinical specimens were collected and cultured in routine culture media. The organisms isolated were identified by routine standard procedures. Antimicrobial susceptibility testing was done by Kirby-Bauer’s disc diffusion method and the results interpreted using guidelines of the « comité de l’antibiogramme de la société française de microbiologie (CASFM) »
Results: Out of the 120 patients followed up, 19 (15.83%) developed infection. The modal age was 20-40 (57.9%). The commonest bones infected were the femur (42.11%), and tibia (36.84%). Highest osteosynthesis involved were plate and screw (73.3%) and reamed intramedullary nailing (26.8%). Predisposing factors were long time lapse between trauma and surgery and scarification. Out of 19 samples, 17 yielded positive culture giving rise to 6 bacteria isolates. Thirteen samples (76.5%) were monobacterial while four (23.5%) were polybacterial. The most predominant species was Staphylococcus aureus (52.4%), followed by Enterobacter cloacae (19.0%), Escherichia coli (9.5%), and Klebsiella pneumonia (9.5%). The Gram-positive organisms showed good sensitivity to Vancomycine (81.8%), Clindamycine (72.7%), Gentamycine, Rifampicine and Fusidic acid (63.6%) and to a lesser extend Nitroflurantoine and Nitilmycine (54.5%).
Conclusion: The bacteria flora of FRI in closed trauma is dominated by nosocomial germs, which are developing resistances to most frequently prescribed antibiotics in our setting, thus emphasizing on hygiene and targeted antibiotherapy.
Keywords:Fracture related infections in closed trauma; Microbiological profile; Antimicrobial susceptibility
Introduction
Fracture Related Infection (FRI) is one of the most challenging musculoskeletal complications in trauma surgery. Currently estimating the impact of FRI has been hampered by the lack of a clear definition [1]. Fracture related infection in closed trauma here will be considered as any deep or organ/space surgical site infection and/or osteomyelitis which occurs following an internal fixation of a closed fracture. Osteomyelitis is an infection of bony tissue which could either be due to haematogenous origin, local spread from surrounding infected soft tissues, or direct inoculation of germs following trauma (open fractures or bone surgery). Fracture related infection implies a serious complication which prolongs the treatment and considerably increases the disability of the patient by leading to amputations and kidney failure. The operative fixation of skeletal fractures can be highly complex due to the unpredictable nature of the bone damage, the multitude of concomitant injuries that may need to be considered and the frequency of life-threatening situations in emergency care. One of the most feared and challenging complications in the treatment of musculoskeletal trauma patients is Infection After Fracture Fixation (IAFF), which can delay healing, lead to permanent functional loss, or even amputation of the affected limb [2].
FRI in closed trauma management frequently involves prolonged hospital stay, rehabilitation, repeated operations and the extensive use of specialized investigation and treatment. As a result, patients with FRI in closed trauma have high morbidity rates and are less likely to return to duty. The increasingly frequent use of internal fixation and the emergence of antibiotic resistant microorganisms have exacerbated this problem [3].
Materials and Methods
We carried out a cross sectional descriptive study from November 2020 to May 2021 (6 months) in four reference hospitals of Yaoundé. All closed fractured patients who developed clinical signs of infection after internal fracture fixation i.e., wound discharge, fever, local inflammation or radiological infection signs were included, socio-clinical information was taken and clinical specimens like pus, pus swaps, bone marrow contents and bone sequestrum were collected and sent to the Bacteriology Laboratory of Yaoundé University Teaching Hospital (YUTH) for analysis. The samples were cultured aerobically in Blood, Mannitol salt and MacConkey agar plates. Quality control of the media was done by verifying dates of expiration and the ensuring the absence of growth before usage. The organisms isolated were identified by routine standard operative procedures. Antimicrobial susceptibility testing was done by Kirby-Bauer’s disc diffusion method. Antibiotics tested included Ampicillin (10μg), Oxacillin (5μg), Ticarcilline (75μg), Piperacillin (30μg), Ticarcillin/clavulanic acid (75/10μg), Piperacilline/tazobactam (30/6μg), Amoxicillin/clavulanic acid (20/10μg), Cefuroxime (30μg), Cefotaxime (30μg), Ceftazidime (30μg), Imipenem (10μg), Vancomycin(30μg), Tobramycin (10μg), Gentamicin (10μg), Amikacin (30μg), Ciprofloxacin (5μg), Levofloxacin (5μg), Erythromycin (5μg), Lincomycin (15μg), Cotrimoxazole (1.25μg /23.75μg), Linezolid (30μg), Rifampicin (30μg), Flucidic acid (10μg). and the results interpreted using the CASFM guidelines. Data obtained was entered on Excel 2016 and analyzed using the statistical software SPSS version 24.0. The results were presented in figures and tables.
Results
One hundred and twenty patients were followed up to detect cases of infection. Nineteen (15.83%) of the patients developed infections during their follow up. This incidence was predominant among males with 13 cases (68.4%). The ages of infected patients ranged between 10 and 63 years and the most represented age group was 20-40 with 11 cases (57.9%), followed by 40-60 with 5 cases (26.3%) and 60-80 with 2 cases (10.5%). The mean age was 38.1±14.2 years. Infections mostly occurred in patients who sustained their injury on the street, n=17 (98%). 47.4% of patients who were referred from other health services incurred infection and 31.6% of patients who came from traditional healers ended up with infections, including three patients who had scarifications. The femur was the highest bone involved in infections (42.11%), followed by the tibia (36.84%). Plate and screw were the highest osteosynthesis technique incriminated in infections, n=14 (73.7%), followed by reamed intramedullary nailing n=5 (26.8%). There was a direct relationship between time lapse between trauma and surgery and the risk of infections, as the P value (0.00001) is statistically significant. Surgical site inflammation occurred in 15.8% of operated patients and in all the infected patients..
Surgical site inflammation and pus drainage from the wound occurred in all the infected patient (100%). Wound fistula and wound healing abnormalities occurred in 89.5% of infected patients. There was pain and loss of function in 94.7% of infected patients. We had hematoma on the surgical site in 31.6% of the infected patients.
Out of the 19 cases of infection, 15 (78.9%) were delayed infections (after 15 days). Early infections occurred in 4 patients (21.1%). No case of late infection was detected. All infected patients benefited from surgical debridement of the infected wound, with implant removal in 73.7%. followed by implant replacement in 63.2%.
Out of the 19 samples analyzed, 17 (89.5%) gave positive culture results with isolation of 6 germs. Overall, 76.5% of the samples were monobacterial while 23.5% were polybacterial. Gram positive cocci were the most common bacteria isolated (57.2%), with Staphylococcus aureus being the most predominant species (52.4%), followed by Enterococcus casseliflavus (4.8%). Gram negative bacilli were present in 42.8% of cases, with Enterobacter cloacae being the predominant species (19.0%), followed by Escherichia coli (9.5%), Klebsiella pneumonia (9.5%) and Klebsiella ozaenae (4.8%) (Table 1).
Table 1:Different bacteria isolated.

Most of the strains of Staphylococcus aureus were sensitive to Vancomycine (81.8%), Clindamycine (72.7%), Gentamycine, Rifampicine and Fusidic acid (63.6%), Nitroflurantoine and Nitilmycine (54.5%). They had a low sensitivity to frequently used prophylactic antibiotics such as cephalosporines, beta lactamase inhibitors and quinolones.
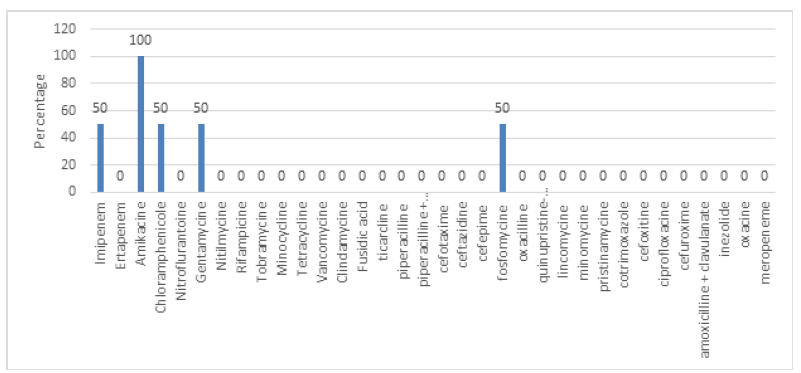
All the isolates of Escherichia coli were sensitive to Amikacine, Piperacilline + Tazobactam, Fosfomycine and Cotrimoxazole. Half of the isolates were sensitive to Imipenem and Meropenem. All the isolates of Klebsiella pneumoniae were sensitive to Amikacine. Half of them were sensitive to Imipeneme, Chloramphenicole, Gentamycine and Fosfomycine. All the isolates of Enterobacter cloacae were sensitive to Amikacine. A majority was sensitive to Imipeneme, and half was sensitive to Ertapeneme. They had a low sensitivity to other antibiotics (Figure 1-3).
Figure 1:Antimicrobial sensitivity pattern of Staphylococcus aureus.
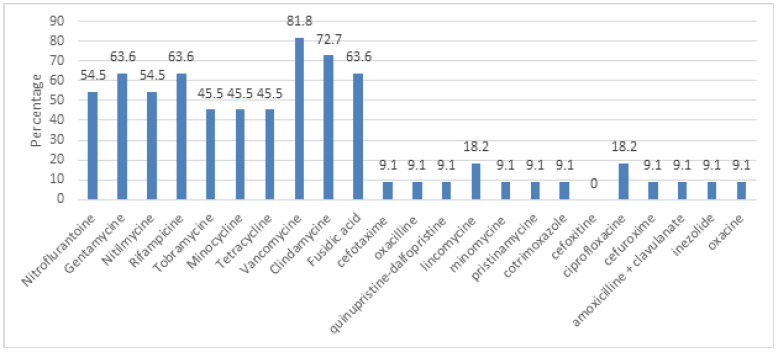
Figure 2:Antimicrobial sensitivity pattern of Escherichia coli.
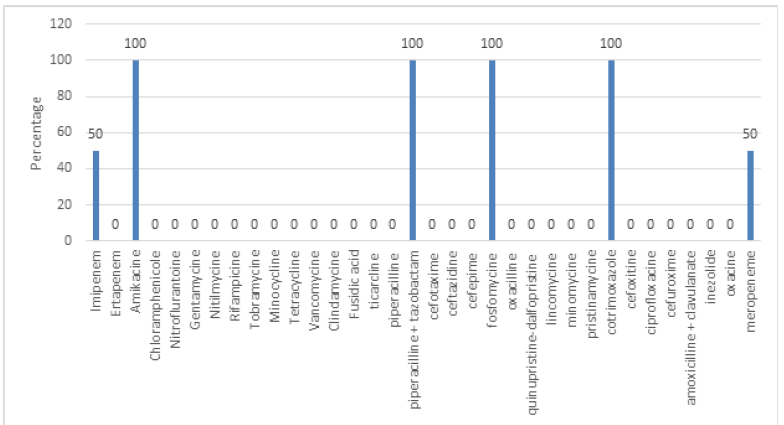
Figure 3:Antimicrobial sensitivity pattern of Klebsiela pneumoniae.
Discussion
Clinical Profile
The incidence of fracture related infections in closed trauma was 15.83%, predominant among males (68.4%) (with a sex ratio of 4.3:2 and in the age groups between 20-40 (57.9%) and 40-60 (26.3%); the mean age being 38.1±14.2 years. This high predominance of the male gender and the youthful age group could be due to the greater likelihood of high-speed trauma and compound fractures in this population group in relation with their daily activities.
In total, 31.6% of patients who came from traditional healers ended up with infections, including three patients who had scarifications. This could be attributed to the delay in management of these patients and scarification on the fractured limb which increasing the chances of infection in such patients after surgery. These results are similar to those obtained in a study carried out in Cameroon in 2005 which reported a case of osteomyelitis in a contusion that was traditionally treated with scarification as a closed fracture [4].
The femur was the highest bone involved in infections accounting for 8 cases (42.11%). These results do not correlate with those obtained from studies conducted in Cameroon in 2005 and 2017 [3,4] in which the tibia was reported as the highest bone involved in osteomyelitis (34.8%) and post-traumatic osteomyelitis (48.4%). Another study conducted in Mali in 2008 [5] reported the tibia as the most frequent (38.03%) bone in lower limb osteomyelitis followed by the femur (35.21%). This difference can be attributed to the fact that the above-mentioned studies included non-traumatic osteomyelitis and osteomyelitis following open fractures which are very frequent in the tibia. Nevertheless, our results correlate with those obtained from a study carried out in India in 2020 [6] which reported the femur having the highest frequency of chronic osteomyelitis (38%), followed by the tibia (36%). The increased soft tissue manipulation in the operative treatment of femoral fractures could also be attributed to the greater chances of infection.
Plate and screw were the highest osteosynthesis technique incriminated in infections, making up 14 (73.7%) of the infected cases, followed by reamed intramedullary nailing which accounted for 5 (26.8%) of the infected cases. These results are similar to those obtained in a study carried out in Norway in 1978 [7] which reported plating (48%) as the most frequent type of osteosynthesis involved in osteomyelitis, followed by intramedullary nailing (22%). These results equally correlate with the literature, as periosteal stripping and reaming of the medullary canal alter blood supply to bone tissue, thereby favouring the onset of infections [8,9].
All infected patients benefited from surgical debridement of the infected wound, with implant removal in 73.7% and implant replacement in 63.2%. This correlates with the literature which states that the most important considerations in late infection with and without consolidation of the fracture are removal of the remaining fracture fixation device/foreign bodies, radical debridement of all involved bone (sequesters) and soft tissue, long term antimicrobial therapy (normally 6 weeks) and reconstruction of the soft tissue envelope [2].
Culture results
In our samples, 89.5% gave positive culture results and enabled the isolation of a total of 6 germs, giving an average of 0.32 bacteria per sample. Overall, 76.5% of the samples were mono-bacterial while 23.5% were poly-bacterial. Our results are similar to those reported in a similar study done in Morocco, in 2007, concerning 85 cases of osteomyelitis in which the average number of isolates per sample was 1.4 and 63.5% were mono-microbial against 36.5% of the cases which were poly-microbial and a similar study conducted in India which reported that mono-microbial flora (69%) were more common than poly-microbial flora (16%) [6,10]. These results are equally similar to those obtained in a study in India in 2020 [6] which reported that out of 100 sample studied, in 85 (85%) the culture was positive, while in 15 (15%) the culture was negative. The low rate of negative cultures in our study could be justified by the fact that many of our cases were early and delayed infections. More negative culture results are often reported in late infections since it often involves germs (like slow growing bacteria) that have adapted diverse mechanisms to survive in the host while evading the immune system [11].
Gram positive cocci were the most common bacteria isolated (57.2%), with Staphylococcus aureus being the most predominant organism (52.4%), followed by Enterococcus casseliflavus (4.8%). These results correlate with literature which states that Staphylococcus aureus causes the majority of osteosynthetic associated infection cases [12], as well as a study conducted in India in 2013 [6] where S. aureus was the most common grampositive cocci. They however differ from those obtained in a study in Cameroon in 2017 [2] on post traumatic osteomyelitis, which reported that Gram negative bacteria were the most predominant isolates (81%). Enterobacteriae represented 62.5% of the isolates followed by non-fermenting Gram-negative bacilli (18.8%) and Gram-positive cocci (18.8%). The most predominant species was Escherichia coli with a prevalence of 29%, followed by Staphylococcus aureus, Pseudomonas aeruginosa and Klebsiella pneumoniae (all 22.6%)
Staphylococcus aureus is the most common pathogens of all types of osteomyelitis. Reasons for this include surface receptors for human extracellular protein fibronectin, fibrinogen, collagen and sialoprotein II, the production of staphylococci toxins that enhance virulence, the formation of biofilms and frequent colonization of the skin and nares [13]. Antonia and al reported an incidence of 25% of MRSA infections in open fracture population and this prevalence has been increasing [14].
Gram negative bacilli were present in 42.8% of cases, with Enterobacter cloacae being the predominant organism (19.0%), followed by Escherichia coli (9.5%), Klebsiella pneumonia (9.5%) and Klebsiella ozaenae (4.8%). This corresponds to the profile of nosocomial germs showing that nosocomial germs play a major role in fracture related infections in closed trauma in our context. This correlates with most studies as Staphylococcus aureus is often reported to be the first causative agent [6,15].
Sensitivity testing
Most of the strains of Staphylococcus aureus were sensitive to Vancomycine (81.8%), Clindamycine (72.7%), Gentamycine, Rifampicine and Fusidic acid (63.6%), Nitroflurantoine and Nitilmycine (54.5%). They had a low sensitivity to cephalosporines, beta lactamase inhibitors and quinolones. These findings are different from those obtained in the study carried out in Morocco 2014 [10] which reported a good (87-100%) sensitivity of all the Staphylococcus aureus strains to most antibiotics except for Penicillin G. All their strains were Methicillin sensitive and Vancomycin sensitive. The difference could be explained by the fact that they mostly had community acquired germs whereas most of the germs isolated in our study are nosocomial germs. The studies carried out in India in 2013 [16] and 2017 [17] had comparable results with ours. They showed reduced sensitivity (less than 50%) to quinolones, aminoglycosides, Cotrimoxazole and to Cephalosporines.
All the isolates of Escherichia coli were sensitive to Amikacine, Piperacilline + Tazobactam, Fosfomycine and Cotrimoxazole. Half of the isolates were sensitive to Imipenem and Meropenem. These results are similar to those gotten in a study done in India in 2020 which revealed that half of the isolates of E. coli were sensitive to Amikacine (53.33%) and 66.67% were sensitive to Imipenem [6].
All the isolates of Klebsiella pneumoniae were sensitive to Amikacine. Half of them were sensitive to Imipeneme, Chloramphenicole, Gentamycine and Fosfomycine. These results are similar to those obtained in a study carried out in Mali in 2010 [18] which reported that all the isolates of K. pneumoniae were sensitive to Amikacine and half of them to Gentamycine in bone and joint infection.
All the isolates of Enterobacter cloacae were sensitive to Amikacine. A majority was sensitive to Imipeneme, and half was sensitive to Ertapeneme. They had a low sensitivity to other antibiotics. It is observed here that most of the germs involved on FRI in closed trauma in our context are either resistant or have a low sensitivity pattern to the routinely used prophylactic antibiotics. There is therefore a need to establish a more appropriate protocol of post-surgical prophylactic antibiotherapy in closed fractures.
Conclusion
Traditional treatment of closed fractures with scarification exposes the patient to infections if they end up undergoing osteosynthesis, with plate and screw being the osteosynthesis technique more prone to infections. The bacterial flora of fracture related infections in closed trauma in our setting is dominated by Staphylococcus aureus and nosocomial Gram-negative bacilli and these bacteria are developing resistances to most of the routinely used antibiotics. Appropriate implementation of pharmacological and non-pharmacological measures in prevention and management of FRI will bring a lot of improvement.
Acknowledgement
None
Ethical Considerations
The manuscript has received approval from the ethical committee of the Faculty of Medicine and biomedical sciences of the University of Yaoundé I, Cameroon
References
- Metsemakers Wj, Morgenstern M, McNally MA, Moriarty TF, McFadyen I, et al. (2018) Fracture-related infection: A consensus on definition from an international expert group. Injury 49(3): 505-510.
- Metsemakersa WJ, Kuehlb R, Moriartyc TF, Richardsc RG, Verhofstadd M, et al. (2016) Morgenstern Infection after fracture fixation current surgical and microbiological concepts. 49(3): 511-522.
- Handy ED, Manfo AA, Gonsu KH, Essi MJ, Ngo Nonga B, et al. (2017) Clinical and microbiological profile of post-traumatic osteomyelitis in tertiary hospital in Yaoundé - Cameroon. 3(3): 1180-1184.
- Ibrahima F, Pisoh-Tagyin C, Abolo-Mbenti L, Sosso MA. Eimo Malonga E (2005) Assessment of bone and joint infections in Yaoundé. Experience of the National Center for the Rehabilitation of the Handicapped in Yaoundé (Etoug-Ebé).
- Oumar AD, Abdou AT. Epidemio-clinical study of osteitis of the lower limb in the orthopedic and traumatological surgery department of the CHU Gabriel Toure.
- Suguneswari G, Singh AH, Basu R (2013) Bacteriological profile of osteomyelitis in a tertiary care hospital at Visakhapatnam, Andhra Pradesh. Int J Cur Res Rev 552-558.
- Rolf Hagen (1978) Osteomyelitis after operative fracture treatment a report of 62 cases treated with radical surgery and lincomycin (Lincocin). Acta Orthopaedica Scandinavica 49(6): 542-548.
- Eijer H, Hauke C, Arens S, Printzen G, Schlegel U, et al. (2001) PC-Fix and local infection resistance - Influence of implant design on postoperative infection development, clinical and experimental results. Injury 32: 38-43.
- Melcher GA, Claudi B, Schlegel U, Perren SM, Printzen G, et al. (1994) Influence of type of medullary nail on the development of local infection. An experimental study of solid and slotted nails in rabbits. J Bone Joint Surg Br 76(6): 955-959.
- Elouennass M, El Hamzaoui S, Frikh M, Zrara A, Chagar B, et al. (2007) Bacteriological aspects of osteitis in a university hospital. Med Mal Infect 37(12): 802-808.
- Zimmerli W. Bone and joint infections.
- Christian Fang, Tak-Man W, Tak-Wing L, Kelvin K, Samson SY, et al. (2017) Infection after fracture osteosynthesis - Part I Pathogenesis, diagnosis and classification. Journal of Orthopaedic Surgery 25(1): 1-13.
- Haas DW, McAndrew MP (1996) Bacterial osteomyelitis in adults: Evolving considerations in diagnosis and treatment. The American Journal of Medicine 101(5): 550-561.
- Chen J (2017) Comparison-of-the-curative-effects-of-pfna-and-dhs-fixation-in-treating-intertrochanteric-fractures-in-elderly-patients. Biomed Res 28(6): 2717-2723.
- Coudane H, Gérard A, George T, Claudot F, Gervaise A (2011) Osté Encycl. Medico-Chirurgical, pp. 1-14.
- Zimmerli W, Flckiger U (2004) Course forms and microbiology of bacterial osteomyelitis. The Orthopede 33: 267-272
- Mader JT, Cripps MW, Calhoun JH (1999) Adult posttraumatic osteomyelitis of the tibia. Clinical Orthopedics and Related Research (360): 14-21.
- Ouma D (2010) Study of the sensitivity to antibiotics of germs isolated from infections. Hospital and University Center CHU Gabriel Touré.
© 2023 Ateaze Chrisantus Formelah. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






